Quest for the right Drug
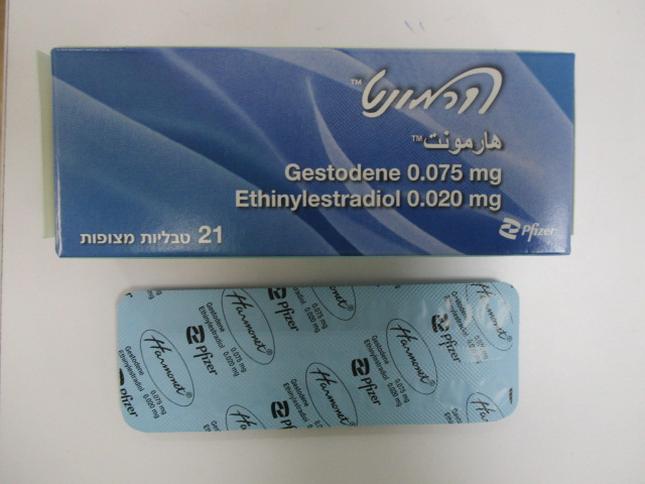
הרמונט HARMONET (ETHINYLESTRADIOL, GESTODENE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות : COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4. Special warnings and precautions for use Warnings If any of the conditions or risk factors mentioned below is present, the suitability of Harmonet® should be discussed with the woman. In the event of aggravation, or first appearance of any of these conditions or risk factors, the woman should be advised to contact her doctor to determine whether the use of Harmonet® should be discontinued. Risk of venous thromboembolism (VTE) The use of any combined hormonal contraceptive (CHC) increases the risk of venous thromboembolism (VTE) compared with no use. Products that contain levonorgestrel, norgestimate or norethisterone are associated with the lowest risk of VTE. Other products such as Harmonet® may have up to twice this level of risk. The decision to use any product other than one with the lowest VTE risk should be taken only after a discussion with the woman to ensure she understands the risk of VTE with Harmonet®, how her current risk factors influence this risk, and that her VTE risk is highest in the first ever year of use. There is also some evidence that the risk is increased when a CHC is re-started after a break in use of 4 weeks or more. In women who do not use a CHC and are not pregnant about 2 out of 10,000 will develop a VTE over the period of one year. However, in any individual woman the risk may be far higher, depending on her underlying risk factors (see below). It is estimated1 that out of 10,000 women who use a CHC containing gestodene between 9 and 12 women will develop a VTE in one year; this compares with about 62 in women who use a levonorgestrel-containing CHC. In both cases, the number of VTEs per year is fewer than the number expected during pregnancy or in the postpartum period. VTE may be fatal in 1-2% of cases. 1 These incidences were estimated from the totality of the epidemiological study data, using relative risks for the different products compared with levonorgestrel-containing CHCs. 2 Mid-point of range of 5-7 per 10,000 WY, based on a reative risk for CHCs containing levonorgestrel versus non-use of approximately 2.3 to 3.6. Number of VTE events per 10,000 women in one year Extremely rarely, thrombosis has been reported to occur in CHC users in other blood vessels, e.g. hepatic, mesenteric, renal or retinal veins and arteries. For information concerning vascular thrombosis of the retina, see paragraph "Ocular lesions". Risk factors for VTE The risk for venous thromboembolic complications in CHC users may increase substantially in a woman with additional risk factors, particularly if there are multiple risk factors (see table). Harmonet® is contraindicated if a woman has multiple risk factors that put her at high risk of venous thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors – in this case her total risk of VTE should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3). Table: Risk factors for VTE Risk factor Comment Obesity (body mass index over Risk increases substantially as BMI rises. 30 kg/m²) Particularly important to consider if other risk factors also present. Prolonged immobilisation, major In these situations it is advisable to discontinue use of surgery, any surgery to the legs or the pill (in the case of elective surgery at least four pelvis, neurosurgery, or major trauma weeks in advance) and not resume until two weeks after complete remobilisation. Another method of contraception should be used to avoid unintentional pregnancy. Antithrombotic treatment should be considered if Harmonet® has not been discontinued in advance. Note: temporary immobilisation including air travel >4 hours can also be a risk factor for VTE, particularly in women with other risk factors Positive family history (venous If a hereditary predisposition is suspected, the woman thromboembolism ever in a sibling or should be referred to a specialist for advice before parent especially at a relatively early deciding about any CHC use age eg. before 50). Other medical conditions associated Cancer, systemic lupus erythematosus, haemolytic with VTE uraemic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell disease Increasing age Particularly above 35 years There is no consensus about the possible role of varicose veins and superficial thrombophlebitis in the onset or progression of venous thrombosis. The increased risk of thromboembolism in pregnancy, and particularly the 6 week period of the puerperium, must be considered. Harmonet® cannot be started until the 28th day after a delivery (for users who choose not to breast-feed) or after an abortion or miscarriage in the second trimester (for information on “Pregnancy and lactation” see section 4.6). Symptoms of VTE (deep vein thrombosis and pulmonary embolism) In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC. Symptoms of deep vein thrombosis (DVT) can include: - unilateral swelling of the leg and/or foot or along a vein in the leg; - pain or tenderness in the leg which may be felt only when standing or walking, - increased warmth in the affected leg; red or discoloured skin on the leg. Symptoms of pulmonary embolism (PE) can include: - sudden onset of unexplained shortness of breath or rapid breathing; - sudden coughing which may be associated with haemoptysis; - sharp chest pain; - severe light headedness or dizziness; - rapid or irregular heartbeat. Some of these symptoms (e.g. “shortness of breath”, “coughing”) are non-specific and might be misinterpreted as more common or less severe events (e.g. respiratory tract infections). Other signs of vascular occlusion can include: sudden pain, swelling and slight blue discoloration of an extremity. If the occlusion occurs in the eye, symptoms can range from painless blurring of vision which can progress to loss of vision. Sometimes loss of vision can occur almost immediately. Risk of arterial thromboembolism (ATE) Epidemiological studies have associated the use of CHCs with an increased risk for arterial thromboembolism (myocardial infarction) or for cerebrovascular accident (eg transient ischaemic attack, stroke). Arterial thromboembolic events may be fatal. Risk factors for ATE The risk of arterial thromboembolic complications or of a cerebrovascular accident in CHC users increases in women with risk factors (see table). Harmonet® is contraindicated if a woman has one serious or multiple risk factors for ATE that puts her at high risk of arterial thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors - in this case her total risk should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3). Table: Risk factors for ATE Risk factor Comment Increasing age Particularly above 35 years Smoking Women should be advised not to smoke if they wish to use a CHC. Women over 35 who continue to smoke should be strongly advised to use a different method of contraception. Hypertension Obesity (body mass index over 30 Risk increases substantially as BMI increases. kg/m2) Particularly important in women with additional risk factors Positive family history (arterial If a hereditary predisposition is suspected, the woman thromboembolism ever in a sibling or should be referred to a specialist for advice before parent especially at relatively early age deciding about any CHC use eg. below 50). Migraine An increase in frequency or severity of migraine during CHC use (which may be prodromal of a cerebrovascular event) may be a reason for immediate discontinuation Other medical conditions associated Diabetes mellitus, hyperhomocysteinaemia, valvular with adverse vascular events heart disease and atrial fibrillation, dyslipoproteinaemia, systemic lupus erythematosus and coronary disorders Symptoms of ATE In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC. Symptoms of a cerebrovascular accident can include: - sudden numbness or weakness of the face, arm or leg, especially on one side of the body; - sudden trouble walking, dizziness, loss of balance or coordination; - sudden confusion, trouble speaking or understanding; - sudden trouble seeing in one or both eyes; - sudden, severe or prolonged headache with no known cause; - loss of consciousness or fainting with or without seizure. Temporary symptoms suggest the event is a transient ischaemic attack (TIA). Symptoms of MI can include: - pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm, or below the breastbone; - discomfort radiating to the back, jaw, throat, arm, stomach; - feeling of being full, having indigestion or choking; - sweating, nausea, vomiting or dizziness; - extreme weakness, anxiety, or shortness of breath; - rapid or irregular heartbeats. Gynaecological cancers Published data do not demonstrate a causal relationship with the use of oral contraceptives whose benefits appear higher than the risks. However, all women who use this type of product should be kept under close medical supervision. If unexpected vaginal bleeding occurs, the necessary diagnostic measures should be taken to exclude a pregnancy, a malignant tumour or other possible causes. Breast cancer Established risk factors for the development of breast cancer include increasing age, family history, obesity, nulliparity, and late age for first full-term pregnancy. A meta-analysis from 54 epidemiological studies reported that there is a slightly increased risk (RR=1.24) of having breast cancer diagnosed in users of oral CHCs (Collaborative Group on Hormonal Factors in Breast Cancer, Lancet 347 : 1713-1727, 1996). The observed risk decreases and progressively disappears during the 10 years following discontinuation of use of an oral CHC. Since the number of cases of breast cancer in women under 40 years of age is low, the observed increase in this number of breast cancer in users of oral CHCs (whether former or new users) nevertheless remains small in relation to the global risk of appearance of breast cancer during the lifetime of each woman. However, women presenting with nodules in the breast, fibrocystic disease or abnormal images in the mammogram should be followed particularly closely. Cancer of the uterus The most important risk factor for cervical cancer is persistent human papillomavirus infection. Some studies suggest that the use of an estrogen/progestogen contraception for a long period can be associated with an elevated risk of intraepithelial or invasive cervical cancer in some populations of women. However, the precise cause of these observations has not been established and sexual behaviour or other factors such as the involvement of the human papilloma virus (HPV) could be cited to explain these observations. In cases of undiagnosed genital bleeding, adequate diagnostic measures are indicated. Hepatic tumours and diseases In very rare cases, benign hepatic tumours such as hepatic adenoma - and in even rarer cases, malignant hepatic tumours such as hepatocellular carcinoma - have been reported in oral CHC users. The risk of developing a tumour increases with the duration of treatment. In isolated cases, these tumours have led to life-threatening intra-abdominal haemorrhage. Women with a history of oral CHC-related cholestasis and women who develop cholestasis during pregnancy are more likely to develop cholestasis with oral CHC use. Such patients who use oral CHCs should be carefully monitored, and oral CHC use should be discontinued if cholestasis recurs. Hepatocellular injury has been reported with oral CHC use. Early identification of drug-related hepatocellular injury can decrease the severity of hepatotoxicity when the drug is discontinued. If hepatocellular injury is diagnosed, patients should stop their oral CHC, use a non-hormonal form of contraception and consult their doctor. Acute or chronic disturbances of liver function may necessitate the discontinuation of oral CHC use until liver function has returned to normal. Headaches and migraine The occurrence or aggravation of a migraine or the development of a new type of recurrent persistent or severe headache requires the immediate discontinuation of treatment and a search for the cause. Users suffering from migraine (particularly those with aura) under treatment with oral CHCs can present a higher risk of developing a cerebrovascular accident (see section 4.3). Ocular lesions Cases of retinal vascular thrombosis capable of causing partial or complete blindness have been associated with usage of oral CHCs. The use of oral CHCs must be discontinued immediately if one of the following phenomena occur: - painless blurred vision - inexplicable loss of sight, gradual or sudden, partial or complete; - proptosis or diplopia; - papillary oedema; - signs of retinal vascular lesions or optic neuritis. In these cases, the necessary diagnostic and therapeutic measures must be taken. Hypertension A rise in arterial blood pressure has been reported in some users of oral CHCs. Another method of contraception should be used in women with hypertension, a history of hypertension or a hypertension based on a pathology (including certain renal pathologies). If an oral CHC is used in these patients, close medical monitoring is recommended and use of the contraceptive should be stopped if there is a significant increase in blood pressure. Oral CHCs are contraindicated in patients with uncontrolled hypertension (see section 4.3). Genital bleeding or absence of menstruation In some women withdrawal bleeding may not occur during the tablet-free interval. If the oral CHC has not been taken according to directions prior to the first missed withdrawal bleed, or if two consecutive withdrawal bleeds are missed, pregnancy should be excluded before continuing the use of oral CHCs and a nonhormonal back-up method of contraception should be used until the possibility of pregnancy is excluded. Metrorrhagia and/or intercurrent blood loss (spotting) sometimes occurs, especially during the first three months that the tablets are taken. Hence any irregular bleeding does not need require investigation before an adaptation period of about three cycles. If metrorrhagia and/or spotting are persistent, occur at irregular intervals during several successive cycles, or for the first time after prolonged use of Harmonet®, a possible organic cause should be investigated. Suitable diagnostic measures should be taken to exclude a pregnancy or tumour. Once a pathological cause has been excluded, the problem of metrorrhagia may be solved by the continuation of the use of Harmonet® or a switch to another hormonal contraceptive. However, due to the increased risk of thromboembolic diseases, great caution is necessary when considering a switch to a pill containing a higher dose of oestrogen. Some women can present with oligomenorrhoea or amenorrhoea (possibly accompanied by anovulation) after ending oral contraceptives, especially if these problems were already present before treatment was started. These phenomena generally stop spontaneously. If they are prolonged, it may be necessary to investigate a possible pineal gland pathology. Depression Depressed mood and depression are well-known undesirable effects of hormonal contraceptive use (see section 4.8). Depression can be serious and is a well-known risk factor for suicidal behaviour and suicide. Women should be advised to contact their physician in case of mood changes and depressive symptoms, including shortly after initiating the treatment. Women with a history of depression should be closely monitored. If a serious depression develops during use of Harmonet®, the treatment should be stopped and another method of contraceptive should be used to determine the causality of Harmonet®. Immunity Angio-edema Exogenous estrogens may induce or exacerbate symptoms of hereditary and acquired angioedema. Glucose and lipid metabolism Glucose intolerance has been reported in users of oral CHCs. Users of oral CHCs who have glucose intolerance or suffer from diabetes mellitus should be closely monitored. Women under oral contraceptives who are being treated for hyperlipidaemia (hypertriglyceridaemia, hypercholesterolaemia) should be closely monitored. A small portion of women will have adverse lipid changes while taking oral CHCs. Use of an additional non-hormonal, mechanical method of contraception is recommended in women with uncontrolled dyslipidemias. Persistent hypertriglyceridaemia can occur in a low proportion of oral CHC users. Elevations of plasma triglycerides in oral CHC users may lead to pancreatitis and other complications. If the hypertriglyceridaemia cannot be controlled, a non-hormonal method of contraception should be considered. Other warnings If one of the following situations occurs, treatment with Harmonet® must be stopped immediately: - acute disorders of hearing or other sensory disorders; - at the first symptoms of thrombophlebitis or thromboembolic disease; - at the onset of cholestatic jaundice, anicteric hepatitis or generalised pruritus; - an increase in number of epileptic seizures. Particular attention should be paid to users : - presenting with benign breast tumours; - presenting with uterine dystrophies (hyperplasia, fibromas); - presenting with hyperprolactinaemia with or without galactorrhoea; - with a history or current pathology known to be associated with, or which can worsen during pregnancy or the usage of oral CHCs: epilepsy, otosclerosis, asthma, varicose veins, gestational herpes, gallstones, systemic lupus erythematosis, hepatic, cardiac or renal dysfunction, chorea, haemolytic uraemic syndrome. If contraception fails, an ectopic pregnancy can occur just as easily as an intra-uterine pregnancy. If chloasma/melasma appears during a pregnancy or under oral CHCs, exposure to sunlight should be avoided. Diarrhoea and vomiting can reduce the intestinal absorption of oral CHCs (see section 4.2). Use of oral contraceptives can affect the normal metabolism of tryptophan, which in turn can cause a relative deficiency of pyridoxine. However, the clinical relevance of this is not yet known. Serum levels of folates can be reduced by the use of oral CHCs. Users who become pregnant shortly after ending oral contraceptive treatment run an increased risk of developing folate deficiency with its associated complications. Harmonet® contains lactose and sucrose. Patients with rare hereditary problems of fructose intolerance,galactose intolerance, total lactase deficiency, glucose-galactose malabsorption or sucrase- isomaltase insufficiency should not take this medicine. Medical examination/consultation Prior to the initiation or reinstitution of Harmonet® a complete medical history (including family history) should be taken and pregnancy must be ruled out. Blood pressure should be measured and a physical examination (an examination of the breasts, liver, extremities and pelvic organs, including cervical cytology) should be performed, guided by the contra-indications (see section 4.3) and warnings (see section 4.4). It is important to draw a woman’s attention to the information on venous and arterial thrombosis, including the risk of Harmonet® compared with other CHCs, the symptoms of VTE and ATE, the known risk factors and what to do in the event of a suspected thrombosis. For every combination of estrogens/progestogens, the treatment prescribed should contain the lowest possible dosage of estrogens/progestogens compatible with a low risk of failure and the needs of the user. The woman should also be instructed to carefully read the user leaflet and to adhere to the advice given. The frequency and nature of examinations should be based on established practice guidelines and be adapted to the individual woman. Women should be advised that oral contraceptives do not protect against HIV infections (AIDS) and other sexually transmitted diseases. Laboratory tests The use of oral CHCs may cause certain physiologic changes that may be reflected in the results of certain laboratory tests, including: - biochemical parameters of liver function (including a decrease in bilirubin and alkaline phosphatase), thyroid function (increased total T3 and T4 due to increased TBG, decreased free T3-resin uptake), adrenal function (increased plasma cortisol, increased cortisol binding globulin, decreased dehydroepiandrosterone sulphate (DHEAS), and renal function (increased plasma creatinine levels and creatinine clearance) - plasma levels of (carrier) proteins, such as corticosteroid-binding globulin and lipid/lipoprotein fractions - parameters of carbohydrate metabolism - parameters of coagulation and fibrinolysis - decreased serum folate levels Oral contraceptives can give false positive results during the evaluation of neutrophilic alkaline phosphatase activity in the early diagnosis of pregnancy.
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
Contraception
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
15.03.22 - עלון לצרכן אנגלית 15.03.22 - עלון לצרכן עברית 15.03.22 - עלון לצרכן ערבית 11.05.23 - עלון לצרכן עברית 17.07.23 - עלון לצרכן אנגלית 17.07.23 - עלון לצרכן עברית 17.07.23 - עלון לצרכן ערבית 30.05.24 - עלון לצרכן עברית 21.08.24 - עלון לצרכן אנגלית 22.08.24 - עלון לצרכן ערבית 28.05.12 - החמרה לעלון 29.06.15 - החמרה לעלון 26.07.15 - החמרה לעלון 12.01.21 - החמרה לעלון 20.10.21 - החמרה לעלון 11.05.23 - החמרה לעלון 30.05.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
הרמונט