Quest for the right Drug
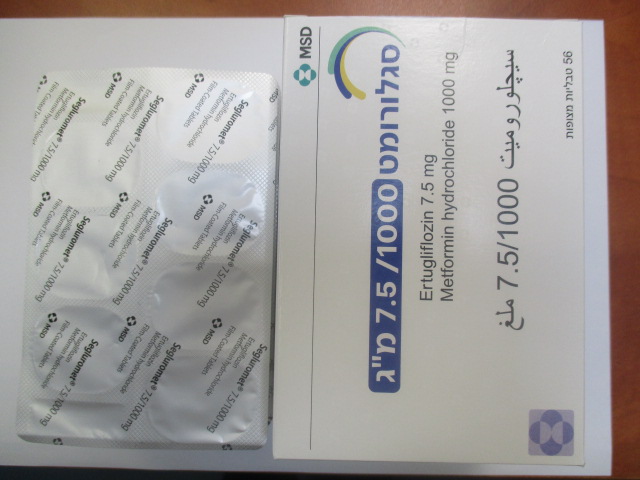
סגלורומט 7.5/1000 מ"ג SEGLUROMET 7.5/1000 MG (ERTUGLIFLOZIN (L-PGA), METFORMIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs used in diabetes, combinations of oral blood glucose lowering drugs, ATC code: A10BD23. Mechanism of action Segluromet combines two antihyperglycaemic agents with complementary mechanisms of action to improve glycaemic control in patients with type 2 diabetes: ertugliflozin, a SGLT2 inhibitor, and metformin hydrochloride, a member of the biguanide class. Ertugliflozin SGLT2 is the predominant transporter responsible for reabsorption of glucose from the glomerular filtrate back into the circulation. Ertugliflozin is a potent, selective, and reversible inhibitor of SGLT2. By inhibiting SGLT2, ertugliflozin reduces renal reabsorption of filtered glucose and lowers the renal threshold for glucose, and thereby increases urinary glucose excretion. Metformin Metformin is an antihyperglycaemic agent which improves glucose tolerance in patients with type 2 diabetes, lowering both basal and post-prandial plasma glucose. Its pharmacologic mechanisms of action are different from other classes of oral antihyperglycaemic agents. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilisation. Unlike sulphonylureas, metformin does not produce hypoglycaemia in either patients with type 2 diabetes or normal subjects, except in special circumstances (see section 4.5), and does not cause hyperinsulinaemia. With metformin therapy, insulin secretion remains unchanged while fasting insulin levels and day-long plasma insulin response may actually decrease. Pharmacodynamic effects Ertugliflozin Urinary glucose excretion and urinary volume Dose-dependent increases in the amount of glucose excreted in urine were observed in healthy subjects and in patients with type 2 diabetes mellitus following single- and multiple-dose administration of ertugliflozin. Dose-response modelling indicates that ertugliflozin 5 mg and 15 mg result in near maximal urinary glucose excretion (UGE) in patients with type 2 diabetes mellitus, providing 87% and 96% of maximal inhibition, respectively. Clinical efficacy and safety Ertugliflozin in combination with metformin The efficacy and safety of ertugliflozin in combination with metformin have been studied in 4 multi-centre, randomised, double-blind, placebo- and active comparator-controlled, Phase 3 clinical studies involving 3,643 patients with type 2 diabetes. Across the four studies, the racial distribution ranged from 66.2% to 80.3% White, 10.6% to 20.3% Asian, 1.9% to 10.3% Black, and 4.5% to 7.4% other. Hispanic or Latino patients comprised 15.6% to 34.5% of the population. The mean age of the patients across these four studies ranged from 55.1 to 59.1 years (range 21 years to 86 years); 15.6% to 29.9% of patients were ≥65 years of age and 0.6% to 3.8% were ≥75 years of age. Ertugliflozin as add-on combination therapy with metformin A total of 621 patients with type 2 diabetes inadequately controlled on metformin monotherapy (≥ 1,500 mg/day) participated in a randomised, double-blind, multi-centre, 26-week, placebo- controlled study to evaluate the efficacy and safety of ertugliflozin in combination with metformin. Patients were randomised to ertugliflozin 5 mg, ertugliflozin 15 mg, or placebo administered once daily in addition to continuation of background metformin therapy (see Table 2). Table 2: Results at Week 26 from a placebo-controlled study for ertugliflozin used in combination with metformin* Ertugliflozin 5 mg Ertugliflozin 15 mg Placebo HbA1c (%) N = 207 N = 205 N = 209 Baseline (mean) 8.1 8.1 8.2 Change from baseline (LS mean†) -0.7 -0.9 -0.0 Difference from placebo (LS mean†, 95% CI) -0.7‡ (-0.9, -0.5) -0.9‡ (-1.1, -0.7) Patients [N (%)] with HbA1c < 7% 73 (35.3)§ 82 (40.0)§ 33 (15.8) Body Weight (kg) N = 207 N = 205 N = 209 Baseline (mean) 84.9 85.3 84.5 Change from baseline (LS mean†) -3.0 -2.9 -1.3 Difference from placebo (LS mean†, 95% CI) -1.7‡ (-2.2, -1.1) -1.6‡ (-2.2, -1.0) * N includes all randomised, treated patients who had at least one measurement of the outcome variable. † Least squares means adjusted for time, prior antihyperglycaemic medication, baseline eGFR, menopausal status randomisation stratum and the interaction of time by treatment. ‡ p≤ 0.001 compared to placebo. § p< 0.001 compared to placebo (based on adjusted odds ratio comparisons from a logistic regression model using multiple imputation for missing data values). Factorial study with ertugliflozin and sitagliptin as add-on combination therapy with metformin A total of 1,233 patients with type 2 diabetes participated in a randomised, double-blind, multi-centre, 26-week, active-controlled study to evaluate the efficacy and safety of ertugliflozin 5 mg or 15 mg in combination with sitagliptin 100 mg compared to the individual components. Patients with type 2 diabetes inadequately controlled on metformin monotherapy (≥ 1,500 mg/day) were randomised to one of five active-treatment arms: ertugliflozin 5 mg or 15 mg, sitagliptin 100 mg, or sitagliptin 100 mg in combination with 5 mg or 15 mg ertugliflozin administered once daily in addition to continuation of background metformin therapy (see Table 3). Table 3: Results at Week 26 from a factorial study with ertugliflozin and sitagliptin as add-on combination therapy with metformin compared to individual components alone* Ertugliflozin Ertugliflozin Sitagliptin Ertugliflozin 5 mg + Ertugliflozin 15 mg 5 mg 15 mg 100 mg Sitagliptin 100 mg + Sitagliptin 100 mg HbA1c (%) N = 250 N = 248 N = 247 N = 243 N = 244 Baseline (mean) 8.6 8.6 8.5 8.6 8.6 Change from baseline (LS mean†) -1.0 -1.1 -1.1 -1.5 -1.5 Difference from Sitagliptin -0.4‡ (-0.6, -0.3) -0.5‡ (-0.6, -0.3) Ertugliflozin 5 mg -0.5‡ (-0.6, -0.3) Ertugliflozin 15 mg -0.4‡ (-0.6, -0.3) (LS mean†, 95% CI) Patients [N (%)] with HbA1c < 7% 66 (26.4) 79 (31.9) 81 (32.8) 127 (52.3)§ 120 (49.2)§ Body Weight (kg) N = 250 N = 248 N = 247 N = 243 N = 244 Baseline (mean) 88.6 88.0 89.8 89.5 87.5 Change from baseline (LS mean†) -2.7 -3.7 -0.7 -2.5 -2.9 Difference from Sitagliptin -1.8‡ (-2.5, -1.2) -2.3‡ (-2.9, -1.6) (LS mean , 95% CI) † * N includes all randomised, treated patients who had at least one measurement of the outcome variable. † Least squares means adjusted for time, baseline eGFR and the interaction of time by treatment. ‡ p< 0.001 compared to control group. § p< 0.001 compared to corresponding dose of ertugliflozin or sitagliptin (based on adjusted odds ratio comparisons from a logistic regression model using multiple imputation for missing data values). Ertugliflozin as add-on combination therapy with metformin and sitagliptin A total of 463 patients with type 2 diabetes inadequately controlled on metformin (≥ 1,500 mg/day) and sitagliptin 100 mg once daily participated in a randomised, double-blind, multi-centre, 26-week, placebo-controlled study to evaluate the efficacy and safety of ertugliflozin. Patients were randomised to ertugliflozin 5 mg, ertugliflozin 15 mg, or placebo administered once daily in addition to continuation of background metformin and sitagliptin therapy (see Table 4). Table 4: Results at Week 26 from an add-on study of ertugliflozin in combination with metformin and sitagliptin* Ertugliflozin 5 mg Ertugliflozin 15 mg Placebo HbA1c (%) N = 156 N = 153 N = 153 Baseline (mean) 8.1 8.0 8.0 Change from baseline (LS mean†) -0.8 -0.9 -0.1 Difference from placebo (LS mean†, 95% CI) -0.7‡ (-0.9, -0.5) -0.8‡ (-0.9, -0.6) Patients [N (%)] with HbA1c < 7% 50 (32.1) § 61 (39.9) § 26 (17.0) Body Weight (kg) N = 156 N = 153 N = 153 Baseline (mean) 87.6 86.6 86.5 Change from baseline (LS mean†) -3.3 -3.0 -1.3 Difference from placebo (LS mean†, 95% CI) -2.0‡ (-2.6, -1.4) -1.7‡ (-2.3, -1.1) * N includes all randomised, treated patients who had at least one measurement of the outcome variable. † Least squares means adjusted for time, prior antihyperglycaemic medication, baseline eGFR and the interaction of time by treatment. ‡ p≤ 0.001 compared to placebo. § p< 0.001 compared to placebo (based on adjusted odds ratio comparisons from a logistic regression model using multiple imputation for missing data values). Active-controlled study of ertugliflozin versus glimepiride as add-on combination therapy with metformin A total of 1,326 patients with type 2 diabetes inadequately controlled on metformin monotherapy participated in a randomised, double-blind, multi-centre, 52-week, active comparator-controlled study to evaluate the efficacy and safety of ertugliflozin in combination with metformin. These patients, who were receiving metformin monotherapy (≥ 1,500 mg/day), were randomised to ertugliflozin 5 mg, ertugliflozin 15 mg, or glimepiride administered once daily in addition to continuation of background metformin therapy. Glimepiride was initiated at 1 mg/day and titrated up to a maximum dose of 6 or 8 mg/day (depending on maximum approved dose in each country) or a maximum tolerated dose or down-titrated to avoid or manage hypoglycaemia. The mean daily dose of glimepiride was 3.0 mg (see Table 5). Table 5: Results at Week 52 from an active-controlled study comparing ertugliflozin to glimepiride as add-on therapy in patients inadequately controlled on metformin* Ertugliflozin 5 mg Ertugliflozin 15 mg Glimepiride HbA1c (%) N = 448 N = 440 N = 437 Baseline (mean) 7.8 7.8 7.8 Change from baseline (LS mean†) -0.6 -0.6 -0.7 Difference from glimepiride (LS mean†, 95% CI) 0.2 (0.1, 0.3) 0.1‡ (-0.0, 0.2) Patients [N (%)] with HbA1c < 7% 154 (34.4) 167 (38.0) 190 (43.5) Body Weight (kg) N = 448 N = 440 N = 437 Baseline (mean) 87.9 85.6 86.8 Change from baseline (LS mean†) -3.0 -3.4 0.9 Difference from glimepiride (LS mean†, 95% CI) -3.9 (-4.4, -3.4) -4.3§ (-4.8, -3.8) * N includes all randomised, treated patients who had at least one measurement of the outcome variable. † Least squares means adjusted for time, prior antihyperglycaemic medication, baseline eGFR and the interaction of time by treatment. ‡ Non-inferiority is declared when the upper bound of the two-sided 95% confidence interval (CI) for the mean difference is less than 0.3%. § p< 0.001 compared to glimepiride. Ertugliflozin as add-on combination therapy with insulin (with or without metformin) In an 18-week randomised, double-blind, multi-centre, placebo-controlled, glycaemic sub-study of VERTIS CV, a total of 1,065 patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease with inadequate glycaemic control (HbA1c between 7% and 10.5%) with background therapy of insulin ≥20 units/day (59% patients were also on metformin ≥1,500 mg/day) were randomised to ertugliflozin 5 mg, ertugliflozin 15 mg or placebo once daily (see Table 6). Table 6: Results at Week 18 from an add-on study of ertugliflozin in combination with insulin (with or without metformin) in patients with type 2 diabetes mellitus* Ertugliflozin 5 mg Ertugliflozin 15 mg Placebo HbA1c (%) N = 348 N = 370 N = 347 Baseline (mean) 8.4 8.4 8.4 Change from baseline (LS mean†) -0.8 -0.8 -0.2 Difference from placebo (LS mean†, 95% CI) -0.6‡ (-0.7, -0.4) -0.6‡ (-0.8, -0.5) § § Patients [N (%)] with HbA1c <7% 72 (20.7) 78 (21.1) 37 (10.7) Body Weight (kg) N = 348 N = 370 N = 347 Baseline (mean) 93.8 92.1 93.3 Change from baseline (LS mean†) -1.9 -2.1 -0.2 Difference from placebo (LS mean†, 95% CI) -1.6‡ (-2.1, -1.1) -1.9‡ (-2.4, -1.4) * N includes all randomised, treated patients who had at least one measurement of the outcome variable. † Least squares means adjusted for time, insulin stratum, baseline eGFR, and the interaction of time by treatment. ‡ p< 0.001 compared to placebo. § p< 0.001 compared to placebo (based on adjusted odds ratio comparisons from a logistic regression model using multiple imputation for missing data values). Ertugliflozin as add-on combination therapy with metformin and sulphonylurea In an 18-week randomised, double-blind, multi-centre, placebo-controlled, glycaemic sub-study of VERTIS CV, a total of 330 patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease with inadequate glycaemic control (HbA1c between 7% and 10.5%) with background therapy of metformin ≥1,500 mg/day and a sulphonylurea were randomised to ertugliflozin 5 mg, ertugliflozin 15 mg or placebo once daily (see Table 7). Table 7: Results at Week 18 from an add-on study of ertugliflozin in combination with metformin and a sulphonylurea in patients with type 2 diabetes mellitus* Ertugliflozin 5 mg Ertugliflozin 15 mg Placebo HbA1c (%) N = 100 N = 113 N = 117 Baseline (mean) 8.4 8.3 8.3 Change from baseline (LS mean†) -0.9 -1.0 -0.2 Difference from placebo (LS mean†, 95% CI) -0.7‡ (-0.9, -0.4) -0.8‡ (-1.0, -0.5) § § Patients [N (%)] with HbA1c <7% 37 (37.0) 37 (32.7) 15 (12.8) Body Weight (kg) N = 100 N = 113 N = 117 Baseline (mean) 92.1 92.9 90.5 Change from baseline (LS mean†) -2.0 -2.4 -0.5 Difference from placebo (LS mean†, 95% CI) -1.6‡ (-2.3, -0.8) -1.9‡(-2.6, -1.2) * N includes all randomised, treated patients who had at least one measurement of the outcome variable. † Least squares means adjusted for time, baseline eGFR, and the interaction of time by treatment. ‡ p< 0.001 compared to placebo. § p< 0.001 compared to placebo (based on adjusted odds ratio comparisons from a logistic regression model using multiple imputation for missing data values). Fasting plasma glucose In three placebo-controlled studies, ertugliflozin resulted in statistically significant reductions in FPG. For ertugliflozin 5 mg and 15 mg, respectively, the placebo-corrected reductions in FPG were 1.92 and 2.44 mmol/L as monotherapy, 1.48 and 2.12 mmol/L as add-on to metformin, and 1.40 and 1.74 mmol/L as add-on to metformin and sitagliptin. The combination of ertugliflozin and sitagliptin on a background of metformin resulted in significantly greater reductions in FPG compared to sitagliptin or ertugliflozin alone. The combination of ertugliflozin 5 or 15 mg and sitagliptin resulted in incremental FPG reductions of 0.46 and 0.65 mmol/L compared to the ertugliflozin alone or 1.02 and 1.28 mmol/L compared to sitagliptin alone, respectively. Efficacy in patients with baseline HbA1c ≥ 9% In the study of ertugliflozin in combination with metformin in patients with baseline HbA1c from 7.0-10.5%, the placebo-corrected reductions in HbA1c for the subgroup of patients in the study with baseline HbA1c ≥ 9% were 1.31% and 1.43% with ertugliflozin 5 mg and 15 mg, respectively. In the study of patients inadequately controlled on metformin with baseline HbA1c from 7.5-11.0%, among the subgroup of patients with a baseline HbA1c ≥ 10%, the combination of ertugliflozin 5 mg or 15 mg with sitagliptin resulted in reductions of HbA1c of 2.35% and 2.66%, respectively, compared to 2.10%, 1.30%, and 1.82% for ertugliflozin 5 mg, ertugliflozin 15 mg, and sitagliptin alone, respectively. Blood pressure As add-on to metformin, ertugliflozin 5 mg and 15 mg resulted in statistically significant placebo-corrected reductions in SBP of 3.7 mmHg and 4.5 mmHg, respectively. As add-on to metformin and sitagliptin, ertugliflozin 5 mg and 15 mg resulted in statistically significant placebo-corrected reductions in SBP of 2.9 mmHg and 3.9 mmHg, respectively. In a 52-week, active-controlled study versus glimepiride, reductions from baseline in SBP were 2.2 mmHg and 3.8 mmHg for ertugliflozin 5 mg and 15 mg, respectively, while subjects treated with glimepiride had an increase in SBP from baseline of 1.0 mmHg. Subgroup analysis In patients with type 2 diabetes treated with ertugliflozin in combination with metformin, clinically meaningful reductions in HbA1c were observed in subgroups defined by age, sex, race, ethnicity, geographic region, baseline BMI, baseline HbA1c, and duration of type 2 diabetes mellitus.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Segluromet Segluromet has been shown to be bioequivalent to coadministration of corresponding doses of ertugliflozin and metformin tablets. Ertugliflozin General introduction The pharmacokinetics of ertugliflozin are similar in healthy subjects and patients with type 2 diabetes. The steady state mean plasma AUC and Cmax were 398 ng∙hr/mL and 81 ng/mL, respectively, with 5 mg ertugliflozin once daily treatment, and 1,193 ng∙hr/mL and 268 ng/mL, respectively, with 15 mg ertugliflozin once daily treatment. Steady-state is reached after 4 to 6 days of once-daily dosing with ertugliflozin. Ertugliflozin does not exhibit time-dependent pharmacokinetics and accumulates in plasma up to 10-40% following multiple dosing. Absorption Following single-dose oral administration of 5 mg and 15 mg of ertugliflozin, peak plasma concentrations (median Tmax) of ertugliflozin occur at 1 hour post-dose under fasted conditions. Plasma Cmax and AUC of ertugliflozin increase in a dose-proportional manner following single doses from 0.5 mg to 300 mg and following multiple doses from 1 mg to 100 mg. The absolute oral bioavailability of ertugliflozin following administration of a 15-mg dose is approximately 100%. Administration of ertugliflozin with a high-fat and high-calorie meal decreases ertugliflozin Cmax by 29% and prolongs Tmax by 1 hour but does not alter AUC as compared with the fasted state. The observed effect of food on ertugliflozin pharmacokinetics is not considered clinically relevant, and ertugliflozin may be administered with or without food. In Phase 3 clinical trials, ertugliflozin was administered without regard to meals. The effects of a high-fat meal on the pharmacokinetics of ertugliflozin and metformin when administered as Segluromet tablets are comparable to those reported for the individual tablets. Food had no meaningful effect on AUCinf of ertugliflozin or metformin, but reduced mean ertugliflozin Cmax by approximately 41% and metformin Cmax by approximately 29% compared to the fasted condition. Ertugliflozin is a substrate of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP) transporters. Distribution The mean steady-state volume of distribution of ertugliflozin following an intravenous dose is 86 l. Plasma protein binding of ertugliflozin is 93.6% and is independent of ertugliflozin plasma concentrations. Plasma protein binding is not meaningfully altered in patients with renal or hepatic impairment. The blood-to-plasma concentration ratio of ertugliflozin is 0.66. Ertugliflozin is not a substrate of organic anion transporters (OAT1, OAT3), organic cation transporters (OCT1, OCT2), or organic anion transporting polypeptides (OATP1B1, OATP1B3) in vitro. Biotransformation Metabolism is the primary clearance mechanism for ertugliflozin. The major metabolic pathway for ertugliflozin is UGT1A9 and UGT2B7-mediated O-glucuronidation to two glucuronides that are pharmacologically inactive at clinically relevant concentrations. CYP-mediated (oxidative) metabolism of ertugliflozin is minimal (12%). Elimination The mean systemic plasma clearance following an intravenous 100 µg dose was 11 l/hr. The mean elimination half-life in type 2 diabetic patients with normal renal function was estimated to be 17 hours based on the population pharmacokinetic analysis. Following administration of an oral [14C]-ertugliflozin solution to healthy subjects, approximately 41% and 50% of the drug-related radioactivity was eliminated in faeces and urine, respectively. Only 1.5% of the administered dose was excreted as unchanged ertugliflozin in urine and 34% as unchanged ertugliflozin in faeces, which is likely due to biliary excretion of glucuronide metabolites and subsequent hydrolysis to parent. Special populations Renal impairment In a Phase 1 clinical pharmacology study in patients with type 2 diabetes and mild, moderate, or severe renal impairment (as determined by eGFR), following a single-dose administration of 15 mg ertugliflozin, the mean increases in AUC of ertugliflozin were ≤ 1.7-fold, compared to subjects with normal renal function. These increases in ertugliflozin AUC are not considered clinically relevant. There were no clinically meaningful differences in the ertugliflozin Cmax values among the different renal function groups. The 24-hour urinary glucose excretion declined with increasing severity of renal impairment (see section 4.4). The plasma protein binding of ertugliflozin was unaffected in patients with renal impairment. Hepatic impairment Moderate hepatic impairment (based on the Child-Pugh classification) did not result in an increase in exposure of ertugliflozin. The AUC of ertugliflozin decreased by approximately 13%, and Cmax decreased by approximately 21% compared to subjects with normal hepatic function. This decrease in ertugliflozin exposure is not considered clinically meaningful. There is no clinical experience in patients with Child-Pugh class C (severe) hepatic impairment. The plasma protein binding of ertugliflozin was unaffected in patients with moderate hepatic impairment. Paediatric population No studies with ertugliflozin have been performed in paediatric patients. Effects of age, body weight, gender and race Based on a population pharmacokinetic analysis, age, body weight, gender, and race do not have a clinically meaningful effect on the pharmacokinetics of ertugliflozin. Drug Interactions In vitro assessment of ertugliflozin In in vitro studies, ertugliflozin and ertugliflozin glucuronides did not inhibit or inactivate CYPs 1A2, 2C9, 2C19, 2C8, 2B6, 2D6, or 3A4, and did not induce CYPs 1A2, 2B6, or 3A4. Ertugliflozin and ertugliflozin glucuronides did not inhibit the activity of UGTs 1A6, 1A9 or 2B7 in vitro. Ertugliflozin was a weak inhibitor of UGTs 1A1 and 1A4 in vitro at higher concentrations that are not clinically relevant. Ertugliflozin glucuronides had no effect on these isoforms. Overall, ertugliflozin is unlikely to affect the pharmacokinetics of concurrently administered drugs eliminated by these enzymes. Ertugliflozin or ertugliflozin glucuronides do not meaningfully inhibit P-gp, OCT2, OAT1, or OAT3 transporters or transporting polypeptides OATP1B1 and OATP1B3 at clinically relevant concentrations in vitro. Overall, ertugliflozin is unlikely to affect the pharmacokinetics of concurrently administered medications that are substrates of these transporters. Metformin Absorption The absolute bioavailability of a metformin hydrochloride 500-mg tablet given under fasting conditions is approximately 50-60%. Studies using single oral doses of metformin hydrochloride tablets 500 mg to 1,500 mg, and 850 mg to 2,550 mg, indicate that there is a lack of dose proportionality with increasing doses, which is due to decreased absorption rather than an alteration in elimination. At usual clinical doses and dosing schedules of metformin hydrochloride tablets, steady- state plasma concentrations of metformin are reached within 24-48 hours and are generally <1 µg/mL. During controlled clinical trials of metformin, maximum metformin plasma levels did not exceed 5 µg/mL, even at maximum doses. Food decreases the extent of and slightly delays the absorption of metformin, as shown by approximately a 40% lower mean peak plasma concentration (Cmax), a 25% lower area under the plasma concentration versus time curve (AUC), and a 35-minute prolongation of time to peak plasma concentration (Tmax) following administration of a single 850-mg tablet of metformin with food, compared to the same tablet strength administered fasting. The clinical relevance of these decreases is unknown. Distribution The apparent volume of distribution (V/F) of metformin following single oral doses of metformin hydrochloride tablets 850 mg averaged 654 ± 358 l. Metformin is negligibly bound to plasma proteins. Metformin partitions into erythrocytes. Biotransformation Metformin is excreted unchanged in the urine. No metabolites have been identified in humans. Elimination Renal clearance is approximately 3.5 times greater than creatinine clearance, which indicates that tubular secretion is the major route of metformin elimination. Following oral administration, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination half-life of approximately 6.2 hours. Special populations Renal impairment In patients with decreased renal function, the plasma and blood half-life of metformin is prolonged and the renal clearance is decreased in proportion to the decrease in eGFR (see sections 4.3 and 4.4). Hepatic impairment No pharmacokinetic studies of metformin have been conducted in patients with hepatic insufficiency. Effects of age, body weight, gender and race Limited data from controlled pharmacokinetic studies of metformin in healthy elderly subjects suggest that total plasma clearance of metformin is decreased, the half-life is prolonged, and Cmax is increased, compared to healthy young subjects. From these data, it appears that the change in metformin pharmacokinetics with aging is primarily accounted for by a change in renal function. Metformin pharmacokinetic parameters did not differ significantly between normal subjects and patients with type 2 diabetes when analysed according to gender. Similarly, in controlled clinical studies in patients with type 2 diabetes, the antihyperglycaemic effect of metformin was comparable in males and females. No studies of metformin pharmacokinetic parameters according to race have been performed. In controlled clinical studies of metformin in patients with type 2 diabetes, the antihyperglycaemic effect was comparable in Whites (n=249), Blacks (n=51), and Hispanics (n=24).

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול בסוכרת בחולי סוכרת סוג 2 העונים על כל אלה:א. HbA1c בערך 7% ומעלה, על אף טיפול קודם למחלתם. ב. eGFR בערך 45 מ"ל/דקה/1.73 מ"ר ומעלה, או בערך גבוה יותר בהתאם לתנאי הרישום.ג. אבחנה של אחד מאלה:1. אוטם בשריר הלב 2. ניתוח מעקפים (CABG)3. מחלת לב איסכמית.4. אי ספיקה כלייתית המוגדרת כאחד מאלה, בהתאם לתנאי הרישום:א. eGFR נמוך מ-90 מ"ל/דקה ומאקרואלבומינוריה (מוגדרת כיחס קראטינין אלבומין מעל 300 מ"ג/גרם).ב. eGFR נמוך מ-90 מ"ל/דקה ומיקרואלבומינוריה (מוגדרת כיחס קראטינין אלבומין מעל 30 מ"ג/גרם).ג. eGFR נמוך מ-60 מ"ל/דקה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| סוכרת בחולי סוכרת סוג 2 העונים על כל אלה: א. HbA1c בערך 7% ומעלה, על אף טיפול קודם למחלתם. ב. eGFR בערך 45 מ"ל/דקה/1.73 מ"ר ומעלה, או בערך גבוה יותר בהתאם לתנאי הרישום. ג. אבחנה של אחד מאלה: 1. אוטם בשריר הלב 2. ניתוח מעקפים (CABG) 3. מחלת לב איסכמית. 4. אי ספיקה כלייתית המוגדרת כאחד מאלה, בהתאם לתנאי הרישום: א. eGFR נמוך מ-90 מ"ל/דקה ומאקרואלבומינוריה (מוגדרת כיחס קראטינין אלבומין מעל 300 מ"ג/גרם). ב. eGFR נמוך מ-90 מ"ל/דקה ומיקרואלבומינוריה (מוגדרת כיחס קראטינין אלבומין מעל 30 מ"ג/גרם). ג. eGFR נמוך מ-60 מ"ל/דקה. | 01/03/2021 | אנדוקרינולוגיה | DAPAGLIFLOZIN, ERTUGLIFLOZIN (L-PGA), EMPAGLIFLOZIN | סוכרת סוג 2 |
| סוכרת סוג 2 בחולים העונים על כל אלה: א. HbA1c בערך 7% ומעלה, על אף טיפול קודם למחלתם. ב. eGFR בערך 45 מ"ל/דקה/1.73 מ"ר ומעלה, או בערך גבוה יותר בהתאם לתנאי הרישום. ג. אבחנה של אחד מאלה: 1. אוטם בשריר הלב 2. ניתוח מעקפים (CABG) 3. מחלת לב איסכמית. 4. אי ספיקה כלייתית המוגדרת כאחד מאלה, בהתאם לתנאי הרישום: א. eGFR נמוך מ-90 מ"ל/דקה ומאקרואלבומינוריה (מוגדרת כיחס קראטינין אלבומין מעל 300 מ"ג/גרם). ב. eGFR נמוך מ-60 מ"ל/דקה. | 30/01/2020 | אנדוקרינולוגיה | DAPAGLIFLOZIN, ERTUGLIFLOZIN (L-PGA), EMPAGLIFLOZIN | סוכרת סוג 2 |
| סוכרת סוג 2 בחולים העונים על כל אלה: א. HbA1c בערך 7% ומעלה, על אף טיפול קודם למחלתם. ב. eGFR בערך 45 מ"ל/דקה/1.73 מ"ר ומעלה, או בערך גבוה יותר בהתאם לתנאי הרישום. ג. אבחנה של אחד מאלה: 1. אוטם בשריר הלב 2. ניתוח מעקפים (CABG) 3. מחלת לב איסכמית. | 12/01/2017 | אנדוקרינולוגיה | DAPAGLIFLOZIN, ERTUGLIFLOZIN (L-PGA), EMPAGLIFLOZIN | סוכרת סוג 2 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/01/2019
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
161 71 35635 00
מחיר
0 ₪
מידע נוסף
