Quest for the right Drug
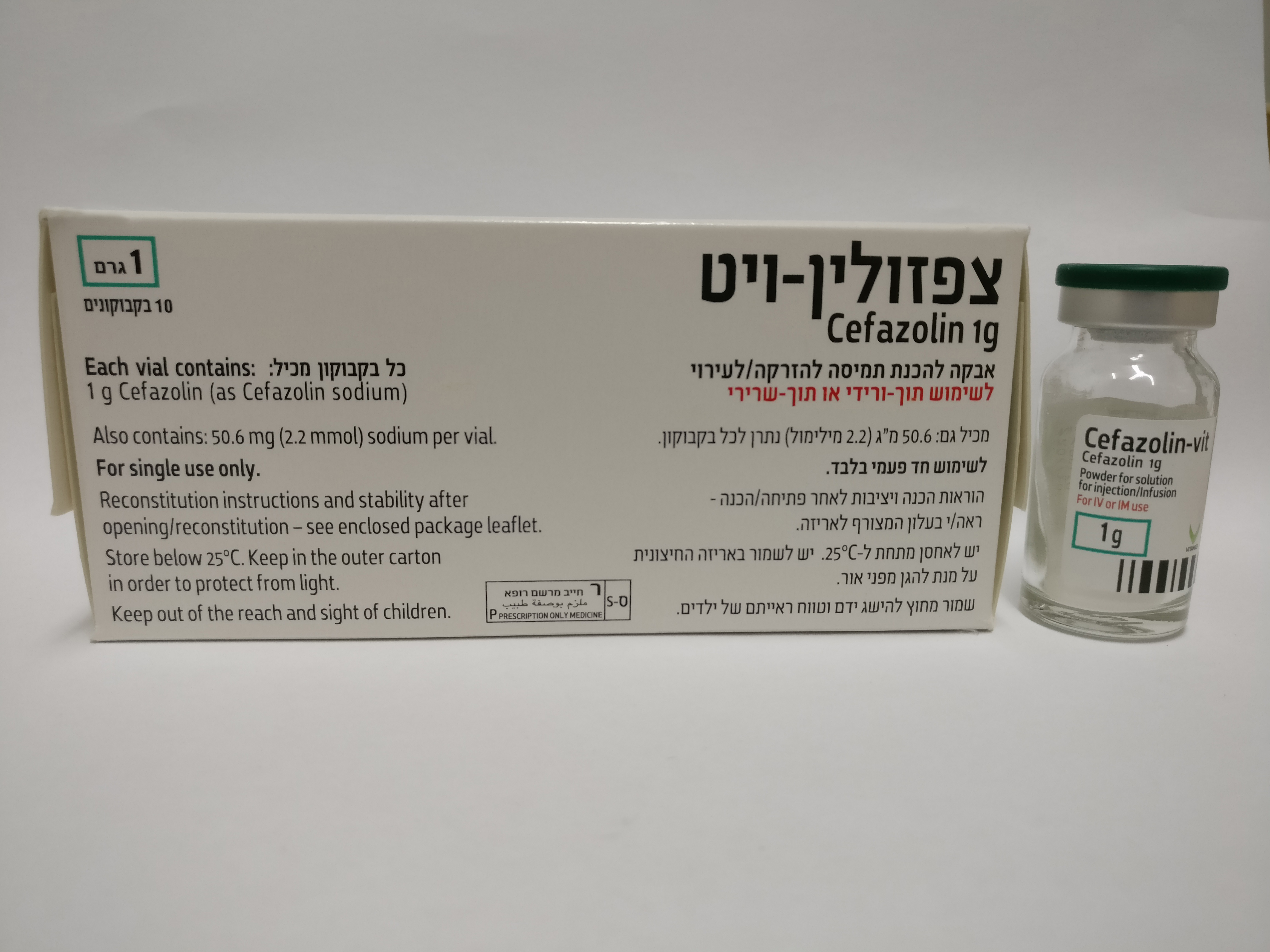
צפזולין- ויט CEFAZOLIN -VIT (CEFAZOLIN AS SODIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-ורידי : I.M, I.V
צורת מינון:
אבקה להמסה להזרקהאינפוזיה : POWDER FOR SOLUTION FOR INJ/INF
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other beta-lactam antibacterials, first-generation cephalosporins ATC-Code: J01DB04 Mode of action: The bactericidal activity of cefazolin results from the inhibition of bacterial cell wall synthesis (during the growth phase) caused by an inhibition of penicillin-binding proteins (PBPs) like transpeptidases. Pharmacokinetics and pharmacodynamics relationship: The extent of the bactericidal activity depends on the period of time during which the serum level of the active substance exceeds the minimum inhibitory concentration (MIC) of the pathogen. Mechanisms of resistance: A resistance to cefazolin may be caused by the following mechanisms: - inactivation by beta-lactamases. Cefazolin exhibits a wide stability against penicillinases of gram-positive bacteria, but only a minor stability against numerous plasmid encoded beta- lactamases, e.g. extended-spectrum beta-lactamases (ESBLs) or by chromosomal encoded beta-lactamases of the AmpC type. - reduced affinity of PBPs to cefazolin. The acquired resistance of Pneumococci and other Streptococci is caused by modifications of already existing PBPs as a consequence of a mutation process. By contrast, the creation of an additional PBP with reduced affinity to cefazolin is responsible for resistance in methicillin-(oxacillin-)resistant Staphylococcus. - inadequate penetration of cefazolin through the outer cell membrane of gram-negative bacteria can lead to insufficient inhibition of the PBPs. - the presence of transport mechanism (efflux pumps) being able to actively transport cefazolin out of the cell. A partial or complete cross resistance of cefazolin occurs with other penicillins and cephalosporins. Breakpoints: The common dilution series is used for testing cefazolin. The following minimum inhibitory concentrations were defined for susceptible and resistant germs: EUCAST (European Committee on Antimicrobial Susceptibility Testing) break points (2011- 01-05, version 10.0): Pathogen Susceptibility Resistance 1 Enterobacterales (only ≤ 0,001 mg/l > 4 mg/l Infections of the urinary tract) 1) 2 Staphylococcus spp. - 2) - 2) 3 Streptococcus spp. (Groups - 3) - 3) A, B, C, G) 3) 4 Streptococci “Viridans”- ≤ 0,5 mg/l > 0,5 mg/l group 5 Non species-related break ≤ 1 mg/l > 2 mg/l points * (exemption: Staphylococcus spp.) 2) 1) exclusively for E. coli and Klebsiella spp. (exept for K. aerogenes) 2) The susceptibility of Staphylococcus spp. is inferred from the Oxacillin resp. Cefoxitin susceptibility. Methicillin (Oxacillin/Cefoxitin)-resistant staphylococci are rated resistant against cephalosporines independently of the outcome of the susceptibility testing. 3) The beta-lactam susceptibility of streptococcus groups A, B, C and G is inferred from the penicillin susceptibility. * based on pharmacokinetic data Susceptibility: The prevalence of acquired resistance may vary geographically and over time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalence of resistance is such that the efficacy of cefazolin in at least some types of infections is questionable. Commonly susceptible species Gram-positive aerobes Staphylococcus aureus (methicillin-susceptible)° Staphylococcus saprophyticus° Streptococcus agalactiae° Streptococcus pneumoniae Streptococcus pyogenes° Gram-negative aerobes Citrobacter koseri Species for which acquired resistance may be a problem Gram-positive aerobes Staphylococcus aureus∋ Staphylococcus epidermidis+ Staphylococcus haemolyticus+ Staphylococcus hominis+ Staphylococcus pneumoniae (penicillin-intermediate) Gram-negative aerobes Escherichia coli% Haemophilus influenzae Klebsiella oxytoca+% Klebsiella pneumoniae% Proteus mirabilis% Inherently resistant species Gram-positive aerobes Enterococcus spp. Staphylococcus aureus (methicillin-resistant) Staphylococcus pneumoniae (penicillin-resistant) Gram-negative aerobes Acinetobacter spp. Citrobacter freundii Enterobacter spp. Legionella spp. Morganella morganii Moraxella catarrhalis Proteus vulgaris Pseudomonas aeruginosa Serratia marcescens Stenotrophomonas maltophilia Anaerobes Bacteroides fragilis Others Chlamydia spp. Chlamydophila spp. Mycoplasma spp. ° Literature data, reference books and therapy guidelines support susceptibility. + In at least one region the resistance rate is > 50%. ∋ In the community the resistance rate is < 10%. % ESBL producing strains are always resistant. Further information: Penicillin-resistant Streptococcus pneumoniae are cross-resistant to cephalosporins such as cefazolin.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Cefazolin is administered parenterally. Maximum serum levels after I.M. injection are reached after 30 to 75 minutes. Serum concentration (µg/ml) after intramuscular administration Dose 30 min 1h 2h 4h 6h 8h 500 mg 36.2 36.8 37.9 15.5 6.3 3 1g 60.1 63.8 54.3 29.3 13.2 7.1 Serum concentration (µg/ml) after intravenous administration of 1 g 5 min 15 min 30 min 1h 2h 4h 188.4 135.8 106.8 73.7 45.6 16.5 About 65-92 % of cefazolin is bound to plasma proteins. Cefazolin penetrates very well into tissues including skeletal muscle, myocardial tissue, bone tissue, bile and gallbladder tissue, endometrium and vaginal tissue. Cefazolin crosses the placenta barrier and is also excreted into human milk. Diffusion into cerebrospinal fluid and aqueous fluid is not sufficient. Cefazolin is not metabolized. Most of the administered dose undergoes glomerular filtration and is eliminated with the urine in a microbiologically active form. A smaller part is excreted by bile. The plasma elimination half-life is about 2 hours; in patients with renal impairment, this time can be prolonged.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
