Quest for the right Drug
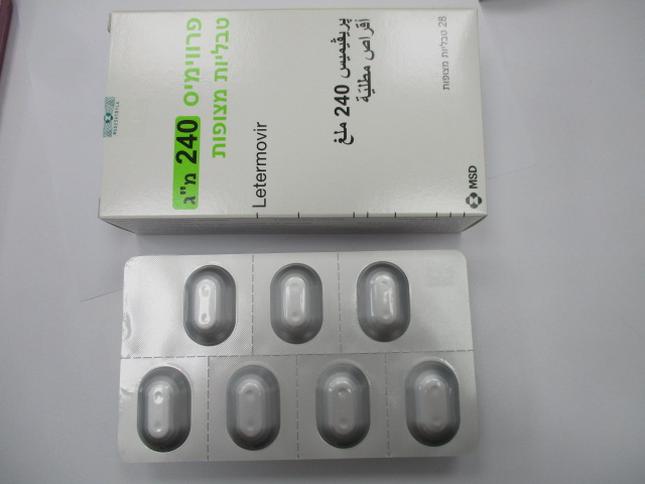
פרווימיס 240 מ"ג טבליות מצופות PREVYMIS 240 MG FILM-COATED TABLETS (LETERMOVIR)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Interactions : אינטראקציות
4.5 Interaction with other medicinal products and other forms of interaction General information about differences in exposure between different letermovir treatment regimens -The estimated letermovir plasma exposure is different depending on the dose regimen used (see table in section 5.2). Therefore, the clinical consequences of drug interactions for letermovir will be dependent on whether or not letermovir is combined with cyclosporine. -The combination of cyclosporine and letermovir may lead to more marked or additional effects on concomitant medicinal products as compared to letermovir alone (see Table 1). Effect of other medicinal products on letermovir The elimination pathways of letermovir in vivo are biliary excretion and glucuronidation. The relative importance of these pathways is unknown. Both elimination pathways involve active uptake into the hepatocyte through the hepatic uptake transporters OATP1B1/ 3. After uptake, glucuronidation of letermovir is mediated by UGT1A1 and 3. Letermovir also appears to be subject to P-gp and BCRP mediated efflux in the liver and intestine (see section 5.2). Inducers of drug metabolizing enzymes or transporters Co-administration of PREVYMIS (with or without cyclosporine) with strong and moderate inducers of transporters (e.g., P-gp) and/or enzymes (e.g., UGTs) is not recommended, as it may lead to subtherapeutic letermovir exposure (see Table 1). -Examples of strong inducers include rifampicin, phenytoin, carbamazepine, St. John’s wort (Hypericum perforatum), rifabutin and phenobarbital. -Examples of moderate inducers include thioridazine, modafinil, ritonavir, lopinavir, efavirenz and etravirine. Rifampicin co-administration resulted in an initial increase in letermovir plasma concentrations (due to OATP1B1/3 and/or P-gp inhibition) that is not clinically relevant, followed by clinically relevant decreases in letermovir plasma concentrations (due to induction of P-gp/UGT) with continued rifampicin co-administration (see Table 1). Additional effects of other products on letermovir relevant when combined with cyclosporine Inhibitors of OATP1B1 or 3 Co-administration of PREVYMIS with medicinal products that are inhibitors of OATP1B1/3 transporters may result in increased letermovir plasma concentrations. If PREVYMIS is co- administered with cyclosporine (a potent OATP1B1/3 inhibitor), the recommended dose of PREVYMIS is 240 mg once daily (see Table 1 and sections 4.2 and 5.2). Caution is advised if other OATP1B1/3 inhibitors are added to letermovir combined with cyclosporine. -Examples of OATP1B1 inhibitors include gemfibrozil, erythromycin, clarithromycin, and several protease inhibitors (atazanavir, simeprevir). Inhibitors of P-gp/BCRP In vitro results indicate that letermovir is a substrate of P-gp/BCRP. Changes in letermovir plasma concentrations due to inhibition of P-gp/BCRP by itraconazole were not clinically relevant. Effect of letermovir on other medicinal products Medicinal products mainly eliminated through metabolism or influenced by active transport Letermovir is a general inducer in vivo of enzymes and transporters. Unless a particular enzyme or transporter is also inhibited (see below) induction can be expected. Therefore, letermovir may potentially lead to decreased plasma exposure and possibly reduced efficacy of co-administered medicinal products that are mainly eliminated through metabolism or by active transport. The size of the induction effect is dependent on whether cyclosporine is concomitantly used. The full induction effect can be expected after 10-14 days of letermovir treatment. The time needed to reach steady state of a specific affected medicinal product will also influence the time needed to reach full effect on the plasma concentrations. In vitro, letermovir is an inhibitor of CYP3A, CYP2C8, CYP2B6, BCRP, UGT1A1, OATP2B1, and OAT3 at in vivo relevant concentrations. In vivo studies are available investigating the net effect on CYP3A4, P-gp, OATP1B1/3 additionally on CYP2C19. The net effect in vivo on the other listed enzymes and transporters is not known. Detailed information is presented below. It is unknown whether letermovir may affect the exposure of piperacillin/tazobactam, amphotericine B and micafungin. The potential interaction between letermovir and these medicinal products have not been investigated. There is a theoretical risk of reduced exposure due to induction but the size of the effect and thus clinical relevance is presently unknown. Medicinal products metabolised by CYP3A Letermovir is a moderate inhibitor of CYP3A in vivo. Co-administration of PREVYMIS with oral midazolam (a CYP3A substrate) results in 2-3-fold increased midazolam plasma concentrations. Co- administration of PREVYMIS may result in clinically relevant increases in the plasma concentrations of co-administered CYP3A substrates (see sections 4.3, 4.4, and 5.2). -Examples of such medicinal products include certain immunosuppressants (e.g., cyclosporine, tacrolimus, sirolimus), HMG-CoA reductase inhibitors, and amiodarone (see Table 1). Pimozide and ergot alkaloids are contraindicated (see section 4.3). The size of the CYP3A inhibitory effect is dependent on whether cyclosporine is concomitantly used. Due to time dependent inhibition and simultaneous induction the net enzyme inhibitory effect may not be reached until after 10-14 days. The time needed to reach steady state of a specific affected medicinal product will also influence the time needed to reach full effect on the plasma concentrations. When ending treatment, it takes 10-14 days for the inhibitory effect to disappear. If monitoring is applied, this is recommended the first 2 weeks after initiating and ending letermovir (see section 4.4). Medicinal products transported by OATP1B1/3 Letermovir is an inhibitor of OATP1B1/3 transporters. Administration of PREVYMIS may result in a clinically relevant increase in plasma concentrations of co-administered medicinal products that are OATP1B1/3 substrates. -Examples of such medicinal products include HMG-CoA reductase inhibitors, fexofenadine, repaglinide and glyburide (see Table 1). The magnitude of the OATP1B1/3 inhibition on co-administered medicinal products is likely greater when PREVYMIS is co-administered with cyclosporine (a potent OATP1B1/3 inhibitor). This needs to be considered when cyclosporine is discontinued during letermovir treatment with an OATP1B1/3 substrate. Medicinal products metabolised by CYP2C9 and/or CYP2C19 Co-administration of PREVYMIS with voriconazole (a CYP2C19 substrate) results in significantly decreased voriconazole plasma concentrations, indicating that letermovir is an inducer of CYP2C19. CYP2C9 is likely also induced. Letermovir has the potential to decrease the exposure of CYP2C9 and/or CYP2C19 substrates potentially resulting in subtherapeutic levels. -Examples of such medicinal products include warfarin, voriconazole, diazepam, lansoprazole, omeprazole, esomeprazole, pantoprazole, tilidine, tolbutamide (see Table 1). The effect is expected to be less pronounced for oral letermovir without cyclosporine, than oral letermovir with cyclosporine. This needs to be considered when cyclosporine is discontinued during letermovir treatment with a CYP2C9 or CYP2C19 substrate. See also general information on induction above regarding time courses of the interaction. Medicinal products metabolised by CYP2C8 Letermovir inhibits CYP2C8 in vitro but may also induce CYP2C8 based on its induction potential. The net effect in vivo is unknown. -An example of a medicinal product which is mainly eliminated by CYP2C8 is repaglinide (see Table 1). Concomitant use of repaglinide and letermovir with or without cyclosporine is not recommended. Medicinal products transported by P-gp in the intestine Letermovir is an inducer of intestinal P-gp. Administration of PREVYMIS may result in a clinically relevant decrease in plasma concentrations of co-administered medicinal products that are significantly transported by P-gp in the intestine such as dabigatran and sofosbuvir. Medicinal products metabolised by CYP2B6, UGT1A1 or transported by BCRP or OATP2B1 Letermovir is a general inducer in vivo but has also been observed to inhibit CYP2B6, UGT1A1, BCRP, and OATP2B1 in vitro. The net effect in vivo is unknown. Therefore, the plasma concentrations of medicinal products that are substrates of these enzymes or transporters may increase or decrease when co-administered with letermovir. Additional monitoring may be recommended; refer to the prescribing information for such medicinal products. - Examples of medicinal products that are metabolised by CYP2B6 include bupropion. - Examples of medicinal products metabolised by UGT1A1 are raltegravir and dolutegravir. - Examples of medicinal products transported by BCRP include rosuvastatin and sulfasalazine. - An example of a medicinal product transported by OATP2B1 is celiprolol. Medicinal products transported by the renal transporter OAT3 In vitro data indicate that letermovir is an inhibitor of OAT3; therefore, letermovir may be an OAT3 inhibitor in vivo. Plasma concentrations of medicinal products transported by OAT3 may be increased. -Examples of medicinal products transported by OAT3 includes ciprofloxacin, tenofovir, imipenem, and cilastin. General information If dose adjustments of concomitant medicinal products are made due to treatment with PREVYMIS, doses should be readjusted after treatment with PREVYMIS is completed. A dose adjustment may also be needed when changing immunosuppressant. Table 1 provides a listing of established or potentially clinically significant medicinal product interactions. The medicinal product interactions described are based on studies conducted with PREVYMIS or are predicted medicinal product interactions that may occur with PREVYMIS (see sections 4.3, 4.4, 5.1, and 5.2). Table 1: Interactions and dose recommendations with other medicinal products. Note that the table is not extensive but provides examples of clinically relevant interactions. See also the general text on DDIs above. Unless otherwise specified, interaction studies have been performed with oral letermovir without cyclosporine. Please note that the interaction potential and clinical consequences may be different depending on whether cyclosporine is concomitantly used. When changing immunosuppressant, the recommendation concerning co-administration should be revisited. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) Antibiotics nafcillin Interaction not studied. Nafcillin may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS and nafcillin is not recommended. (P-gp/UGT induction) Antifungals fluconazole ↔ fluconazole No dose adjustment required. (400 mg single AUC 1.03 (0.99, 1.08) dose)/letermovir Cmax 0.95 (0.92, 0.99) (480 mg single dose) ↔ letermovir AUC 1.11 (1.01, 1.23) Cmax 1.06 (0.93, 1.21) Interaction at steady state not studied. Expected; ↔ fluconazole ↔ letermovir itraconazole ↔ itraconazole No dose adjustment required. (200 mg once daily AUC 0.76 (0.71, 0.81) PO)/letermovir Cmax 0.84 (0.76, 0.92) (480 mg once daily PO) ↔ letermovir AUC 1.33 (1.17, 1.51) Cmax 1.21 (1.05, 1.39) posaconazole‡ ↔ posaconazole No dose adjustment required. (300 mg single dose)/ AUC 0.98 (0.82, 1.17) letermovir (480 mg Cmax 1.11 (0.95, 1.29) daily) voriconazole‡ ↓ voriconazole If concomitant administration is necessary, (200 mg twice daily)/ AUC 0.56 (0.51, 0.62) TDM for voriconazole is recommended the letermovir (480 mg Cmax 0.61 (0.53, 0.71) first 2 weeks after initiating or ending daily) letermovir, as well as after changing (CYP2C9/19 induction) immunosuppressant. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) Antimycobacterials rifabutin Interaction not studied. Rifabutin may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS and rifabutin is not recommended. (P-gp/UGT induction) rifampicin (600 mg single dose ↔letermovir PO)/ letermovir AUC 2.03 (1.84, 2.26) (480 mg single dose Cmax 1.59 (1.46, 1.74) PO) C24 2.01 (1.59, 2.54) (OATP1B1/3 and/or P-gp inhibition) (600 mg single dose ↔ letermovir intravenous)/ AUC 1.58 (1.38, 1.81) letermovir (480 mg Cmax 1.37 (1.16, 1.61) single dose PO) C24 0.78 (0.65, 0.93) Multiple dose rifampicin decreases plasma (OATP1B1/3 and/or P-gp concentrations of letermovir. inhibition) Co-administration of PREVYMIS and (600 mg once daily ↓ letermovir rifampicin is not recommended. PO)/ letermovir AUC 0.81 (0.67, 0.98) (480 mg once daily Cmax 1.01 (0.79, 1.28) PO) C24 0.14 (0.11, 0.19) (Sum of OATP1B1/3 and/or P- gp inhibition and P-gp/UGT induction) (600 mg once daily ↓ letermovir PO (24 hours after AUC 0.15 (0.13, 0.17) rifampicin))§/ Cmax 0.27 (0.22, 0.31) letermovir (480 mg C24 0.09(0.06, 0.12) once daily PO) (P-gp/UGT induction) Antipsychotics thioridazine Interaction not studied. Thioridazine may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS and thioridazine is not recommended. (P-gp/UGT induction) Endothelin antagonists bosentan Interaction not studied. Bosentan may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS and bosentan is not recommended. (P-gp/UGT induction) Antivirals acyclovir‡ ↔ acyclovir No dose adjustment required. (400 mg single dose)/ AUC 1.02 (0.87, 1.2) letermovir (480 mg Cmax 0.82 (0.71, 0.93) daily) Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) valacyclovir Interaction not studied. No dose adjustment required. Expected: ↔ valacyclovir Herbal products St. John’s wort Interaction not studied. St. John’s wort may decrease plasma (Hypericum Expected: concentrations of letermovir. perforatum) ↓ letermovir Co-administration of PREVYMIS and St. John’s wort is contraindicated. (P-gp/UGT induction) HIV medicinal products efavirenz Interaction not studied. Efavirenz may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS and (P-gp/UGT induction) efavirenz is not recommended. ↑ or ↓ efavirenz (CYP2B6 inhibition or induction) etravirine, nevirapine, Interaction not studied. These antivirals may decrease plasma ritonavir, lopinavir Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS with these antivirals is not recommended. (P-gp/UGT induction) HMG-CoA reductase inhibitors atorvastatin‡ ↑ atorvastatin Statin-associated adverse events such as (20 mg single dose)/ AUC 3.29 (2.84, 3.82) myopathy should be closely monitored. The letermovir (480 mg Cmax 2.17 (1.76, 2.67) dose of atorvastatin should not exceed daily) 20 mg daily when co-administered with (CYP3A, OATP1B1/3 PREVYMIS#. inhibition) Although not studied, when PREVYMIS is co-administered with cyclosporine, the magnitude of the increase in atorvastatin plasma concentrations is expected to be greater than with PREVYMIS alone. When PREVYMIS is co-administered with cyclosporine, atorvastatin is contraindicated. simvastatin, Interaction not studied. Letermovir may substantially increase pitavastatin, Expected: plasma concentrations of these statins. rosuvastatin ↑ HMG-CoA reductase Concomitant use is not recommended with inhibitors PREVYMIS alone. (CYP3A, OATP1B1/3 When PREVYMIS is co-administered with inhibition) cyclosporine, use of these statins is contraindicated. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) fluvastatin, Interaction not studied. Letermovir may increase statin plasma pravastatin Expected: concentrations. ↑ HMG-CoA reductase inhibitors When PREVYMIS is co-administered with these statins, a statin dose reduction may be (OATP1B1/3 and/or BCRP necessary#. Statin-associated adverse events inhibition) such as myopathy should be closely monitored. When PREVYMIS is co-administered with cyclosporine, pravastatin is not recommended while for fluvastatin, a dose reduction may be necessary#. Statin- associated adverse events such as myopathy should be closely monitored. Immunosuppressants cyclosporine ↑ cyclosporine If PREVYMIS is co-administered with (50 mg single dose)/ AUC 1.66 (1.51, 1.82) cyclosporine, the dose of PREVYMIS letermovir (240 mg Cmax 1.08 (0.97, 1.19) should be decreased to 240 mg once daily daily) (CYP3A inhibition) (see sections 4.2 and 5.1). cyclosporine ↑ letermovir Frequent monitoring of cyclosporine whole (200 mg single dose)/ AUC 2.11 (1.97, 2.26) blood concentrations should be performed letermovir (240 mg Cmax 1.48 (1.33, 1.65) during treatment, and at discontinuation of daily) PREVYMIS and the dose of cyclosporine (OATP1B1/3 inhibition) adjusted accordingly#. mycophenolate ↔mycophenolic acid No dose adjustment required. mofetil AUC 1.08 (0.97, 1.20) (1 g single dose)/ Cmax 0.96 (0.82, 1.12) letermovir (480 mg daily) ↔ letermovir AUC 1.18 (1.04, 1.32) Cmax 1.11 (0.92, 1.34) sirolimus‡ ↑ sirolimus Frequent monitoring of sirolimus whole (2 mg single dose)/ AUC 3.40 (3.01, 3.85) blood concentrations should be performed letermovir (480 mg Cmax 2.76 (2.48, 3.06) during treatment, and at discontinuation of daily) PREVYMIS and the dose of sirolimus (CYP3A inhibition) adjusted accordingly#. Frequent monitoring of sirolimus Interaction not studied. concentrations is recommended at initiation Expected: or discontinuation of cyclosporine ↔ letermovir co-administration with PREVYMIS. When PREVYMIS is co-administered with cyclosporine, also refer to the sirolimus prescribing information for specific dosing recommendations for use of sirolimus with cyclosporine. When PREVYMIS is co-administered with cyclosporine, the magnitude of the increase in concentrations of sirolimus may be greater than with PREVYMIS alone. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) tacrolimus ↑ tacrolimus Frequent monitoring of tacrolimus whole (5 mg single dose)/ AUC 2.42 (2.04, 2.88) blood concentrations should be performed letermovir (480 mg Cmax 1.57 (1.32, 1.86) during treatment, and at discontinuation of daily) (CYP3A inhibition) PREVYMIS and the dose of tacrolimus tacrolimus adjusted accordingly#. (5 mg single dose)/ ↔ letermovir letermovir (80 mg AUC 1.02 (0.97, 1.07) twice daily) Cmax 0.92 (0.84, 1) Oral contraceptives ethinylestradiol (EE) ↔ EE No dose adjustment required. (0.03 mg)/ AUC 1.42 (1.32, 1.52) levonorgestrel Cmax 0.89 (0.83, 0.96) (LNG)‡ (0.15 mg) single ↔ LNG dose/ letermovir AUC 1.36 (1.30, 1.43) (480 mg daily) Cmax 0.95 (0.86, 1.04) Other systemically Risk of ↓ contraceptive steroids Letermovir may reduce plasma acting oral concentrations of other oral contraceptive contraceptive steroids steroids thereby affecting their efficacy. For adequate contraceptive effect to be ensured with an oral contraceptive, products containing EE and LNG should be chosen. Antidiabetic medicinal products repaglinide Interaction not studied. Letermovir may increase or decrease the Expected: plasma concentrations of repaglinide. (The ↑ or ↓ repaglinide net effect is not known). (CYP2C8 induction, CYP2C8 Concomitant use is not recommended. and OATP1B inhibition) When PREVYMIS is co-administered with cyclosporine, the plasma concentrations of repaglinide is expected to increase due to the additional OATP1B inhibition by cyclosporine. Concomitant use is not recommended#. glyburide Interaction not studied. Letermovir may increase the plasma Expected: concentrations of glyburide. ↑ glyburide Frequent monitoring of glucose (OATP1B1/3 inhibition concentrations is recommended the first CYP3A inhibition, CYP2C9 2 weeks after initiating or ending induction) letermovir. When PREVYMIS is co-administered with cyclosporine, refer also to the glyburide prescribing information for specific dosing recommendations. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) Antiepileptic medicinal products (see also general text) carbamazepine, Interaction not studied. Carbamazepine or phenobarbital may phenobarbital Expected: decrease plasma concentrations of ↓ letermovir letermovir. Co-administration of PREVYMIS and (P-gp/UGT induction) carbamazepine or phenobarbital is not recommended. phenytoin Interaction not studied. Phenytoin may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Letermovir may decrease the plasma (P-gp/UGT induction) concentrations of phenytoin. ↓ phenytoin Co-administration of PREVYMIS and phenytoin is not recommended. (CYP2C9/19 induction) Oral anticoagulants warfarin Interaction not studied. Letermovir may decrease the plasma Expected: concentrations of warfarin. ↓ warfarin Frequent monitoring of International (CYP2C9 induction) Normalised Ratio (INR) should be performed when warfarin is co- administered with PREVYMIS treatment#. Monitoring is recommended the first 2 weeks after initiating or ending letermovir, as well as after changing immunosuppressant. dabigatran Interaction not studied. Letermovir may decrease the plasma Expected: concentrations of dabigatran and may ↓ dabigatran decrease efficacy of dabigatran. Concomitant use of dabigatran should be (intestinal P-gp induction) avoided due to the risk of reduced dabigatran efficacy. When PREVYMIS is co-administered with cyclosporine, dabigatran is contraindicated. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) Sedatives midazolam ↑ midazolam Close clinical monitoring for respiratory (1 mg single dose intravenous: depression and/or prolonged sedation intravenous)/ AUC 1.47 (1.37, 1.58) should be exercised during co- letermovir (240 mg Cmax 1.05 (0.94, 1.17) administration of PREVYMIS with once daily PO) midazolam. Dose adjustment of midazolam PO: should be considered#. The increase in midazolam (2 mg AUC 2.25 (2.04, 2.48) midazolam plasma concentration may be single dose PO) / Cmax 1.72 (1.55, 1.92) greater when oral midazolam is letermovir (240 mg administered with letermovir at the clinical once daily PO) (CYP3A inhibition) dose than with the dose studied. Opioid agonists Examples: alfentanil, Interaction not studied. Frequent monitoring for adverse reactions fentanyl Expected: related to these medicinal products is ↑ CYP3A metabolised opioids recommended during co-administration. Dose adjustment of CYP3A metabolised (CYP3A inhibition) opioids may be needed# (see section 4.4). When PREVYMIS is co-administered with cyclosporine, the magnitude of the increase in plasma concentrations of CYP3A metabolised opioids may be greater. Close clinical monitoring for respiratory depression and/or prolonged sedation should be exercised during co- administration of PREVYMIS in combination with cyclosporine and alfentanil or fentanyl. Refer to the respective prescribing information (see section 4.4). Anti-arrhythmic medicinal products amiodarone Interaction not studied. Letermovir may increase the plasma Expected: concentrations of amiodarone. ↑ amiodarone Frequent monitoring for adverse reactions (primarily CYP3A inhibition related to amiodarone is recommended and CYP2C8 inhibition or during co-administration. Monitoring of induction) amiodarone concentrations should be performed regularly when amiodarone is co-administered with PREVYMIS#. quinidine Interaction not studied. Letermovir may increase the plasma Expected: concentrations of quinidine. ↑ quinidine Close clinical monitoring should be (CYP3A inhibition) exercised during administration of PREVYMIS with quinidine. Refer to the respective prescribing information#. Concomitant Effect on concentration† Recommendations concerning co- medicinal product Mean ratio (90 % confidence administration with PREVYMIS interval) for AUC, Cmax (likely mechanism of action) Cardiovascular medicinal products digoxin‡ ↔ digoxin No dose adjustment required. (0.5 mg single dose)/ AUC 0.88 (0.80, 0.96) letermovir (240 mg Cmax 0.75 (0.63, 0.89) twice daily) (P-gp induction) Proton pump inhibitors omeprazole Interaction not studied. Letermovir may decrease the plasma Expected: concentrations of CYP2C19 substrates. ↓omeprazole Clinical monitoring and dose adjustment (induction of CYP2C19) may be needed. Interaction not studied. Expected: ↔ letermovir pantoprazole Interaction not studied. Letermovir may decrease the plasma Expected: concentrations of CYP2C19 substrates. ↓ pantoprazole Clinical monitoring and dose adjustment (likely due to induction of may be needed. CYP2C19) Interaction not studied. Expected: ↔ letermovir Wakefulness-promoting agents modafinil Interaction not studied. Modafinil may decrease plasma Expected: concentrations of letermovir. ↓ letermovir Co-administration of PREVYMIS and modafinil is not recommended. (P-gp/UGT induction) *This table is not all inclusive. † ↓ =decrease, ↑ =increase ↔ =no clinically relevant change ‡ One-way interaction study assessing the effect of letermovir on the concomitant medicinal product. § These data are the effect of rifampicin on letermovir 24 hours after final rifampicin dose. # Refer to the respective prescribing information. Paediatric population Interaction studies have only been performed in adults.

פרטי מסגרת הכללה בסל
א. הטיפול בתרופה יינתן לחולה מבוגר שעובר השתלת מח עצם אלוגנאית ויש לו בדיקה סרולוגית חיובית ל CMV (סרו-חיובי ל CMV). ב. הטיפול בתרופה לא יינתן בשילוב עם Valganciclovir.ג. מתן התרופה ייעשה לפי מרשם של מומחה במחלות זיהומיות או מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. הטיפול בתרופה יינתן לחולה מבוגר שעובר השתלת מח עצם אלוגנאית ויש לו בדיקה סרולוגית חיובית ל CMV (סרו-חיובי ל CMV) הנמצא בסיכון גבוה לרה אקטיבציה של CMV. לעניין זה סיכון גבוה לרה-אקטיבציה יוגדר כאחד מאלה: 1. תורם שלילי ל CMV (סרו-נגטיב); 2. השתלה מתורם שאינו מתאים mismatch; 3. השתלה מתורם הפלו haplo-identical; 4. השתלה מתאי אב שמקורם בחבל טבור cord blood; 5. מושתל עם GvHD מדרגה שניה (Grade 2) ומעלה; 6. שימוש ב-ex vivo T-cell–depleted grafts ב. הטיפול בתרופה לא יינתן בשילוב עם Valganciclovir. ג. מתן התרופה ייעשה לפי מרשם של מומחה במחלות זיהומיות או מומחה בהמטולוגיה. | 30/01/2020 | המטולוגיה | Allogeneic hematopoietic stem cell transplant, השתלת מח עצם אלוגנאית | |
| א. הטיפול בתרופה יינתן לחולה מבוגר שעובר השתלת מח עצם אלוגנאית ויש לו בדיקה סרולוגית חיובית ל CMV (סרו-חיובי ל CMV). ב. הטיפול בתרופה לא יינתן בשילוב עם Valganciclovir. ג. מתן התרופה ייעשה לפי מרשם של מומחה במחלות זיהומיות או מומחה בהמטולוגיה. | 03/02/2022 | המטולוגיה | Allogeneic hematopoietic stem cell |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
30/01/2020
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
166 13 35974 00
מחיר
0 ₪
מידע נוסף
