Quest for the right Drug
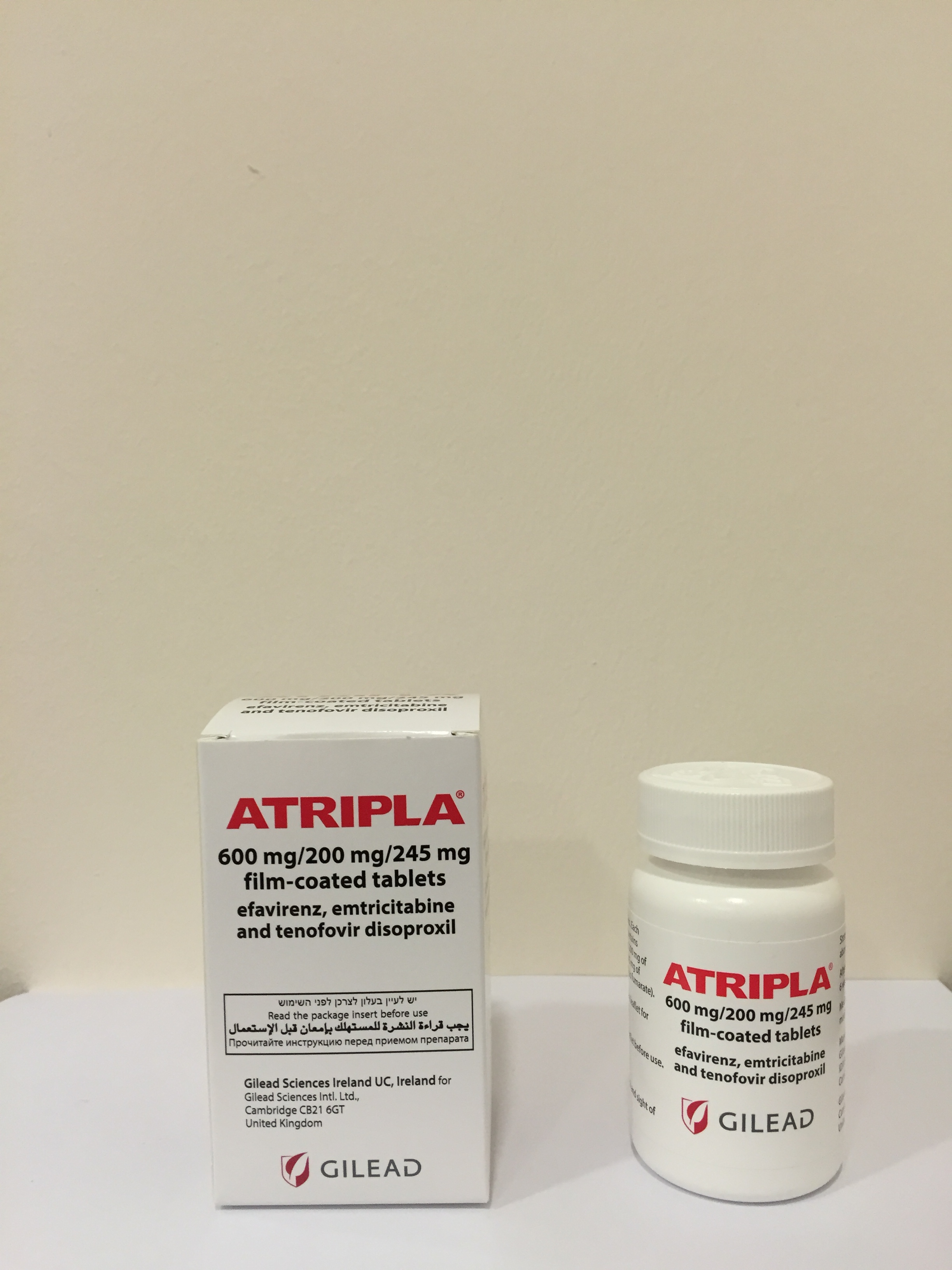
אטריפלה ATRIPLA (EFAVIRENZ, EMTRICITABINE, TENOFOVIR DISOPROXIL AS)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antiviral for systemic use, antivirals for treatment of HIV infections, combinations, ATC code: J05AR06 Mechanism of action and pharmacodynamic effects Efavirenz is an NNRTI of HIV-1. Efavirenz non-competitively inhibits HIV-1 reverse transcriptase (RT) and does not significantly inhibit human immunodeficiency virus-2 (HIV-2) RT or cellular deoxyribonucleic acid (DNA) polymerases (α, β, γ, and δ). Emtricitabine is a nucleoside analogue of cytidine. Tenofovir disoproxil is converted in vivo to tenofovir, a nucleoside monophosphate (nucleotide) analogue of adenosine monophosphate. Emtricitabine and tenofovir are phosphorylated by cellular enzymes to form emtricitabine triphosphate and tenofovir diphosphate, respectively. In vitro studies have shown that both emtricitabine and tenofovir can be fully phosphorylated when combined together in cells. Emtricitabine triphosphate and tenofovir diphosphate competitively inhibit HIV-1 reverse transcriptase, resulting in DNA chain termination. Both emtricitabine triphosphate and tenofovir diphosphate are weak inhibitors of mammalian DNA polymerases and there was no evidence of toxicity to mitochondria in vitro and in vivo. Cardiac Electrophysiology The effect of efavirenz on the QTc interval was evaluated in an open-label, positive and placebo controlled, fixed single sequence 3-period, 3-treatment crossover QT study in 58 healthy subjects enriched for CYP2B6 polymorphisms. The mean Cmax of efavirenz in subjects with CYP2B6 *6/*6 genotype following the administration of 600 mg daily dose for 14 days was 2.25-fold the mean Cmax observed in subjects with CYP2B6 *1/*1 genotype. A positive relationship between efavirenz concentration and QTc prolongation was observed. Based on the concentration-QTc relationship, the mean QTc prolongation and its upper bound 90% confidence interval are 8.7 ms and 11.3 ms in subjects with CYP2B6*6/*6 genotype following the administration of 600 mg daily dose for 14 days (see section 4.5). Antiviral activity in vitro Efavirenz demonstrated antiviral activity against most non-clade B isolates (subtypes A, AE, AG, C, D, F, G, J, and N) but had reduced antiviral activity against group O viruses. Emtricitabine displayed antiviral activity against HIV-1 clades A, B, C, D, E, F, and G. Tenofovir displayed antiviral activity against HIV-1 clades A, B, C, D, E, F, G, and O. Both emtricitabine and tenofovir showed strain specific activity against HIV-2 and antiviral activity against HBV. In combination studies evaluating the in vitro antiviral activity of efavirenz and emtricitabine together, efavirenz and tenofovir together, and emtricitabine and tenofovir together, additive to synergistic antiviral effects were observed. Resistance Resistance to efavirenz can be selected in vitro and resulted in single or multiple amino acid substitutions in HIV-1 RT, including L100I, V108I, V179D, and Y181C. K103N was the most frequently observed RT substitution in viral isolates from patients who experienced rebound in viral load during clinical studies of efavirenz. Substitutions at RT positions 98, 100, 101, 108, 138, 188, 190 or 225 were also observed, but at lower frequencies, and often only in combination with K103N. Cross-resistance profiles for efavirenz, nevirapine and delavirdine in vitro demonstrated that the K103N substitution confers loss of susceptibility to all three NNRTIs. The potential for cross-resistance between efavirenz and NRTIs is low because of the different binding sites on the target and mechanism of action. The potential for cross-resistance between efavirenz and PIs is low because of the different enzyme targets involved. Resistance to emtricitabine or tenofovir has been seen in vitro and in some HIV-1 infected patients due to the development of an M184V or M184I substitution in RT with emtricitabine or a K65R substitution in RT with tenofovir. Emtricitabine-resistant viruses with the M184V/I mutation were cross-resistant to lamivudine, but retained sensitivity to didanosine, stavudine, tenofovir and zidovudine. The K65R mutation can also be selected by abacavir or didanosine and results in reduced susceptibility to these agents plus lamivudine, emtricitabine and tenofovir. Tenofovir disoproxil should be avoided in patients with HIV-1 harbouring the K65R mutation. Both the K65R and M184V/I mutation remain fully susceptible to efavirenz. In addition, a K70E substitution in HIV-1 RT has been selected by tenofovir and results in low-level reduced susceptibility to abacavir, emtricitabine, lamivudine and tenofovir. Patients with HIV-1 expressing three or more thymidine analogue associated mutations (TAMs) that included either an M41L or an L210W substitution in RT showed reduced susceptibility to tenofovir disoproxil. In vivo resistance (antiretroviral-naïve patients): In a 144-week open-label randomised clinical study (GS-01-934) in antiretroviral-naïve patients, where efavirenz, emtricitabine and tenofovir disoproxil were used as individual formulations (or as efavirenz and the fixed combination of emtricitabine and tenofovir disoproxil (Truvada) from week 96 to 144), genotyping was performed on plasma HIV-1 isolates from all patients with confirmed HIV RNA > 400 copies/ml at week 144 or early study drug discontinuation (see section on Clinical experience). As of week 144: • The M184V/I mutation developed in 2/19 (10.5%) isolates analysed from patients in the efavirenz + emtricitabine + tenofovir disoproxil group and in 10/29 (34.5%) isolates analysed from the efavirenz + lamivudine/zidovudine group (p-value < 0.05, Fisher’s Exact test comparing the emtricitabine + tenofovir disoproxil group to the lamivudine/zidovudine group among all subjects). • No virus analysed contained the K65R or K70E mutation. • Genotypic resistance to efavirenz, predominantly the K103N mutation, developed in virus from 13/19 (68%) patients in the efavirenz + emtricitabine + tenofovir disoproxil group and in virus from 21/29 (72%) patients in the efavirenz + lamivudine/zidovudine group. A summary of resistance mutation development is shown in Table 3. Table 3: Development of resistance in study GS-01-934 through week 144 Efavirenz+ Efavirenz+lamivudine/zid emtricitabine+ ovudine tenofovir disoproxil (N=243) (N=244) Resistance analysis by week 144 19 31 On-therapy genotypes 19 (100%) 29 (100%) Efavirenz resistance1 13 (68%) 21 (72%) K103N 8 (42%) 18* (62%) K101E 3 (16%) 3 (10%) G190A/S 2 (10.5%) 4 (14%) Y188C/H 1 (5%) 2 (7%) V108I 1 (5%) 1 (3%) P225H 0 2 (7%) M184V/I 2 (10.5%) 10* (34.5%) K65R 0 0 K70E 0 0 TAMs2 0 2 (7%) * p-value < 0.05, Fisher’s Exact test comparing efavirenz + emtricitabine + tenofovir disoproxil group to efavirenz + lamivudine/zidovudine group among all patients. 1 Other efavirenz resistance mutations included A98G (n=1), K103E (n=1), V179D (n=1), and M230L (n=1). 2 Thymidine analogue associated mutations included D67N (n=1) and K70R (n=1). In the open-label extended phase of study GS-01-934, where patients received Atripla on an empty stomach, 3 additional cases of resistance were seen. All 3 subjects had received a fixed dose combination of lamivudine and zidovudine (Combivir) and efavirenz for 144 weeks and then switched to Atripla. Two subjects with confirmed virologic rebound developed NNRTI resistance-associated substitutions to efavirenz including K103N, V106V/I/M and Y188Y/C reverse transcriptase substitutions at week 240 (96 weeks on Atripla) and week 204 (60 weeks on Atripla). A third subject had pre-existing NNRTI resistance-associated substitutions to efavirenz and the M184V reverse transcriptase resistance-associated substitution to emtricitabine at entry into the Atripla extension phase and experienced a suboptimal virologic response, and developed K65K/R, S68N and K70K/E NRTI resistance-associated substitutions at week 180 (36 weeks on Atripla). Please refer to the Summary of Product Characteristics for the individual components for additional information regarding in vivo resistance with these medicinal products. Clinical efficacy and safety In a 144-week open-label randomised clinical study (GS-01-934) antiretroviral treatment-naïve HIV-1 infected patients received either a once-daily regimen of efavirenz, emtricitabine and tenofovir disoproxil or a fixed combination of lamivudine and zidovudine (Combivir) administered twice daily and efavirenz once daily (please refer to the Summary of Product Characteristics for Truvada). Patients who completed 144 weeks of treatment with either treatment arm in study GS-01-934 were given the option to continue in an open-label extended phase of the study with Atripla on an empty stomach. Data are available from 286 patients who switched to Atripla: 160 had previously received efavirenz, emtricitabine and tenofovir disoproxil, and 126 had previously received Combivir and efavirenz. High rates of virologic suppression were maintained by subjects from both initial treatment groups who then received Atripla in the open-label extended phase of the study. After 96 weeks of Atripla treatment, HIV-1 RNA plasma concentrations remained < 50 copies/ml in 82% of patients and < 400 copies/ml in 85% of patients (intention to treat analysis (ITT), missing=failure). Study AI266073 was a 48-week open-label randomised clinical study in HIV infected patients comparing the efficacy of Atripla to antiretroviral therapy consisting of at least two nucleoside or nucleotide reverse transcriptase inhibitors (NRTIs) with a protease inhibitor or non-nucleoside reverse transcriptase inhibitor; however not a regimen containing all Atripla components (efavirenz, emtricitabine and tenofovir disoproxil). Atripla was administered on an empty stomach (see section 4.2). Patients had never experienced virological failure on a previous antiretroviral therapy, had no known HIV-1 mutations that confer resistance to any of the three components within Atripla, and had been virologically suppressed for at least three months at baseline. Patients either changed to Atripla (N=203) or continued on their original antiretroviral treatment regimen (N=97). Forty-eight week data showed that high levels of virologic suppression, comparable to the original treatment regimen, were maintained in patients who were randomised to change to Atripla (see Table 4). Table 4: 48-week efficacy data from study AI266073 in which Atripla was administered to virologically suppressed patients on combination antiretroviral therapy Treatment group Endpoint Atripla (N=203) Stayed on original Difference between Atripla and n/N (%) treatment regimen original treatment regimen (N=97) (95%CI) n/N (%) patients with HIV-1 RNA < 50 copies/ml PVR (KM) 94.5% 85.5% 8.9% (-7.7% to 25.6%) M=Excluded 179/181 (98.9%) 85/87 (97.7%) 1.2% (-2.3% to 6.7%) M=Failure 179/203 (88.2%) 85/97 (87.6%) 0.5% (-7.0% to 9.3%) Modified LOCF 190/203 (93.6%) 94/97 (96.9%) -3.3 (-8.3% to 2.7%) patients with HIV-1 RNA < 200 copies/ml PVR (KM) 98.4% 98.9% -0.5% (-3.2% to 2.2%) M=Excluded 181/181 (100%) 87/87 (100%) 0% (-2.4% to 4.2%) M=Failure 181/203 (89.2%) 87/97 (89.7%) -0.5% (-7.6% to 7.9%) PVR (KM): Pure virologic response assessed using the Kaplan Meier (KM) method M: Missing Modified LOCF: Post-hoc analysis where patients who failed virologically or discontinued for adverse events were treated as failures; for other drop-outs, the LOCF (last observation carried forward) method was applied When the two strata were analysed separately, response rates in the stratum with prior PI-treatment were numerically lower for patients switched to Atripla [92.4% versus 94.0% for the PVR (sensitivity analysis) for Atripla and SBR patients respectively; a difference (95%CI) of -1.6% (-10.0%, 6.7%). In the prior-NNRTI stratum, response rates were 98.9% vs 97.4% for Atripla and SBR patients respectively; a difference (95%CI) of 1.4% (-4.0%, 6.9%)]. A similar trend was observed in a sub-group analysis of treatment-experienced patients with baseline HIV-1 RNA < 75 copies/ml from a retrospective cohort study (data collected over 20 months, see Table 5). Table 5: Maintenance of pure virologic response (Kaplan Meier % (Standard Error) [95%CI]) at week 48 for treatment-experienced patients with baseline HIV-1 RNA < 75 copies/ml who had therapy switched to Atripla according to the type of prior antiretroviral regimen (Kaiser Permanente patient database) Prior Atripla components Prior NNRTI-based regimen Prior PI-based regimen (N=299) (N=104) (N=34) 98.9% (0.6%) 98.0% (1.4%) 93.4% (4.5%) [96.8%, 99.7%] [92.3%, 99.5%] [76.2%, 98.3%] No data are currently available from clinical studies with Atripla in treatment-naïve patients or in heavily pretreated patients. There is no clinical experience with Atripla in patients who are experiencing virological failure in a first-line antiretroviral treatment regimen or in combination with other antiretroviral agents. Patients coinfected with HIV and HBV Limited clinical experience in patients co-infected with HIV and HBV suggests that treatment with emtricitabine or tenofovir disoproxil in antiretroviral combination therapy to control HIV infection also results in a reduction in HBV DNA (3 log10 reduction or 4 to 5 log10 reduction, respectively) (see section 4.4).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The separate pharmaceutical forms of efavirenz, emtricitabine and tenofovir disoproxil were used to determine the pharmacokinetics of efavirenz, emtricitabine and tenofovir disoproxil, administered separately in HIV infected patients. The bioequivalence of one Atripla film-coated tablet with one efavirenz 600 mg film-coated tablet plus one emtricitabine 200 mg hard capsule plus one tenofovir disoproxil 245 mg film-coated tablet (equivalent to 300 mg tenofovir disoproxil fumarate) administered together, was established following single dose administration to fasting healthy subjects in study GS-US-177-0105 (see Table 6). Table 6: Summary of pharmacokinetic data from study GS-US-177-0105 Efavirenz Emtricitabine Tenofovir disoproxil (n=45) (n=45) (n=45) GMR (%) GMR (%) GMR (%) Parameters Test Reference (90%CI) Test Reference (90%CI) Test Reference (90%CI) 98.79 88.84 91.46 2,264.3 2,308.6 2,130.6 2,384.4 325.1 352.9 Cmax (ng/ml) (92.28, (84.02, (84.64, (26.8) (30.3) (25.3) (20.4) (34.2) (29.6) 105.76) 93.94) 98.83) 95.84 97.98 99.29 AUC0-last 125,623.6 132,795.7 10,682.6 10,874.4 1,948.8 1,969.0 (90.73, (94.90, (91.02, (ng∙h/ml) (25.7) (27.0) (18.1) (14.9) (32.9) (32.8) 101.23) 101.16) 108.32) 95.87 97.96 100.45 AUCinf 146,074.9 155,518.6 10,854.9 11,054.3 2,314.0 2,319.4 (89.63, (94.86, (93.22, (ng∙h/ml) (33.1) (34.6) (17.9) (14.9) (29.2) (30.3) 102.55) 101.16) 108.23) T1/2 180.6 182.5 14.5 14.6 18.9 17.8 (h) (45.3) (38.3) (53.8) (47.8) (20.8) (22.6) Test: single fixed-dose combination tablet taken under fasted conditions. Reference: single dose of a 600 mg efavirenz tablet, 200 mg emtricitabine capsule and 300 mg tenofovir disoproxil tablet taken under fasted conditions. Values for Test and Reference are mean (% coefficient of variation). GMR=geometric least-squares mean ratio, CI=confidence interval Absorption In HIV infected patients, peak efavirenz plasma concentrations were attained by 5 hours and steady-state concentrations reached in 6 to 7 days. In 35 patients receiving efavirenz 600 mg once daily, steady-state peak concentration (Cmax) was 12.9 ± 3.7 µM (29%) [mean ± standard deviation (S.D.) (coefficient of variation (%CV))], steady-state Cmin was 5.6 ± 3.2 µM (57%), and AUC was 184 ± 73 µM•h (40%). Emtricitabine is rapidly absorbed with peak plasma concentrations occurring at 1 to 2 hours post-dose. Following multiple dose oral administration of emtricitabine to 20 HIV infected patients, steady-state Cmax was 1.8 ± 0.7 µg/ml (mean ± S.D.) (39%CV), steady-state Cmin was 0.09 ± 0.07 µg/ml (80%) and the AUC was 10.0 ± 3.1 µg•h/ml (31%) over a 24 hour dosing interval. Following oral administration of a single 300 mg dose of tenofovir disoproxil to HIV-1 infected patients in the fasted state, maximum tenofovir concentrations were achieved within one hour and the Cmax and AUC (mean ± S.D.) (%CV) values were 296 ± 90 ng/ml (30%) and 2,287 ± 685 ng•h/ml (30%), respectively. The oral bioavailability of tenofovir from tenofovir disoproxil in fasted patients was approximately 25%. Effect of food Atripla has not been evaluated in the presence of food. Administration of efavirenz capsules with a high fat meal increased the mean AUC and Cmax of efavirenz by 28% and 79%, respectively, compared to administration in a fasted state. Compared to fasted administration, dosing of tenofovir disoproxil and emtricitabine in combination with either a high fat meal or a light meal increased the mean AUC of tenofovir by 43.6% and 40.5%, and Cmax by 16% and 13.5%, respectively without affecting emtricitabine exposures. Atripla is recommended for administration on an empty stomach since food may increase efavirenz exposure and may lead to an increase in the frequency of adverse reactions (see sections 4.4 and 4.8). It is anticipated that tenofovir exposure (AUC) will be approximately 30% lower following administration of Atripla on an empty stomach as compared to the individual component tenofovir disoproxil when taken with food (see section 5.1). Distribution Efavirenz is highly bound (> 99%) to human plasma proteins, predominantly albumin. In vitro binding of emtricitabine to human plasma proteins is < 4% and independent of concentrations over the range of 0.02 to 200 µg/ml. Following intravenous administration the volume of distribution of emtricitabine was approximately 1.4 l/kg. After oral administration, emtricitabine is widely distributed throughout the body. The mean plasma to blood concentration ratio was approximately 1.0 and the mean semen to plasma concentration ratio was approximately 4.0. In vitro binding of tenofovir to human plasma or serum protein is < 0.7% and 7.2%, respectively over the tenofovir concentration range 0.01 to 25 µg/ml. Following intravenous administration the volume of distribution of tenofovir was approximately 800 ml/kg. After oral administration, tenofovir is widely distributed throughout the body. Biotransformation Studies in humans and in vitro studies using human liver microsomes have demonstrated that efavirenz is principally metabolised by the CYP system to hydroxylated metabolites with subsequent glucuronidation of these hydroxylated metabolites. These metabolites are essentially inactive against HIV-1. The in vitro studies suggest that CYP3A4 and CYP2B6 are the major isozymes responsible for efavirenz metabolism and that it inhibits CYP isozymes 2C9, 2C19, and 3A4. In in vitro studies efavirenz did not inhibit CYP2E1 and inhibited CYP2D6 and CYP1A2 only at concentrations well above those achieved clinically. Efavirenz plasma exposure may be increased in patients with homozygous G516T genetic variant of the CYP2B6 isozyme. The clinical implications of such an association are unknown; however, the potential for an increased frequency and severity of efavirenz-associated adverse events cannot be excluded. Efavirenz has been shown to induce CYP3A4 and CYP2B6, resulting in the induction of its own metabolism, which may be clinically relevant in some patients. In uninfected volunteers, multiple doses of 200 to 400 mg per day for 10 days resulted in a lower than predicted extent of accumulation (22 to 42% lower) and a shorter terminal half-life of 40 to 55 hours (single dose half-life 52 to 76 hours). Efavirenz has also been shown to induce UGT1A1. Exposures of raltegravir (a UGT1A1 substrate) are reduced in the presence of efavirenz (see section 4.5, Table 1). Although in vitro data suggest that efavirenz inhibits CYP2C9 and CYP2C19, there have been contradictory reports of both increased and decreased exposures to substrates of these enzymes when co-administered with efavirenz in vivo. The net effect of co-administration is not clear. There is limited metabolism of emtricitabine. The biotransformation of emtricitabine includes oxidation of the thiol moiety to form the 3'-sulphoxide diastereomers (approximately 9% of dose) and conjugation with glucuronic acid to form 2'-O-glucuronide (approximately 4% of dose). In vitro studies have determined that neither tenofovir disoproxil nor tenofovir are substrates for the CYP enzymes. Neither emtricitabine nor tenofovir inhibited in vitro drug metabolism mediated by any of the major human CYP isoforms involved in drug biotransformation. Also, emtricitabine did not inhibit uridine 5'-diphosphoglucuronyl transferase, the enzyme responsible for glucuronidation. Elimination Efavirenz has a relatively long terminal half-life of at least 52 hours after single doses (see also data from bioequivalence study described above) and 40 to 55 hours after multiple doses. Approximately 14 to 34% of a radiolabelled dose of efavirenz was recovered in the urine and less than 1% of the dose was excreted in urine as unchanged efavirenz. Following oral administration, the elimination half-life of emtricitabine is approximately 10 hours. Emtricitabine is primarily excreted by the kidneys with complete recovery of the dose achieved in urine (approximately 86%) and faeces (approximately 14%). Thirteen percent of the emtricitabine dose was recovered in urine as three metabolites. The systemic clearance of emtricitabine averaged 307 ml/min. Following oral administration, the elimination half-life of tenofovir is approximately 12 to 18 hours. Tenofovir is primarily excreted by the kidneys by both filtration and an active tubular transport system with approximately 70 to 80% of the dose excreted unchanged in urine following intravenous administration. The apparent clearance of tenofovir averaged approximately 307 ml/min. Renal clearance has been estimated to be approximately 210 ml/min, which is in excess of the glomerular filtration rate. This indicates that active tubular secretion is an important part of the elimination of tenofovir. Pharmacokinetics in special populations Age Pharmacokinetic studies have not been performed with efavirenz, emtricitabine or tenofovir in elderly patients (over 65 years of age). Gender The pharmacokinetics of emtricitabine and tenofovir are similar in male and female patients. Limited data suggest that females may have higher exposure to efavirenz but they do not appear to be less tolerant of efavirenz. Ethnicity Limited data suggest that Asian and Pacific Island patients may have higher exposure to efavirenz but they do not appear to be less tolerant of efavirenz. Renal impairment The pharmacokinetics of efavirenz, emtricitabine and tenofovir disoproxil after co-administration of the separate pharmaceutical forms or as Atripla have not been studied in HIV infected patients with renal impairment. Pharmacokinetic parameters were determined following administration of single doses of the individual preparations of emtricitabine 200 mg or tenofovir disoproxil 245 mg to non-HIV infected patients with varying degrees of renal impairment. The degree of renal impairment was defined according to baseline creatinine clearance (normal renal function when creatinine clearance > 80 ml/min; mild impairment with creatinine clearance=50 to 79 ml/min; moderate impairment with creatinine clearance=30 to 49 ml/min and severe impairment with creatinine clearance=10 to 29 ml/min). The mean (%CV) emtricitabine exposure increased from 12 µg•h/ml (25%) in subjects with normal renal function to 20 µg•h/ml (6%), 25 µg•h/ml (23%) and 34 µg•h/ml (6%) in patients with mild, moderate and severe renal impairment, respectively. The mean (%CV) tenofovir exposure increased from 2,185 ng•h/ml (12%) in patients with normal renal function, to 3,064 ng•h/ml (30%), 6,009 ng•h/ml (42%) and 15,985 ng•h/ml (45%) in patients with mild, moderate and severe renal impairment, respectively. In patients with end-stage renal disease (ESRD) requiring haemodialysis, between dialysis drug exposures substantially increased over 72 hours to 53 µg•h/ml (19%) of emtricitabine, and over 48 hours to 42,857 ng•h/ml (29%) of tenofovir. The pharmacokinetics of efavirenz have not been studied in patients with renal impairment. However, less than 1% of an efavirenz dose is excreted unchanged in the urine, so the impact of renal impairment on exposure to efavirenz is likely to be minimal. Atripla is not recommended for patients with moderate or severe renal impairment (creatinine clearance < 50 ml/min). Patients with moderate or severe renal impairment require dose interval adjustment of emtricitabine and tenofovir disoproxil that cannot be achieved with the combination tablet (see sections 4.2 and 4.4). Hepatic impairment The pharmacokinetics of Atripla have not been studied in HIV infected patients with hepatic impairment. Atripla should be administered with caution to patients with mild hepatic impairment (see sections 4.3 and 4.4). Atripla must not be used in patients with severe hepatic impairment (see section 4.3) and is not recommended for patients with moderate hepatic impairment. In a single-dose study of efavirenz, half-life was doubled in the single patient with severe hepatic impairment (Child-Pugh-Turcotte Class C), indicating a potential for a much greater degree of accumulation. A multiple-dose study of efavirenz showed no significant effect on efavirenz pharmacokinetics in patients with mild hepatic impairment (Child-Pugh-Turcotte Class A) compared with controls. There were insufficient data to determine whether moderate or severe hepatic impairment (Child-Pugh-Turcotte Class B or C) affects efavirenz pharmacokinetics. The pharmacokinetics of emtricitabine have not been studied in non-HBV infected patients with varying degrees of hepatic insufficiency. In general, emtricitabine pharmacokinetics in HBV infected patients were similar to those in healthy subjects and in HIV infected patients. A single 245 mg dose of tenofovir disoproxil was administered to non-HIV infected patients with varying degrees of hepatic impairment defined according to CPT classification. Tenofovir pharmacokinetics were not substantially altered in subjects with hepatic impairment suggesting that no dose adjustment of tenofovir disoproxil is required in these subjects.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול בנשאי HIVב. מתן התרופה ייעשה לפי מרשם של מנהל מרפאה לטיפול באיידס, במוסד רפואי שהמנהל הכיר בו כמרכז AIDS.ג. משטר הטיפול בתרופה יהיה כפוף להנחיות המנהל, כפי שיעודכנו מזמן לזמן על פי המידע העדכני בתחום הטיפול במחלה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| . התרופה האמורה תינתן לטיפול בנשאי HIV | 10/01/2012 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
10/01/2012
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
