Quest for the right Drug
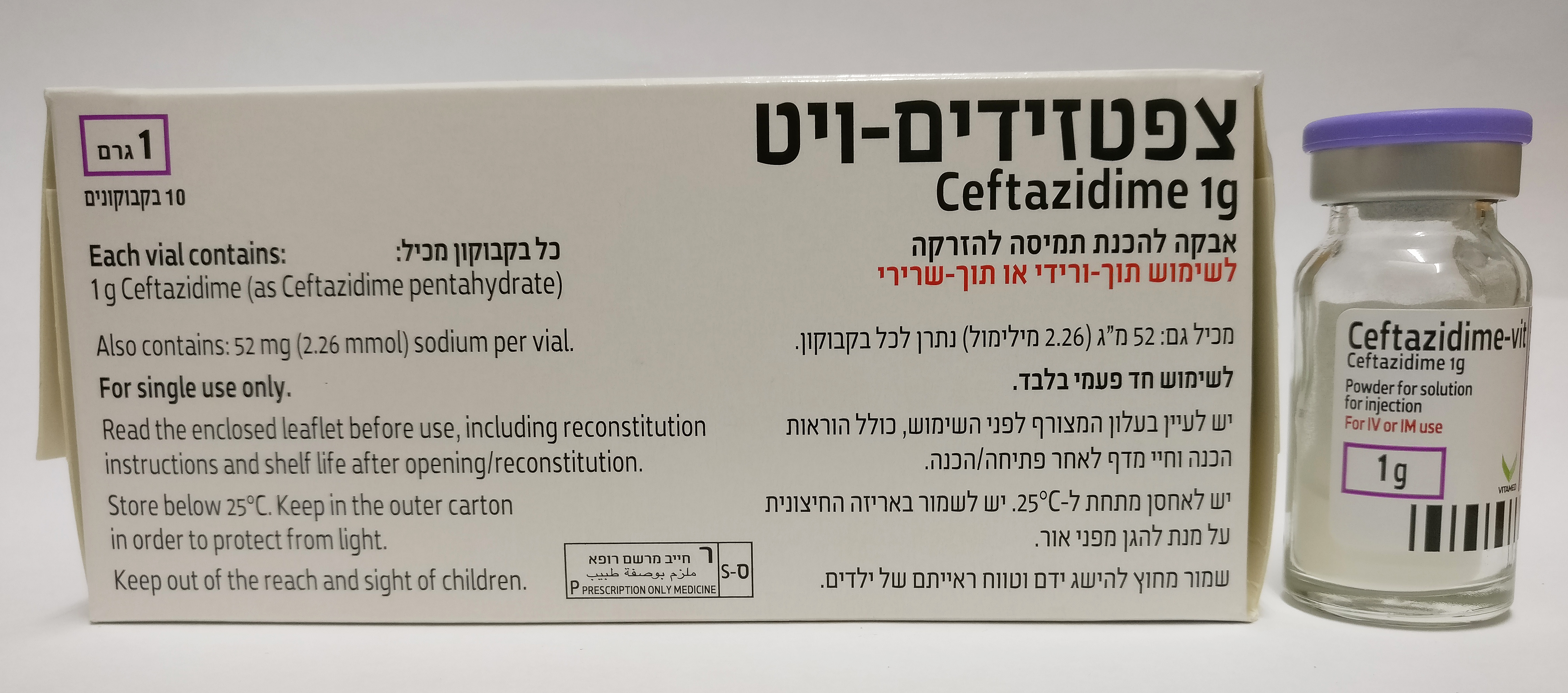
צפטזידים- ויט CEFTAZIDIME - VIT (CEFTAZIDIME AS PENTAHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-ורידי : I.M, I.V
צורת מינון:
אבקה להכנת תמיסה לזריקה : POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Anti-bacterials for systemic use. Third-generation cephalosporins ATC code: J01DD02 Mechanism of action Ceftazidime inhibits bacterial cell wall synthesis following attachment to penicillin binding proteins (PBPs). This results in the interruption of cell wall (peptidoglycan) biosynthesis, which leads to bacterial cell lysis and death. PK/PD relationship For cephalosporins, the most important pharmacokinetic-pharmacodynamic index correlating with in vivo efficacy has been shown to be the percentage of the dosing interval that the unbound concentration remains above the minimum inhibitory concentration (MIC) of ceftazidime for individual target species (i.e. %T>MIC). Mechanism of Resistance Bacterial resistance to ceftazidime may be due to one or more of the following mechanisms: • hydrolysis by beta-lactamases. Ceftazidime may be efficiently hydrolysed by extended- spectrum beta-lactamases (ESBLs), including the SHV family of ESBLs and AmpC enzymes that may be induced or stably derepressed in certain aerobic Gram-negative bacterial species. • reduced affinity of penicillin-binding proteins for ceftazidime. • outer membrane impermeability, which restricts access of ceftazidime to penicillin binding proteins in Gram-negative organisms. • bacterial efflux pumps. Breakpoints Minimum inhibitory concentration (MIC) breakpoints established by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) are as follows: Organism Breakpoints (mg/L) S I R Enterobacteriaceae ≤1 2-4 >4 Pseudomonas ≤81 - >8 aeruginosa Non-species related ≤4 8 >8 breakpoints2 S=Susceptible, I=Intermediate, R=Resistant 1 The breakpoints relate to high dose therapy (2 g x 3). 2 Non-species related breakpoints have been determined mainly on the basis of PK/PD data and are independent of MIC distributions of specific species. They are for use only for species not mentioned in the table or footnotes. Microbiological Susceptibility The prevalence of acquired resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalence of resistance is such that the utility of ceftazidime in at least some types of infections is questionable. Commonly Susceptible Species Gram-positive aerobes: Streptococcus pyogenes Streptococcus agalactiae Gram-negative aerobes: Citrobacter koseri Haemophilus influenzae Moraxella catarrhalis Neisseria meningitidis Pasteurella multocida Proteus mirabilis Proteus spp (other) Providencia spp. Species for which acquired resistance may be a problem Gram-negative aerobes: Acinetobacter baumannii+ Burkholderia cepacia Citrobacter freundii Enterobacter aerogenes Enterobacter cloacae Escherichia coli Klebsiella pneumoniae Klebsiella spp (other) Pseudomonas aeruginosa Serratia spp Morganella morganii Gram-positive aerobes: Staphylococcus aureus£ Streptococcus pneumoniae££ Viridans group streptococcus Gram-positive anaerobes: Clostridium perfringens Peptostreptococcus spp. Gram-negative anaerobes Fusobacterium spp. Inherently resistant organisms Gram-positive aerobes: Enterococcus spp including Enterococcus faecalis and Enterococcus faecium Listeria spp. Gram-positive anaerobes: Clostridium difficile. Gram-negative anaerobes Bacteroides spp. (many strains of Bacteroides fragilis are resistant). Others: Chlamydia spp Mycoplasma spp Legionella spp. £ S.aureus that is methicillin susceptible are considered to have inherent low susceptibility to ceftazidime. All methicillin-resistant S.Aureus are resistant to ceftazidime. ££ S.pneumoniae that demonstrate intermediate susceptibility or are resistant to penicillin can be expected to demonstrate at least reduced susceptibility to ceftazidime. + High rates of resistance have been observed in one or more areas/countries/regions within the EU.
Pharmacokinetic Properties
5.2. Pharmacokinetic properties Absorption After intramuscular administration of 500 mg and 1 g of ceftazidime, peak plasma levels of 18 and 37 mg/l respectively are achieved rapidly. Five minutes after intravenous bolus injection of 500 mg, 1 g or 2 g, plasma levels are 46, 87 and 170 mg/l, respectively. The kinetics of ceftazidime are linear within the single dose range of 0.5 to 2 g following intravenous or intramuscular dosing. Distribution The serum protein binding of ceftazidime is low at about 10%. Concentrations in excess of the MIC for common pathogens can be achieved in tissues such as bone, heart, bile, sputum, aqueous humour, synovial, pleural and peritoneal fluids. Ceftazidime crosses the placenta readily, and is excreted in the breast milk. Penetration of the intact blood-brain barrier is poor, resulting in low levels of ceftazidime in the CSF in the absence of inflammation. However, concentrations of 4 to 20 mg/l or more are achieved in the CSF when the meninges are inflamed. Biotransformation Ceftazidime is not metabolised. Elimination After parenteral administration plasma levels decrease with a half-life of about 2 h. Ceftazidime is excreted unchanged into the urine by glomerular filtration; approximately 80 to 90 % of the dose is recovered in the urine within 24 h. Less than 1 % is excreted via the bile. Special patient populations Renal impairment Elimination of ceftazidime is decreased in patients with impaired renal function and the dose should be reduced (see section 4.2). Hepatic impairment The presence of mild to moderate hepatic dysfunction had no effect on the pharmacokinetics of ceftazidime in individuals administered 2 g intravenously every 8 hours for 5 days, provided renal function was not impaired (see section 4.2). Elderly The reduced clearance observed in elderly patients was primarily due to age-related decrease in renal clearance of ceftazidime. The mean elimination half-life ranged from 3.5 to 4 hours following single or 7 days repeat BID dosing of 2 g IV bolus injections in elderly patients 80 years or older. Paediatric population The half-life of ceftazidime is prolonged in preterm and term neonates by 4.5 to 7.5 hours after doses of 25 to 30 mg/kg. However, by the age of 2 months the half-life is within the range for adults.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
