Quest for the right Drug
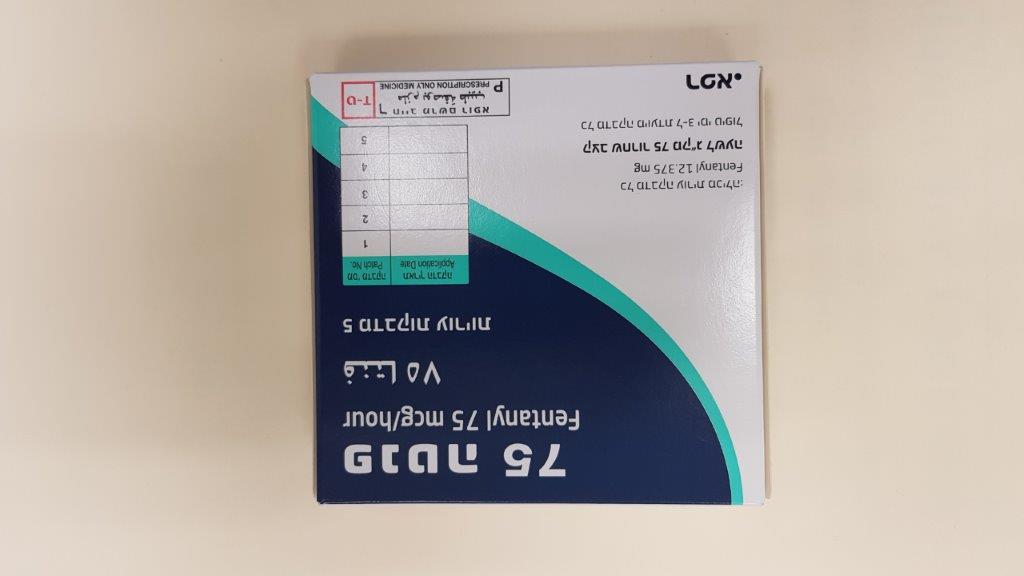
פנטה 75 FENTA 75 (FENTANYL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
בין-עורי : TRANSDERMAL
צורת מינון:
מדבקות : PATCHES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Patients who have experienced serious adverse events should be monitored for at least 24 hours after removal of Fenta TDP, or more, as clinical symptoms dictate, because serum fentanyl concentrations decline gradually and are reduced by about 50% 20 to 27 hours later. Patients and their carers must be instructed that Fenta TDP contains an active substance in an amount that can be fatal, especially to a child. Therefore, they must keep all patches out of the sight and reach of children, both before and after use. Because of the risks, including fatal outcome, associated with accidental ingestion, misuse, and abuse, patients and their carers must be advised to keep Fenta TDP in a safe and secure place, not accessible by others. Opioid-naive and not opioid-tolerant states Use of Fenta TDP in the opioid-naive patient has been associated with very rare cases of significant respiratory depression and/or fatality when used as initial opioid therapy, especially in patients with non-cancer pain. The potential for serious or life-threatening hypoventilation exists even if the lowest dose of Fenta TDP is used in initiating therapy in opioid-naive patients, especially in elderly or patients with hepatic or renal impairment. The tendency of tolerance development varies widely among individuals. Fenta TDP should only be used in patients who have demonstrated opioid tolerance (see section 4.2). Respiratory depression Some patients may experience significant respiratory depression with Fenta TDP; patients must be observed for these effects. Respiratory depression may persist beyond the removal of the Fenta TDP patch. The incidence of respiratory depression increases as the Fenta TDP dose is increased (see section 4.9). Opioids can cause sleep-related breathing disorders including central sleep apnoea (CSA) and sleep-related hypoxia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA consider decreasing the total opioid dosage. Risk from concomitant use of central nervous system (CNS) depressants, including sedative medicines such as benzodiazepines or related drugs, alcohol and CNS depressant narcotic drugs Concomitant use of Fenta TDP and sedative medicines such as benzodiazepines or related drugs, alcohol, or CNS depressant narcotic drugs, may result in sedation, respiratory depression, coma and death. Because of these risks, concomitant prescribing with sedative medicines should be reserved for patients for whom alternative treatment options are not possible. If a decision is made to prescribe Fenta TDP concomitantly with sedative medicines, the lowest effective dose should be used, and the duration of treatment should be as short as possible. The patients should be followed closely for signs and symptoms of respiratory depression and sedation. In this respect, it is strongly recommended to inform patients and their caregivers to be aware of these symptoms (see section 4.5). Chronic pulmonary disease Fenta TDP may have more severe adverse effects in patients with chronic obstructive or other pulmonary disease. In such patients, opioids may decrease respiratory drive and increase airway resistance. Long-term treatment effects and tolerance In all patients, tolerance to the analgesic effects, hyperalgesia, physical dependence, and psychological dependence may develop upon repeated administration of opioids, whereas incomplete tolerance is developed for some side effects like opioid induced constipation. Particularly in patients with chronic non cancer pain, it has been reported that they may not experience a meaningful amelioration in pain intensity from continuous opioid treatment in the long term. It is recommended to re-evaluate the appropriateness of continued use of Fenta TDP regularly at the time of prescription renewals in patients. When it is decided that there is no benefit for continuation, gradual down titration should be applied to address withdrawal symptoms. Do not abruptly discontinue Fenta TDP in a patient physically dependent on opioids. Drug withdrawal syndrome may occur upon abrupt cessation of therapy or dose reduction. There have been reports that rapid tapering of fentanyl transdermal patch in a patient physically dependent on opioids may lead to serious withdrawal symptoms and uncontrolled pain (see section 4.2 and section 4.8). When a patient no longer requires therapy, it is advisable to taper the dose gradually to minimise symptoms of withdrawal. Tapering from a high dose may take weeks to months. The opioid drug withdrawal syndrome is characterised by some or all of the following: restlessness, lacrimation, rhinorrhoea, yawning, perspiration, chills, myalgia, mydriasis and palpitations. Other symptoms may also develop including irritability, agitation, anxiety, hyperkinesia, tremor, weakness, insomnia, anorexia, abdominal cramps, nausea, vomiting, diarrhoea, increased blood pressure, increased respiratory rate or heart rate. Opioid use disorder (abuse and dependence) Repeated use of Fenta TDP may lead to Opioid use disorder (OUD). Abuse or intentional misuse of Fenta TDP may result in overdose and/or death. The risk of developing OUD is increased in patients with a personal or a family history (parents or siblings) of substance use disorders (including alcohol use disorder), in current tobacco users or in patients with a personal history of other mental health disorders (e.g. major depression, anxiety and personality disorders). Patients treated with opioid medications should be monitored for signs of OUD, such as drug-seeking behaviour (e.g. too early requests for refills), particularly with patients at increased risk. This includes the review of concomitant opioids and psycho-active drugs (like benzodiazepines). For patients with signs and symptoms of OUD, consultation with an addiction specialist should be considered. If opioid discontinuation is to occur see section 4.4. Central nervous system conditions including increased intracranial pressure Fenta TDP should be used with caution in patients who may be particularly susceptible to the intracranial effects of CO 2 retention such as those with evidence of increased intracranial pressure, impaired consciousness, or coma. Fenta TDP should be used with caution in patients with brain tumours. Cardiac disease Fentanyl may produce bradycardia and should therefore be administered with caution to patients with bradyarrhythmias. Hypotension Opioids may cause hypotension, especially in patients with acute hypovolaemia. Underlying, symptomatic hypotension and/or hypovolaemia should be corrected before treatment with fentanyl transdermal patches is initiated. Hepatic impairment Because fentanyl is metabolised to inactive metabolites in the liver, hepatic impairment might delay its elimination. If patients with hepatic impairment receive Fenta TDP, they should be observed carefully for signs of fentanyl toxicity and the dose of Fenta TDP reduced if necessary (see section 5.2). Renal impairment Even though impairment of renal function is not expected to affect fentanyl elimination to a clinically relevant extent, caution is advised because fentanyl pharmacokinetics has not been evaluated in this patient population (see section 5.2). Treatment should only be considered if the benefits outweigh the risks. If patients with renal impairment receive Fenta TDP, they should be observed carefully for signs of fentanyl toxicity and the dose reduced if necessary. Fever/external heat application Fentanyl concentrations may increase if the skin temperature increases (see section 5.2). Therefore, patients with fever should be monitored for opioid undesirable effects and the Fenta TDP dose should be adjusted if necessary. There is a potential for temperature-dependent increases in fentanyl released from the system resulting in possible overdose and death. All patients should be advised to avoid exposing the Fenta TDP application site to direct external heat sources such as heating pads, electric blankets, heated water beds, heat or tanning lamps, sunbathing, hot water bottles, prolonged hot baths, saunas and hot whirlpool spa baths. Serotonin syndrome Caution is advised when Fenta TDP is co-administered with medicinal products that affect the serotonergic neurotransmitter systems. The development of a potentially life-threatening serotonin syndrome may occur with the concomitant use of serotonergic active substances such as Selective Serotonin Re-uptake Inhibitors (SSRIs) and Serotonin Norepinephrine Re-uptake Inhibitors (SNRIs), and with active substances that impair metabolism of serotonin (including Monoamine Oxidase Inhibitors [MAOIs]). This may occur within the recommended dose (see section 4.5). Serotonin syndrome may include mental-status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular abnormalities (e.g., hyperreflexia, incoordination, rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhoea). If serotonin syndrome is suspected, treatment with Fenta TDP should be discontinued. Interactions with other medicinal products CYP3A4 inhibitors The concomitant use of Fenta TDP with cytochrome P450 3A4 (CYP3A4) inhibitors may result in an increase in fentanyl plasma concentrations, which could increase or prolong both the therapeutic and adverse effects, and may cause serious respiratory depression. Therefore, the concomitant use of Fenta TDP and CYP3A4 inhibitors is not recommended unless the benefits outweigh the increased risk of adverse effects. Generally, a patient should wait for 2 days after stopping treatment with a CYP3A4 inhibitor before applying the first Fenta transdermal patch. However, the duration of inhibition varies and for some CYP3A4 inhibitors with a long elimination half-life, such as amiodarone, or for time-dependent inhibitors such as erythromycin, idelalisib, nicardipine and ritonavir, this period may need to be longer. Therefore, the product information of the CYP3A4 inhibitor must be consulted for the active substance's half-life and duration of the inhibitory effect before applying the first Fenta transdermal patch. A patient who is treated with Fenta TDP should wait at least 1 week after removal of the last patch before initiating treatment with a CYP3A4 inhibitor. If concomitant use of Fenta TDP with a CYP3A4 inhibitor cannot be avoided, close monitoring for signs or symptoms of increased or prolonged therapeutic effects and adverse effects of fentanyl (in particular respiratory depression) is warranted, and the Fenta TDP dosage must be reduced or interrupted as deemed necessary (see section 4.5). Accidental exposure by patch transfer Accidental transfer of a fentanyl patch to the skin of a non-patch wearer (particularly a child), while sharing a bed or being in close physical contact with a patch wearer, may result in an opioid overdose for the non-patch wearer. Patients should be advised that if accidental patch transfer occurs, the transferred patch must be removed immediately from the skin of the non-patch wearer (see section 4.9). Use in elderly patients Data from intravenous studies with fentanyl suggest that elderly patients may have reduced clearance, a prolonged half life, and they may be more sensitive to the active substance than younger patients. If elderly patients receive Fenta TDP, they should be observed carefully for signs of fentanyl toxicity and the dose reduced if necessary (see section 5.2). Gastrointestinal tract Opioids increase the tone and decrease the propulsive contractions of the smooth muscle of the gastrointestinal tract. The resultant prolongation in gastrointestinal transit time may be responsible for the constipating effect of fentanyl. Patients should be advised on measures to prevent constipation and prophylactic laxative use should be considered. Extra caution should be used in patients with chronic constipation. If paralytic ileus is present or suspected, treatment with Fenta TDP should be stopped. Patients with myasthenia gravis Non-epileptic (myo)clonic reactions can occur. Caution should be exercised when treating patients with myasthenia gravis. Concomitant use of mixed opioid agonists/antagonists The concomitant use of buprenorphine, nalbuphine or pentazocine is not recommended (see section 4.5). Paediatric population Fenta TDP should not be administered to opioid-naive paediatric patients (see section 4.2). The potential for serious or life-threatening hypoventilation exists regardless of the dose of Fenta TDP transdermal system administered. Fentanyl transdermal patch has not been studied in children under 2 years of age. Fenta TDP should be administered only to opioid-tolerant children age 2 years or older (see section 4.2). To guard against accidental ingestion by children, use caution when choosing the application site for Fenta TDP (see sections 4.2 and 6.6) and monitor adhesion of the patch closely. Opioid induced hyperalgesia Opioid induced hyperalgesia (OIH) is a paradoxical response to an opioid in which there is an increase in pain perception despite stable or increased opioid exposure. It differs from tolerance, in which higher opioid doses are required to achieve the same analgesic effect or treat recurring pain. OIH may manifest as increased levels of pain, more generalised pain (i.e., less focal), or pain from ordinary (i.e. non-painful) stimuli (allodynia) with no evidence of disease progression. When OIH is suspected, the dose of opioid should be reduced or tapered off, if possible.
Effects on Driving
4.7 Effects on ability to drive and use machines Fenta TDP may impair mental and/or physical ability required for the performance of potentially hazardous tasks such as driving or operating machinery. This medicine can impair cognitive function and can affect a patient's ability to drive safely. When prescribing this medicine, patients should be told: • The medicine is likely to affect your ability to drive • Do not drive until you know how the medicine affects you

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2000
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
07.08.22 - עלון לצרכן אנגלית 07.08.22 - עלון לצרכן עברית 07.08.22 - עלון לצרכן ערבית 04.01.23 - עלון לצרכן עברית 06.03.23 - עלון לצרכן אנגלית 06.03.23 - עלון לצרכן עברית 06.03.23 - עלון לצרכן ערבית 16.08.23 - עלון לצרכן אנגלית 16.08.23 - עלון לצרכן עברית 16.08.23 - עלון לצרכן ערבית 23.05.19 - החמרה לעלון 13.06.19 - החמרה לעלון 28.02.22 - החמרה לעלון 18.01.15 - החמרה לעלון 04.01.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פנטה 75