Quest for the right Drug
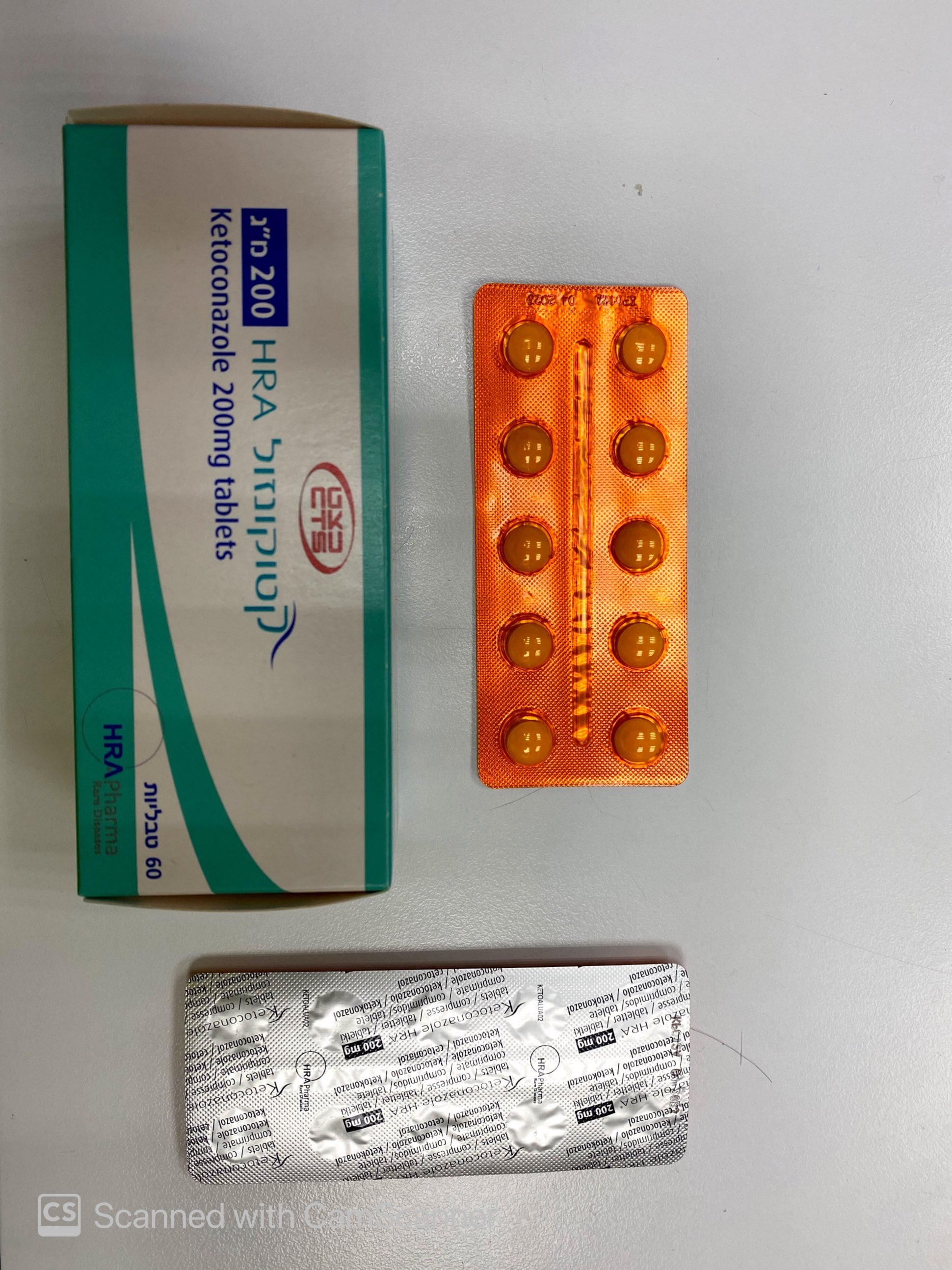
קטוקונזול HRA 200 מ"ג KETOCONAZOLE HRA 200 MG (KETOCONAZOLE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most frequent adverse reactions are adrenal insufficiency, nausea, vomiting, abdominal pain, diarrhoea, pruritus, rash and the hepatic enzymes increased. The most serious adverse reaction is hepatotoxicity, primarily as acute hepatocellular toxicity, but may also result in cholestatic injury or a mixed pattern of toxicity. ASAT, ALAT, gammaGT, bilirubin and alkaline phosphatase should be monitored at frequent intervals during treatment (see sections 4.2 and 4.4). Tabulated list of adverse reactions The safety of ketoconazole has been evaluated based on published literature and use of ketoconazole as an antifungal treatment. The adverse reactions listed below in table 2 are classified according to System Organ Class. Frequency groupings are defined according to the following convention: very common (≥ 1/10) , common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), not known cannot be estimated from the available data. Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness. Table 2: Incidence of adverse reactions and marked laboratory abnormalities reported in the literature in adults and adolescents patients System organ class Frequency Adverse reaction Blood and lymphatic Uncommon Thrombocytopenia system disorders Immune system Uncommon Allergic conditions including anaphylactic disorders shock, anaphylactoid reaction and anaphylactic reaction and angioedema Endocrine disorders Common Adrenal insufficiency Metabolism and Not known Alcohol intolerance, anorexia, increased nutrition disorders appetite Psychiatric Not known Insomnia, nervousness disorders Nervous system Uncommon Headache, dizziness, somnolence disorders Not known Intracranial pressure increased (papilloedema, fontanelle bulging), paraesthesia Eye disorders Not known Photophobia Respiratory, Not known Epistaxis thoracic and mediastinal disorders Gastrointestinal Common Nausea, abdominal pain, vomiting, disorders diarrhoea Not known Dyspepsia, flatulence, tongue discoloration, dry mouth, dysgeusia Hepatobiliary Very common Liver function tests abnormal disorders Rare Serious hepatotoxicity, including jaundice, hepatitis, hepatic necrosis, hepatic cirrhosis, hepatic failure including cases necessitating transplantation or resulting in death. (see 4.4 Special warnings and special precautions for use) Skin and Common Pruritus, rash subcutaneous tissue disorders Uncommon Urticaria, alopecia Not known Photosensitivity, erythema multiforme, dermatitis, erythema, xeroderma Musculoskeletal and Not known Myalgia, arthralgia connective tissue disorder Reproductive system Not known Menstrual disorder, azoospermia, erectile and breast disorders dysfunction, gynaecomastia General disorders Uncommon Asthenia and administration site conditions Very rare Pyrexia Not known Oedema peripheral, malaise, hot flush Investigations Very common Hepatic enzyme increased Uncommon Platelet count decreased Not known Transient decrease of testosterone concentrations Description of selected adverse reactions Hepatotoxicity Serious hepatic toxicity caused by ketoconazole treatment is rare (1/15000). Acute hepatocellular injury has been primarily observed as has cholestatic injury or a mixed pattern of toxicity. Fatal cases have been reported particularly when treatment is continued despite liver enzyme elevation. Increases in liver enzymes (5N and > 5N) were observed in ~13.5 % and ~2.5% of patients respectively occurring mostly within the first 6 months of treatment. Liver enzyme levels returned to normal within 2-12 weeks after a dose decrease or withdrawal of ketoconazole. Hepatotoxicity does not appear to be dose dependent. All potential associated factors of hepatotoxicity, and abnormal liver enzyme levels detected before ketoconazole initiation, should be taken into account before considering ketoconazole treatment. Ketoconazole should not be administered when liver enzymes are greater than 2 times the upper limit of normal or in association with other hepatotoxic medicinal products. Liver enzyme monitoring should be performed once weekly during the first month of treatment and then monthly for 6 months. In the case an increase of liver enzymes is detected which is less than 3 times the upper limit of normal, closer monitoring of liver function should be performed and the daily dose should be decreased by at least 200 mg. In the case of increase of liver enzymes levels above 3 times the upper limit of normal, Ketoconazole should be stopped immediately and should not be reintroduced because of the risk of serious hepatic toxicity. Adrenal insufficiency Adrenal insufficiency may occur in patients on ketoconazole without corticosteroid substitution (block-only regimen) or if there is an insufficient glucocorticoid replacement therapy (for the patients treated with a block- and-replace regimen). Monitor and instruct patients on the signs and symptoms associated with hypocortisolism (e.g. weakness, fatigue, anorexia, nausea, vomiting, hypotension, hyperkalemia, hyponatraemia, hyperkalaemia or hypoglycaemia). Adrenal insufficiency may be detected by periodic clinical assessment and monitoring of plasma/serum or salivary cortisol levels. In case of adrenal insufficiency, Ketoconazole HRA treatment should be temporarily discontinued or the dose reduced and, if needed, a corticosteroid substitution therapy added. Paediatric population Frequency of hepatotoxicity could be higher in adolescents than in adults. In the literature, among 24 paediatric patients treated with ketoconazole, two developed severe hepatoxicity. A 14 year-old girl who was treated for Cushing’s disease with ketoconazole 200 mg twice daily presented one month later with jaundice, fever anorexia, nausea and vomiting. Ketoconazole was stopped, but she deteriorated rapidly and died. A 17 years old girl was treated on ketoconazole 1,200 mg/day for an adrenal carcinoma with liver metastasis and had altered liver function tests at 22 days. After ketoconazole withdrawal, liver enzymes returned to normal levels within 3 weeks (section 5.1). Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the national regulation by using an online form https://sideeffects.health.gov.il/.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
