Quest for the right Drug
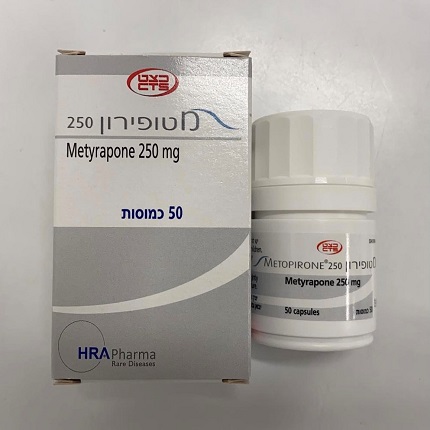
מטופירון 250 METOPIRONE 250 (METYRAPONE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Posology Diagnostic Applications (i) Short single-dose test – diagnosis of ACTH insufficiency This can be performed on an ambulatory basis. In this test, plasma 11- desoxycortisol and/or ACTH levels are determined after a single dose of Metopirone 250. The patient is given 30 mg/kg (maximum 3 g Metopirone 250) at midnight with yoghurt or milk to minimize nausea and vomiting. Paediatric population: The same dose as in adults is recommended in children. The blood sample for the assay is taken early in the morning (7:30– 8:00 hours). The plasma should be frozen as soon as possible. The patient is then given a prophylactic dose of 50 mg cortisone acetate. Evaluation: Normal values will depend on the method used to determine ACTH and 11-desoxycortisol levels. An intact ACTH reserve is generally indicated by an increase in plasma ACTH to at least 44 pmol/L (200 ng/L) or by an increase in 11-desoxycortisol to over 0.2 micromol/L (70 microg/L). Patients with suspected adrenocortical insufficiency should be hospitalised overnight as a precautionary measure. (ii) Multiple-dose test – diagnosis of ACTH insufficiency and differential diagnosis of adrenocortical hyperfunction in Cushing’s syndrome. The patient must be hospitalised. In this test, urinary steroid levels are measured. The first day, baseline values are determined for the 24 hours preceding the test. The second day, 500-750 mg Metopirone 250 are administered every 4 hours for 24 hours, giving a total dose of 3.0-4.5g. The effect is evaluated in two consecutive 24-hour urinary samples. The maximum effect of Metopirone on urinary steroid values should be reached within the next 24 hours. Paediatric population: The paediatric dosage recommendation is based on limited data. In children the dosage should be 15 mg/kg body weight, with a minimum dose of 250 mg every 4 hours for 6 doses. It is recommended that patients take the capsules with milk or after meals to minimize nausea and vomiting. Evaluation: ACTH deficiency: If the anterior pituitary is functioning normally, Metopirone 250 brings about a marked increase in 17-hydroxycorticosteroids (17–OHCS) or 17 ketogenic steroids (17–KGS) in the urine (to at least twice baseline levels). Lack of response indicates secondary adrenocortical insufficiency. Cushing’s syndrome: An excessive increase in 17–OHCS or 17–KGS in the urine after administration of Metopirone 250 indicates over-production of ACTH which has led to adrenocortical hyperplasia (Cushing’s syndrome). Such an increase can be taken as an indication that there is no adrenocortical tumour producing cortisol autonomously. Therapeutic Use Adults For the management of Cushing’s syndrome, the initial dose of metyrapone may vary from 250 to 1,000 mg/day depending on the severity of hypercortisolism and the cause of Cushing’s syndrome. Metyrapone 250 may be initiated at doses of 750 mg/day. For patients with severe Cushing’s syndrome initiation doses may be higher, up to 1500 mg/day. Lower starting doses may be used in cases of mild Cushing’s disease or adrenal adenoma or hyperplasia. The dosage of metyrapone should be adjusted on an individual basis to meet patient’s requirements and depending on tolerability. The usual maintenance dose varies between 500 and 6,000 mg/day. The dose should be given in three or four divided doses. The daily dose should be adjusted after a few days with the aim of lowering the mean plasma/serum cortisol levels and/or the 24 hour urinary free-cortisol levels to a normal target value or until the maximal tolerated dose of metyrapone is reached. Mean serum/plasma cortisol levels may be calculated from the average of 5 to 6 plasma/serum samples obtained throughout a day or from cortisol levels obtained just before the morning dose. Once weekly monitoring of plasma/serum cortisol levels and/or a 24-hour free urinary cortisol levels is necessary to allow further dose adjustments if needed. The dose- adjustment period is usually 1 to 4 weeks. When cortisol levels are close to the optimal levels, longer periods (generally once a month or every 2 months) are sufficient for the monitoring. A physiological corticosteroid replacement therapy may be added to a complete cortisol blockade by metyrapone (block-and-replace regimen). This should be started when the serum or urine cortisol is in the normal range and the metyrapone doses are increased to achieve complete suppression of cortisol secretion. In case of rapid dose-escalation or for patients with cyclic Cushing’s syndrome, a physiological corticosteroid replacement therapy may be added. Special populations Paediatric population: The paediatric dosage recommendation is based on limited data. Case reports showed that there is no specific dosage recommendation for paediatric use in the treatment of Cushing’s syndrome. The dose should be adjusted on an individual basis as a function of cortisol levels and tolerability. Elderly population: Dosage as for adults. There is limited data available on the use of metyrapone in elderly (≥ 65 years old). Clinical evidence indicates that no special dosage recommendations are required in all indications. Method of administration The capsules should be taken with milk or after a meal to minimise nausea and vomiting which can lead to impaired absorption.

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול במקרים האלה:א. בדיקה אבחנתית לאי ספיקה אדרנוקורטיקלית משנית;ב. טיפול בבצקת עמידה הקשורה לעליה בהפרשת אלדוסטרון;ג. טיפול בתסמונת קושינג אנדוגנית.הטיפול לא יינתן בשילוב עם Ketoconazole. הטיפול בתרופה האמורה ייעשה לפי מרשם של רופא מומחה באנדוקרינולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| בדיקה אבחנתית לאי ספיקה אדרנוקורטיקלית משנית | 01/01/1995 | אנדוקרינולוגיה | ||
| טיפול בתסמונת קושינג אנדוגנית. הטיפול לא יינתן בשילוב עם Ketoconazole. | 30/01/2020 | אנדוקרינולוגיה | ||
| טיפול בבצקת עמידה הקשורה לעליה בהפרשת אלדוסטרון | 01/01/1995 | אנדוקרינולוגיה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
