Quest for the right Drug
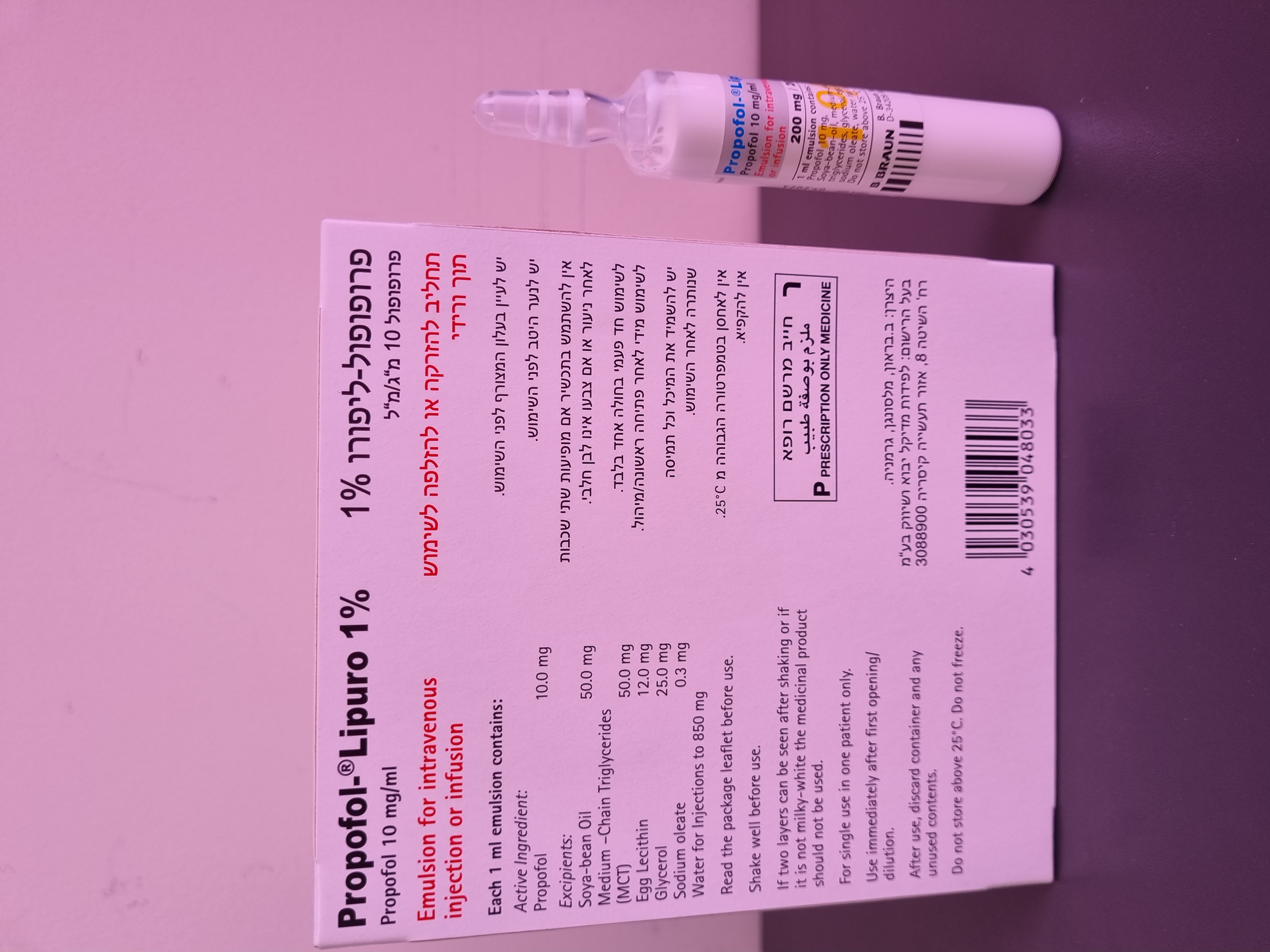
פרופופול ליפורו % 1 PROPOFOL - LIPURO 1 % (PROPOFOL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תחליב להזרקה או אינפוזיה : EMULSION FOR INJECTION OR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special Warnings and Precautions for Use Propofol should be given by those trained in anaesthesia (or, where appropriate, doctors trained in the care of patients in Intensive Care). Patients should be constantly monitored and facilities for maintenance of a patent airway, artificial ventilation, oxygen enrichment and other resuscitative facilities should be readily available at all times. Propofol should not be administered by the person conducting the diagnostic or surgical proce- dure. The abuse of and dependence on propofol, predominantly by health care professionals, have been re- ported. As with other general anaesthetics, the administration of propofol without airway care may re- sult in fatal respiratory complications. When propofol is administered for conscious sedation, for surgical and diagnostic procedures, pa- tients should be continually monitored for early signs of hypotension, airway obstruction and oxygen desaturation. As with other sedative agents, when propofol is used for sedation during operative procedures, invol- untary patient movements may occur. During procedures requiring immobility these movements may be hazardous to the operative site. An adequate period is needed prior to discharge of the patient to ensure full recovery after use of propofol. Very rarely the use of propofol may be associated with the development of a period of post- operative unconsciousness, which may be accompanied by an increase in muscle tone. This may or may not be preceded by a period of wakefulness. Although recovery is spontaneous, appropriate care of an unconscious patient should be administered. Propofol induced impairment is not generally detectable beyond 12 hours. The effects of propofol, the procedure, concomitant medications, the age and the condition of the patient should be considered when advising patients on: • The advisability of being accompanied on leaving the place of administration • The timing of recommencement of skilled or hazardous tasks such as driving • The use of other agents that may sedate (e.g. benzodiazepines, opiates, alcohol.) As with other intravenous anaesthetic agents, caution should be applied in patients with cardiac, res- piratory, renal or hepatic impairment or in hypovolaemic or debilitated patients. Propofol clearance is blood flow dependent, therefore, concomitant medication that reduces cardiac output will also reduce propofol clearance Propofol lacks vagolytic activity and has been associated with reports of bradycardia (occasionally profound) and also asystole. The intravenous administration of an anticholinergic agent before induc- tion or during maintenance of anaesthesia should be considered, especially in situations where vagal tone is likely to predominate or when propofol is used in conjunction with other agents likely to cause bradycardia. As with other intravenous anaesthetic and sedative agents, patients should be instructed to avoid alco- hol before and for at least 8 hours after administration of propofol. During bolus administration for operative procedures, extreme caution should be exercised in patients with acute pulmonary insufficiency or respiratory depression. Concomitant use of central nervous system depressants e.g., alcohol, general anaesthetics, narcotic analgesics will result in accentuation of their sedative effects. When propofol is combined with cen- trally depressant drugs administered parenterally, severe respiratory and cardiovascular depression may occur. It is recommended that propofol is administered following the analgesic and the dose should be carefully titrated to the patient's response . During induction of anaesthesia, hypotension and transient apnoea may occur depending on the dose and use of premedicants and other agents. Occasionally, hypotension may require use of intravenous fluids and reduction of the rate of admin- istration of propofol during the period of anaesthetic maintenance. When propofol is administered to an epileptic patient, there may be a risk of convulsion. Appropriate care should be applied in patients with disorders of fat metabolism and in other condi- tions where lipid emulsions must be used cautiously. As with other anaesthetics, sexual disinhibition may occur during recovery Paediatric population The use of propofol is not recommended in newborn infants as this patient population has not been fully investigated. Pharmacokinetic data (see section 5.2) indicate that clearance is considerably re- duced in neonates and has a very high inter-individual variability. Relative overdose could occur on administering doses recommended for older children and result in severe cardiovascular depression. Propofol must not be used in patients of 16 years of age or younger for sedation for intensive care as the safety and efficacy of propofol for sedation in this age group have not been demonstrated (see section 4.3). Advisory statements concerning Intensive Care Unit management Use of propofol for ICU sedation has been associated with a constellation of metabolic disturbances and system organ failures that may result in death. Reports have been received of combinations of the following: Metabolic acidosis, Rhabdomyolysis, Hyperkalaemia, Hepatomegaly, Renal failure, Hy- perlipidaemia, Cardiac arrhythmia, Brugada-type ECG (elevated ST-segment and coved T-wave) and rapidly progressive Cardiac failure usually unresponsive to inotropic supportive treatment. Combina- tions of these events have been referred to as the Propofol infusion syndrome. These events were mostly seen in patients with serious head injuries and children with respiratory tract infections who received dosages in excess of those advised in adults for sedation in the intensive care unit. The following appear to be the major risk factors for the development of these events: decreased oxy- gen delivery to tissues; serious neurological injury and/or sepsis; high dosages of one or more of the following pharmacological agents - vasoconstrictors, steroids, inotropes and/or propofol (at dose rates greater than 4 mg/kg/h for more than 48 hours). Prescribers should be alert to these events in patients with the above risk factors and promptly consid- er decreasing or stopping the propofol dosage when the above signs develop. All sedative and thera- peutic agents used in the intensive care unit (ICU), should be titrated to maintain optimal oxygen de- livery and haemodynamic parameters. Patients with raised intra-cranial pressure (ICP) should be giv- en appropriate treatment to support the cerebral perfusion pressure during these treatment modifica- tions. Treating physicians are reminded if possible not to exceed the dosage of 4 mg/kg/h. Appropriate care should be applied in patients with disorders of fat metabolism and in other conditions where lipid emulsions must be used cautiously. It is recommended that blood lipid levels should be monitored if propofol is administered to patients thought to be at particular risk of fat overload. Administration of propofol should be adjusted appropriately if the monitoring indicates that fat is being inadequately cleared from the body. If the patient is receiving other intravenous lipid concurrently, a reduction in quantity should be made in order to take account of the amount of lipid infused as part of the propofol formulation; 1.0 ml of Propofol-Lipuro 10 mg/ml contains 0.1 g of fat. Additional precautions Caution should be taken when treating patients with mitochondrial disease. These patients may be susceptible to exacerbations of their disorder when undergoing anaesthesia, surgery and ICU care. Maintenance of normothermia, provision of carbohydrates and good hydration are recommended for such patients. The early presentations of mitochondrial disease exacerbation and of the ‘propofol infusion syndrome’ may be similar. Propofol-Lipuro 1% contains no antimicrobial preservatives and supports growth of micro-organisms. When propofol is to be aspirated, it must be drawn aseptically into a sterile syringe or giving set im- mediately after opening the ampoule or breaking the vial seal. Administration must commence with- out delay. Asepsis must be maintained for both propofol and infusion equipment throughout the infu- sion period. Any infusion fluids added to the propofol line must be administered close to the cannula site. Propofol must not be administered via a microbiological filter. Propofol and any syringe containing propofol are for single use in an individual patient. In accordance with established guidelines for other lipid emulsions, a single infusion of propofol must not exceed 12 hours. At the end of the procedure or at 12 hours, whichever is the sooner, both the reservoir of propofol and the infusion line must be discarded and replaced as appropriate. This medicinal product contains less than 1 mmol (23 mg) sodium in 100 ml, i.e. essentially ‘sodium free’.
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
