Quest for the right Drug
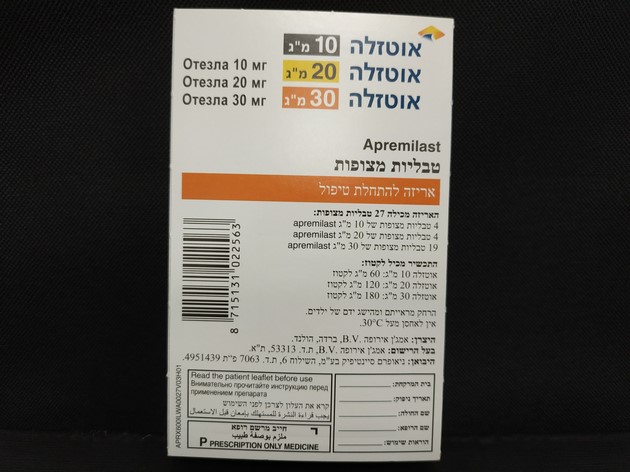
אוטזלה 10 מ"ג OTEZLA 10 MG (APREMILAST)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Immunosuppressants, selective immunosuppressants, ATC code: L04AA32 Mechanism of action Apremilast, an oral small-molecule inhibitor of phosphodiesterase 4 (PDE4), works intracellularly to modulate a network of pro-inflammatory and anti-inflammatory mediators. PDE4 is a cyclic adenosine monophosphate (cAMP)- specific PDE and the dominant PDE in inflammatory cells. PDE4 inhibition elevates intracellular cAMP levels, which in turn down-regulates the inflammatory response by modulating the expression of TNF-α, IL-23, IL-17 and other inflammatory cytokines. Cyclic AMP also modulates levels of anti-inflammatory cytokines such as IL-10. These pro- and anti-inflammatory mediators have been implicated in psoriatic arthritis and psoriasis. Pharmacodynamic effects In clinical studies in patients with psoriatic arthritis, apremilast significantly modulated, but did not fully inhibit, plasma protein levels of IL-1α, IL-6, IL-8, MCP-1, MIP-1β, MMP-3, and TNF-α. After 40 weeks of treatment with apremilast, there was a decrease in plasma protein levels of IL-17 and IL-23, and an increase in IL-10. In clinical studies in patients with psoriasis, apremilast decreased lesional skin epidermal thickness, inflammatory cell infiltration, and expression of pro-inflammatory genes, including those for inducible nitric oxide synthase (iNOS), IL-12/IL-23p40, IL-17A, IL-22 and IL-8. Apremilast administered at doses of up to 50 mg twice daily did not prolong the QT interval in healthy subjects. Clinical efficacy and safety Psoriatic Arthritis The safety and efficacy of apremilast were evaluated in 3 multi-center, randomized, double-blind, placebo-controlled studies (Studies PALACE 1, PALACE 2, and PALACE 3) of similar design in adult patients with active PsA (≥ 3 swollen joints and ≥ 3 tender joints) despite prior treatment with small molecule or biologic DMARDs. A total of 1493 patients were randomized and treated with either placebo, apremilast 20 mg or apremilast 30 mg given orally twice daily. Patients in these studies had a diagnosis of PsA for at least 6 months. One qualifying psoriatic skin lesion (at least 2 cm in diameter) was also required in PALACE 3. Apremilast was used as a monotherapy (34.8%) or in combination with stable doses of small molecule DMARDs (65.2%). Patients received apremilast in combination with one or more of the following: methotrexate (MTX, ≤ 25 mg/week, 54.5%), sulfasalazine (SSZ, ≤ 2 g/day, 9.0%), and leflunomide (LEF; ≤ 20 mg/day, 7.4%). Concomitant treatment with biologic DMARDs, including TNF blockers, was not allowed. Patients with each subtype of PsA were enrolled in the 3 studies, including symmetric polyarthritis (62.0%), asymmetric oligoarthritis (26.9%), distal interphalangeal (DIP) joint arthritis (6.2%), arthritis mutilans (2.7%), and predominant spondylitis (2.1%). Patients with pre-existing enthesopathy (63%) or pre-existing dactylitis (42%) were enrolled. A total of 76.4% of patients were previously treated with only small-molecule DMARDs and 22.4% of patients were previously treated with biologic DMARDs, which includes 7.8% who had a therapeutic failure with a prior biologic DMARD. The median duration of PsA disease was 5 years. Based on the study design, patients whose tender and swollen joint counts had not improved by at least 20% were considered non-responders at week 16. Placebo patients who were considered non-responders were re-randomized 1:1 in a blinded fashion to either apremilast 20 mg twice daily or 30 mg twice daily. At week 24, all remaining placebo-treated patients were switched to either apremilast 20 or 30 mg twice daily Following 52 weeks of treatment, patients could continue on open-label apremilast 20 mg or 30 mg within the long-term extension of the PALACE 1, PALACE 2, and PALACE 3 studies for a total duration of treatment up to 5 years (260 weeks). The primary endpoint was the percentage of patients achieving American College of Rheumatology (ACR) 20 response at week 16. Treatment with apremilast resulted in significant improvements in the signs and symptoms of PsA, as assessed by the ACR 20 response criteria compared to placebo at weeks 16. The proportion of patients with ACR 20/50/70(responses in Studies PALACE 1, PALACE 2 and PALACE 3, and the pooled data for studies PALACE 1, PALACE 2 and PALACE 3, for apremilast 30 mg twice daily at week 16, are shown in Table 3. ACR 20/50/70 responses were maintained at week 24. Among patients who were initially randomized to apremilast 30 mg twice daily treatment, ACR 20/50/70 response rates were maintained through week 52 in the pooled Studies PALACE 1, PALACE 2 and PALACE 3 (Figure 1). Table 3. Proportion of patients with ACR responses in studies PALACE 1, PALACE 2 and PALACE 3 and pooled studies at week 16 PALACE 1 PALACE 2 PALACE 3 POOLED Placebo Apremilast Placebo Apremilast Placebo Apremilast Placebo Apremilast 30 mg twice 30 mg twice 30 mg twice 30 mg twice +/- daily +/- daily +/- daily +/- daily DMARDs +/- DMARDs +/- DMARDs +/- DMARDs +/- N=168 DMARDs N=159 DMARDs N=169 DMARDs N=496 DMARDs Na N=168 N=162 N=167 N=497 ACR 20a Week 19.0% 38.1%** 18.9% 32.1%* 18.3% 40.7%** 18.8% 37.0%** 16 ACR 50 Week 6.0% 16.1%* 5.0% 10.5% 8.3% 15.0% 6.5% 13.9%** 16 ACR 70 Week 1.2% 4.2% 0.6% 1.2% 2.4% 3.6% 1.4% 3.0% 16 *p ≤ 0.01 for apremilast vs. placebo. **p ≤ 0.001 for apremilast vs. placebo a N is the number of patients as randomized and treated. Figure 1 Proportion of ACR 20/50/70 responders through week 52 in the pooled analysis of studies PALACE 1, PALACE 2 and PALACE 3 (NRI*) *NRI: None responder imputation. Subjects who discontinued early prior to the time point and subjects who did not have sufficient data for a definitive determination of response status at the time point are counted as non-responders. Among 497 patients initially randomized to apremilast 30 mg twice daily, 375 (75%) patients were still on this treatment on week 52. In these patients, ACR 20/50/70 responses at week 52 were of 57%, 25%, and 11% respectively. Among 497 patients initially randomized to apremilast 30 mg twice daily, 375 (75%) patients entered the long-term extension studies, and of these, 221 patients (59%) were still on this treatment at week 260. ACR responses were maintained in the long-term open label extension studies for up to 5 years. Responses observed in the apremilast treated group were similar in patients receiving and not receiving concomitant DMARDs, including MTX. Patients previously treated with DMARDs or biologics who received apremilast achieved a greater ACR 20 response at week 16 than patients receiving placebo. Similar ACR responses were observed in patients with different PsA subtypes, including DIP. The number of patients with arthritis mutilans and predominant spondylitis subtypes was too small to allow meaningful assessment. In PALACE 1, PALACE 2 and PALACE 3, improvements in Disease Activity Scale (DAS) 28 C-reactive protein (CRP) and in the proportion of patients achieving a modified PsA response criteria (PsARC) were greater in the apremilast group, compared to placebo at week 16 (nominal p-value p< 0.0004, p-value ≤0.0017, respectively). These improvements were maintained at week 24. Among patients who remained on the apremilast treatment to which they were randomized at study start, DAS28(CRP) score and PsARC response were maintained through week 52. At weeks 16 and 24 improvements in parameters of peripheral activity characteristic of psoriatic arthritis (e.g. number of swollen joints, number of painful/tender joints, dactylitis and enthesitis) and in the skin manifestations of psoriasis were seen in the apremilast-treated patients. Among patients who remained on the apremilast treatment to which they were randomized at study start, these improvements were maintained through week 52. The clinical responses were maintained in the same parameters of peripheral activity and in the skin manifestations of psoriasis in the open-label extension studies for up to 5 years of treatment. Physical function and health-related quality of life Apremilast-treated patients demonstrated statistically significant improvement in physical function, as assessed by the disability index of the health assessment questionnaire (HAQ-DI) change from baseline, compared to placebo at weeks 16 in PALACE 1, PALACE 2 and PALACE 3 and in the pooled studies. Improvement in HAQ-DI scores was maintained at week 24. Among patients who were initially randomized to apremilast 30 mg twice daily treatment, the change from baseline in the HAQ-DI score at week 52 was -0.333 in the apremilast 30 mg twice daily group in a pooled analysis of the open-label phase of studies PALACE 1, PALACE 2 and PALACE 3. In studies PALACE 1, PALACE 2 and PALACE 3, significant improvements were demonstrated in health-related quality of life, as measured by the changes from baseline in the physical functioning (PF) domain of the Short Form Health Survey version 2 (SF-36v2), and in the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT- fatigue) scores in patients treated with apremilast compared to placebo at weeks 16 and 24. Among patients who remained on the apremilast treatment, to which they were initially randomized at study start, improvement in physical function and FACIT- fatigue was maintained through week 52. Improved physical function as assessed by the HAQ-DI and the SF36v2PF domain, and the FACIT-fatigue scores were maintained in the open-label extension studies for up to 5 years of treatment. Psoriasis The safety and efficacy of apremilast were evaluated in two multicenter, randomized, double-blind, placebo- controlled studies (Studies ESTEEM 1 and ESTEEM 2) which enrolled a total of 1257 patients with moderate to severe plaque psoriasis who had a body surface area (BSA) involvement of ≥ 10%, Psoriasis Area and Severity Index (PASI) score ≥ 12, static Physician Global Assessment (sPGA) of ≥ 3 (moderate or severe), and who were candidates for phototherapy or systemic therapy. These studies had a similar design through week 32. In both studies, patients were randomized 2:1 to apremilast 30 mg twice daily or placebo for 16 weeks (placebo-controlled phase) and from weeks 16-32, all patients received apremilast 30 mg twice daily (maintenance phase). During the Randomized Treatment Withdrawal Phase (weeks 32- 52), patients originally randomized to apremilast who achieved at least a 75% reduction in their PASI score (PASI- 75) (ESTEEM 1) or a 50% reduction in their PASI score (PASI-50) (ESTEEM 2) were re-randomized at week 32 to either placebo or apremilast 30 mg twice daily. Patients who were re-randomized to placebo and who lost PASI-75 response (ESTEEM 1) or lost 50% of the PASI improvement at week 32 compared to baseline (ESTEEM 2) were retreated with apremilast 30 mg twice daily. Patients who did not achieve the designated PASI response by week 32, or who were initially randomized to placebo, remained on apremilast until week 52. The use of low potency topical corticosteroids on the face, axillae, and groin, coal tar shampoo and/or salicylic acid scalp preparations was permitted throughout the studies. In addition, at week 32, subjects who did not achieve a PASI-75 response in ESTEEM 1, or a PASI-50 response in ESTEEM 2, were permitted to use topical psoriasis therapies and/or phototherapy in addition to apremilast 30 mg twice daily treatment. Following 52 weeks of treatment, patients could continue on open-label apremilast 30 mg within the long-term extension of the ESTEEM 1 and ESTEEM 2 studies for a total duration of treatment up to 5 years (260 weeks). In both studies, the primary endpoint was the proportion of patients who achieved PASI-75 at week 16. The major secondary endpoint was the proportion of patients who achieved a sPGA score of clear (0) or almost clear (1) at week 16. The mean baseline PASI score was 19.07 (median 16.80), and the proportion of patients with sPGA score of 3 (moderate) and 4 (severe) at baseline was 70.0% and 29.8%, respectively with a mean baseline BSA involvement of 25.19% (median 21.0%). Approximately 30% of all patients had received prior phototherapy and 54% had received prior conventional systemic and/or biologic therapy for the treatment of psoriasis (including treatment failures), with 37% receiving prior conventional systemic therapy and 30% receiving prior biologic therapy. Approximately one- third of patients had not received prior phototherapy, conventional systemic or biologic therapy. A total of 18% of patients had a history of psoriatic arthritis. The proportion of patients achieving PASI-50, -75 and -90 responses, and sPGA score of clear (0) or almost clear (1), are presented in Table 4 below. Treatment with apremilast resulted in significant improvement in moderate to severe plaque psoriasis as demonstrated by the proportion of patients with PASI-75 response at week 16, compared to placebo. Clinical improvement measured by sPGA, PASI-50 and PASI-90 responses were also demonstrated at week 16. In addition, apremilast demonstrated a treatment benefit across multiple manifestations of psoriasis including pruritus, nail disease, scalp involvement and quality of life measures. Table 4. Clinical response at week 16 in studies ESTEEM 1 and ESTEEM 2 (FAS a, LOCFb) ESTEEM 1 ESTEEM 2 Placebo 30 mg twice daily Placebo 30 mg twice daily APR* APR* N 282 562 137 274 PASIc 75, n (%) 15 (5.3) 186 (33.1) 8 (5.8) 79 (28.8) sPGAd of Clear or 11 (3.9) 122 (21.7) 6 (4.4) 56 (20.4) Almost Clear, n (%) PASI 50, n (%) 48 (17.0) 330 (58.7) 27 (19.7) 152 (55.5) PASI 90, n (%) 1 (0.4) 55 (9.8) 2 (1.5) 24 (8.8) Percent Change - 6.9 - 47.8 - 6.1 -48.4 BSAe (%) ± 38.95 ± 38.48 ± 47.57 ± 40.78 mean ± SD Change in - 7.3 - 31.5 - 12.2 - 33.5 Pruritus VASf ± 27.08 ± 32.43 ± 30.94 ±35.46 (mm), mean ± SD Change in DLQIg, - 2.1 - 6.6 -2.8 -6.7 mean ± SD ± 5.69 ± 6.66 ± 7.22 ± 6.95 Change in SF-36 - 1.02 2.39 0.00 ±10.498 2.58 MCS h, mean ± SD ± 9.161 ± 9.504 ± 10.129 * p< 0.0001 for apremilast vs placebo, except for ESTEEM 2 PASI 90 and Change in SF-36 MCS where p=0.0042 and p=0.0078, respectively. a FAS = Full Analysis Set b LOCF = Last Observation Carried Forward c PASI = Psoriasis Area and Severity Index d sPGA = Static Physician Global Assessment e BSA = Body Surface Area f VAS = Visual Analog Scale; 0 = best, 100 = worst g DLQI = Dermatology Life Quality Index; 0 = best, 30 = worst h SF-36 MCS = Medical Outcome Study Short Form 36-Item Health Survey, Mental Component Summary The clinical benefit of apremilast was demonstrated across multiple subgroups defined by baseline demographics and baseline clinical disease characteristics (including psoriasis disease duration and patients with a history of psoriatic arthritis). The clinical benefit of apremilast was also demonstrated regardless of prior psoriasis medication usage and response to prior psoriasis treatments. Similar response rates were observed across all weight ranges. Response to apremilast was rapid, with significantly greater improvements in the signs and symptoms of psoriasis, including PASI, skin discomfort/pain and pruritus, compared to placebo by week 2. In general, PASI responses were achieved by week 16 and were maintained through week 32. In both studies, the mean percent improvement in PASI from baseline remained stable during the Randomized Treatment Withdrawal Phase for patients re-randomized to apremilast at week 32 (Table 5). Table 5. Persistence of effect among subjects randomized to APR 30 twice daily at week 0 and re-randomized to APR 30 twice daily at week 32 to week 52 Time Point ESTEEM 1 ESTEEM 2 Patients who achieved Patients who achieved PASI-75 at Week 32 PASI-50 at Week 32 Percent Change in PASI Week 16 -77.7 ± 20.30 -69.7 ± 24.23 from baseline, mean (%) Week 32 -88 ± 8.30 -76.7 ± 13.42 ± SDa Week 52 -80.5 ± 12.60 -74.4 ± 18.91 Change in DLQI from Week 16 -8.3 ± 6.26 -7.8 ± 6.41 baseline, mean ± SDa Week 32 -8.9 ± 6.68 -7.7 ± 5.92 Week 52 -7.8 ± 5.75 -7.5 ± 6.27 Proportion of subjects Week 16 40/48 (83.3) 21/37 (56.8) with Scalp Psoriasis PGA Week 32 39/48 (81.3) 27/37 (73.0) (ScPGA) 0 or 1, n/N (%)b Week 52 35/48 (72.9) 20/37 (54.1) Includes subjects re-randomized to APR 30 twice daily at week 32 with a baseline value and a post-baseline value at the evaluated study week. a b N is based on subjects with moderate or greater scalp psoriasis at baseline who were re-randomized to APR 30 twice daily at week 32. Subjects with missing data were counted as non-responders. In Study ESTEEM 1, approximately 61% of patients re-randomized to apremilast at week 32 had a PASI-75 response at week 52. Of the patients with at least a PASI-75 response who were re-randomized to placebo at week 32 during a Randomized Treatment Withdrawal Phase, 11.7% were PASI-75 responders at week 52. The median time to loss of PASI-75 response among the patients re-randomized to placebo was 5.1 weeks. In Study ESTEEM 2, approximately 80.3% of patients re-randomized to apremilast at week 32 had a PASI-50 response at week 52. Of the patients with at least a PASI-50 response who were re-randomized to placebo at week 32, 24.2% were PASI-50 responders at week 52. The median time to loss of 50% of their week 32 PASI improvement was 12.4 weeks. After randomized withdrawal from therapy at week 32, approximately 70% of patients in Study ESTEEM 1, and 65.6% of patients in Study ESTEEM 2, regained PASI-75 (ESTEEM 1) or PASI-50 (ESTEEM 2) responses after re- initiation of apremilast treatment. Due to the study design the duration of re-treatment was variable, and ranged from 2.6 to 22.1 weeks. In Study ESTEEM 1, patients randomized to apremilast at the start of the study who did not achieve a PASI-75 response at week 32 were permitted to use concomitant topical therapies and/or UVB phototherapy between weeks 32 to 52. Of these patients, 12% achieved a PASI-75 response at week 52 with apremilast plus topical and/or phototherapy treatment. In Studies ESTEEM 1 and ESTEEM 2, significant improvements (reductions) in nail psoriasis, as measured by the mean percent change in Nail Psoriasis Severity Index (NAPSI) from baseline, were observed in patients receiving apremilast compared to placebo-treated patients at week 16 (p< 0.0001 and p=0.0052, respectively). Further improvements in nail psoriasis were observed at week 32 in patients continuously treated with apremilast. In Studies ESTEEM 1 and ESTEEM 2, significant improvements in scalp psoriasis of at least moderate severity (≥3), measured by the proportion of patients achieving Scalp Psoriasis Physician’s Global Assessment (ScPGA) of clear (0) or minimal (1) at week 16, were observed in patients receiving apremilast compared to placebo-treated patients (p< 0.0001 for both studies). The improvements were generally maintained in subjects who were re- randomized to apremilast at week 32 through week 52 (Table 5). In Studies ESTEEM 1 and ESTEEM 2, significant improvements in quality of life as measured by the Dermatology Life Quality Index (DLQI) and the SF-36v2MCS were demonstrated in patients receiving apremilast compared with placebo-treated patients (Table 4). Improvements in DLQI were maintained through week 52 in subjects who were re-randomized to apremilast at week 32 (Table 5). In addition, in Study ESTEEM 1, significant improvement in the Work Limitations Questionnaire (WLQ-25) Index was achieved in patients receiving apremilast compared to placebo. Among 832 patients initially randomized to apremilast 30 mg twice daily, 443 patients (53%) entered the open-label extension studies of ESTEEM 1 and ESTEEM 2, and of these 115 patients (26%) were still on treatment at week 260. For patients who remained on apremilast in the open-label extension of ESTEEM 1 and ESTEEM 2 studies, improvements were generally maintained in PASI score, affected BSA, itch, nail and quality of life measures for up to 5 years. The long-term safety of apremilast 30 mg twice daily in patients with psoriatic arthritis and psoriasis was assessed for a total duration of treatment up to 5 years. Long-term experience in open-label extension studies with apremilast was generally comparable to the 52-week studies. Oral Ulcers Associated with Behçet’s disease A multicenter, randomized, placebo-controlled trial (BCT-002) enrolled a total of 207 adult patients with BD with active oral ulcers. Patients were previously treated with at least one nonbiologic BD medication and were candidates for systemic therapy. Patients met the International Study Group (ISG) Criteria for BD. Patients had at least 2 oral ulcers at screening and at least 2 oral ulcers at randomization and without currently active major organ involvement. Concomitant treatment for BD was not allowed. Patients were randomized 1:1 to receive either apremilast 30 mg twice daily (n=104) or placebo (n=103) for 12 weeks. After week 12, all patients received apremilast 30 mg twice daily. Efficacy was assessed based on the number and pain of oral ulcers. Patients ranged in age from 19 to 72, with a mean age of 40 years. The mean duration of BD was 6.84 years. All subjects had a history of recurrent oral ulcers that were currently active. Subjects had a history of skin lesions (98.6%), genital ulcers (90.3%), musculoskeletal manifestations (72.5%), ocular manifestations (17.4%), central nervous system (9.7%), gastrointestinal (GI) manifestations (9.2%) and vascular involvement (1.4%). The mean baseline oral ulcer counts were 4.2 and 3.9 in the apremilast and placebo groups, respectively. Measures of Oral Ulcers Improvements in measures of oral ulcers at week 12 are presented in Table 6. Table 6: Clinical Response of Oral Ulcers at Week 12 in the BCT-002 Study (ITTa Population) OTEZLA Treatmentb Placebo Difference 30 mg twice daily Endpoint N=103 (95% CIc) N=104 Changed from baseline in the pain of -24.1 oral ulcers as measured by VASe at -18.7 - 42.7 week 12 (-32.4, -15.7) Proportionf of subjects achieving oral 52.9% 30.6%g ulcer complete response (oral ulcer-free) 22.3% (18.1%, at week 12 43.1%) Proportionf of subjects achieving oral ulcer complete response (oral ulcer-free) 25.1%g by week 6, and who remained oral ulcer-free for at least 6 additional weeks 4.9% 29.8% (15.5%, during the 12-week Placebo-controlled 34.6%) Treatment Phase Daily averageh,i number of oral ulcers -1.1 during the 12-week Placebo-controlled 2.6 1.5 Treatment Phase (-1.6, -0.7) a ITT=intent to treat. b OTEZLA – Placebo. c CI=confidence interval. d Mean changes from baseline are least square means from mixed-effects model for repeated measures, adjusting for sex, region, and baseline pain of oral ulcers as measured by the visual analog scale. e VAS=visual analog scale; 0=no pain, 100=worst possible pain. f Patients for whom data are not available to determine response status are considered non-responders. g Adjusted difference in proportions is the weighted average of the treatment differences across the 4 strata of combined sex and region factors with the Cochran- Mantel-Haenszel weights. h Mean daily averages are least squares means from analysis of covariance, after adjusting for sex, region, and baseline number of oral ulcers. i Based on oral ulcer counts measured at baseline and at weeks 1, 2, 4, 6, 8, 10, and 12. Figure 2 displays the mean number of oral ulcers for each treatment group at each visit, while Figure 3 displays the mean oral ulcer pain on a visual analog scale for each treatment group at each visit. Figure 2: Mean (± SE) Number of Oral Ulcers by Time Point Through Week 12 (ITT Population) ITT = intent-to-treat; SE = standard error. Figure 3: Mean (± SE) Oral Ulcer Pain on a Visual Analog Scale by Time Point Through Week 12 (ITT Population) ITT=intent-to-treat; SE=standard error. Oral ulcer pain was assessed on a 100-mm Visual Analog Scale with 0 = no pain and 100 = worst possible pain. Mean baseline Visual Analog Scale pain scores were 61.2 and 60.8 in the OTEZLA 30 mg twice daily treatment group and placebo treatment group, respectively.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Apremilast is well absorbed with an absolute oral bioavailability of approximately 73%, with peak plasma concentrations (Cmax) occurring at a median time (t max) of approximately 2.5 hours. Apremilast pharmacokinetics are linear, with a dose-proportional increase in systemic exposure in the dose range of 10 to 100 mg daily. Accumulation is minimal when apremilast is administered once daily and approximately 53% in healthy subjects and 68% in patients with psoriasis when administered twice daily. Co-administration with food does not alter the bioavailability therefore, apremilast can be administered with or without food. Distribution Human plasma protein binding of apremilast is approximately 68%. The mean apparent volume of distribution (V d) is 87 L, indicative of extravascular distribution. Biotransformation Apremilast is extensively metabolized by both CYP and non-CYP mediated pathways including oxidation, hydrolysis, and conjugation, suggesting inhibition of a single clearance pathway is not likely to cause a marked drug- drug interaction. Oxidative metabolism of apremilast is primarily mediated by CYP3A4, with minor contributions from CYP1A2 and CYP2A6. Apremilast is the major circulating component following oral administration. Apremilast undergoes extensive metabolism with only 3% and 7% of the administered parent compound recovered in urine and feces, respectively. The major circulating inactive metabolite is the glucuronide conjugate of O- demethylated apremilast (M12). Consistent with apremilast being a substrate of CYP3A4, apremilast exposure is decreased when administered concomitantly with rifampicin, a strong inducer of CYP3A4. In vitro, apremilast is not an inhibitor or inducer of cytochrome P450 enzymes. Hence, apremilast co-administered with substrates of CYP enzymes is unlikely to affect the clearance and exposure of active substances that are metabolized by CYP enzymes. In vitro, apremilast is a substrate, and a weak inhibitor of P-glycoprotein (IC50>50 µM), however clinically relevant drug interactions mediated via P-gp are not expected to occur. In vitro, apremilast has little to no inhibitory effect (IC50>10 µM) on Organic Anion Transporter (OAT)1 and OAT3, Organic Cation Transporter (OCT)2, Organic Anion Transporting Polypeptide (OATP)1B1 and OATP1B3, or breast cancer resistance protein (BCRP) and is not a substrate for these transporters. Hence, clinically relevant drug-drug interactions are unlikely when apremilast is co-administered with drugs that are substrates or inhibitors of these transporters. Elimination The plasma clearance of apremilast is on average about 10 L/hr in healthy subjects, with a terminal elimination half- life of approximately 9 hours. Following oral administration of radiolabelled apremilast, about 58% and 39% of the radioactivity is recovered in urine and feces, respectively, with about 3% and 7% of the radioactive dose recovered as apremilast in urine and feces, respectively. Elderly patients Apremilast was studied in young and elderly healthy subjects. The exposure in elderly subjects (65 to 85 years of age) is about 13% higher in AUC and about 6% higher in C max for apremilast than that in young subjects (18 to 55 years of age). There is limited pharmacokinetic data in subjects over 75 years of age in clinical trials. No dosage adjustment is necessary for elderly patients. Renal impairment There is no meaningful difference in the PK of apremilast between mild or moderate renally impaired subjects and matched healthy subjects (N = 8 each). The results support that no dose adjustment is needed in patients with mild and moderate renal impairment. Apremilast dose should be reduced to 30 mg once daily in patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2 or CLcr < 30 mL/min). In 8 subjects with severe renal impairment to whom a single dose of 30 mg apremilast was administered, the AUC and C max of apremilast increased by approximately 89% and 42%, respectively. Hepatic impairment The pharmacokinetics of apremilast and its major metabolite M12 are not affected by moderate or severe hepatic impairment. No dose adjustment is necessary for patients with hepatic impairment.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול במקרים האלה:1. חולה בוגר הסובל מדלקת מפרקים פסוריאטית (Psoriatic arthritis), לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs.2. חולה בוגר הסובל מפסוריאזיס, לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs ו/או PUVA ו/או Psoralen.3. טיפול בכיבים בחלל הפה בחולי בכצ'ט אחרי מיצוי טיפול בקולכיצין.ב. התכשיר לא יינתן בשילוב עם תכשירים ביולוגיים.ג. מתן התכשיר יינתן לחולה בהתאם למרשם של מומחה ברפואת עור ומין או מומחה בראומטולוגיה או מומחה בגסטרואנטרולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| כיבים בחלל הפה בחולי בכצ'ט אחרי מיצוי טיפול בקולכיצין | 01/03/2021 | ראומטולוגיה | Behcet disease | |
| מפסוריאזיס, לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs ו/או PUVA ו/או Psoralen | 12/01/2017 | עור ומין | Psoriasis | |
| דלקת מפרקים פסוריאטית (Psoriatic arthritis), לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs. | 15/01/2015 | ראומטולוגיה | Psoriatic arthritis |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
