Quest for the right Drug
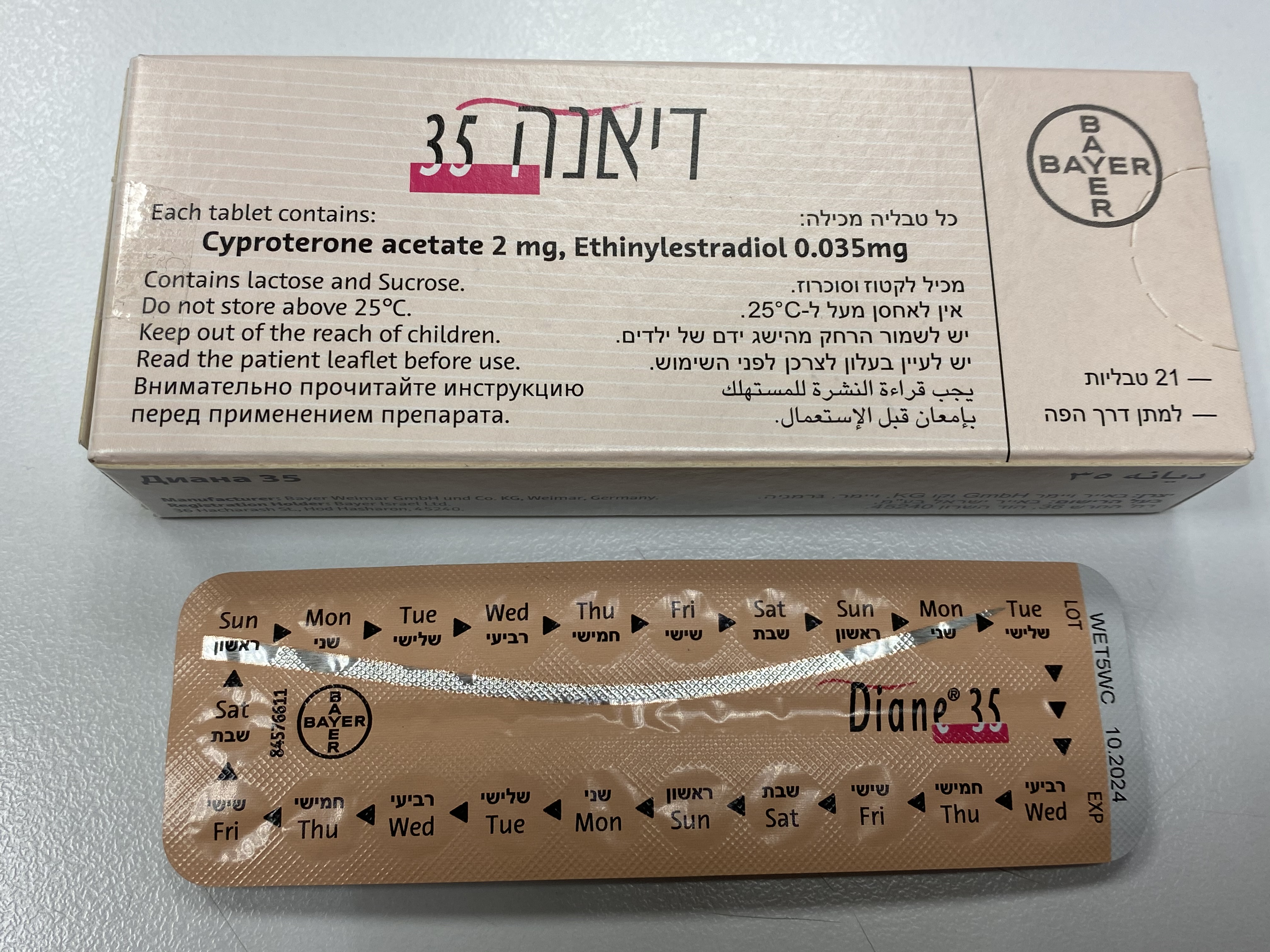
דיאנה 35 DIANE ® 35 (CYPROTERONE ACETATE, ETHINYLESTRADIOL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Medical Examination Assessment of women prior to starting oral contraceptives (and at regular intervals thereafter) should include a personal and family medical history of each woman. Physical examination should be guided by this and by the contraindications (section 4.3) and warnings (section 4.4) for this product. The frequency and nature of these assessments should be based upon relevant guidelines and should be adapted to the individual woman, but should include measurement of blood pressure and, if judged appropriate by the clinician, breast, abdominal and pelvic examination including cervical cytology. Exclude the likelihood of pregnancy before starting treatment. Undiagnosed vaginal bleeding that is suspicious for underlying conditions should be investigated. Warnings: Diane 35 is composed of the progestogen cyproterone acetate and the oestrogen ethinylestradiol and is administered for 21 days of a monthly cycle. It has a similar composition to that of a combined oral contraceptive (COC). Duration of Use Time to relief of symptoms is at least three months. The need to continue treatment should be evaluated periodically by the treating physician (see section 4.2). Women should be advised that Diane 35 does not protect against HIV infections (AIDS) and other sexually transmitted diseases. Conditions which require strict medical supervision If any of the conditions/risk factors mentioned below is present, the benefits of the use of Diane 35 should be weighed against the possible risks for each individual woman and discussed with the woman before she decides to start using Diane 35. In the event of aggravation, exacerbation or first appearance of any of these conditions or risk factors, the woman should contact her physician. The physician should then decide on whether the use of Diane 35 should be discontinued. • Diabetes mellitus, with mild vascular disease or mild nephropathy, retinopathy or neuropathy • Hypertension that is adequately controlled, i.e. systolic >140 to159 mmHg or diastolic > 90 to 94 mmHg (see also Section 4.4 'Reasons for stopping Diane 35 immediately') • porphyria • clinical depression • obesity • migraine • cardiovascular diseases • chloasma Patients with a history of depression or any condition mentioned above should be monitored during treatment with Diane 35. Depressed mood and depression are well-known undesirable effects of hormonal contraceptive use (see section 4.8). Depression can be serious and is a well-known risk factor for suicidal behaviour and suicide. Women should be advised to contact their physician in case of mood changes and depressive symptoms, including shortly after initiating the treatment. Reasons for stopping Diane 35 immediately: When stopping oral contraception non-hormonal contraception should be used to ensure contraceptive protection is maintained, if needed. 1. Occurrence for the first time, or exacerbation, of migrainous headaches or unusually frequent or unusually severe headaches. 2. Sudden disturbances of vision or hearing or other perceptual disorders. 3. First signs of thrombosis or blood clots (e.g. unusual pains in or swelling of the leg(s), stabbing pains on breathing or coughing for no apparent reason). Feeling of pain and tightness in the chest. 4. At least four weeks before an elective major operation (e.g. abdominal, orthopaedic), any surgery to the legs, medical treatment for varicose veins or prolonged immobilisation, e.g. after accidents or surgery. Do not restart until 2 weeks after full ambulation. In case of emergency surgery, thrombotic prophylaxis is usually indicated e.g. subcutaneous heparin. 5. Onset of jaundice, hepatitis, itching of the whole body. 6. Significant rise in blood pressure. 7. Onset of severe depression. 8. Severe upper abdominal pain or liver enlargement. 9. Clear worsening of conditions known to deteriorate during use of hormonal contraception or during pregnancy (see section 4.4 ‘Conditions which deteriorate in pregnancy or during previous COC use’ under ‘Other conditions’. 10. Pregnancy is a reason for stopping immediately (see section 4.6) Circulatory disorders • The use of Diane 35 carries an increased risk of venous thromboembolism (VTE) compared with no use. The excess risk of VTE is highest during the first year a woman starts Diane 35 or when restarting or switching after a pill-free interval of at least a month. Venous thromboembolism can be fatal in 1-2% of cases. • Epidemiological studies have shown that the incidence of VTE is 1.5 to 2 times higher in users of Diane 35 than in users of levonorgestrel-containing combined oral contraceptives (COCs) and may be similar to the risk for desogestrel / gestodene / drospirenone-containing COCs. • The user group of Diane 35 is likely to include patients that may have an inherently increased cardiovascular risk such as that associated with polycystic ovarian syndrome. • Epidemiological studies have also associated the use of hormonal contraceptive with an increased risk for arterial (myocardial infarction, transient ischaemic attack) thromboembolism. • Extremely rarely, thrombosis has been reported to occur in other blood vessels, e.g. hepatic, mesenteric, renal, cerebral or retinal veins and arteries, in hormonal contraceptive users. • Symptoms of venous or arterial thrombosis or of a cerebrovascular accident can include: unusual unilateral leg pain and / or swelling; sudden severe pain in the chest, whether or not it radiates to the left arm; sudden breathlessness; sudden onset of coughing; any unusual, severe, prolonged headache; sudden partial or complete loss of vision; diplopia; slurred speech or aphasia; vertigo; collapse with or without focal seizure; weakness or very marked numbness suddenly affecting one side or one part of the body; motor disturbances; ‘acute’ abdomen. • The risk of venous thromboembolic events increases with: − increasing age; − smoking (with heavier smoking and increasing age the risk further increases, especially in women over 35 years of age. Women over 35 years of age should be strongly advised not to smoke if they wish to use Diane 35); − a positive family history (i.e. venous thromboembolism ever in a sibling or parent at a relatively early age). If a hereditary predisposition is suspected, the woman should be referred to a specialist for advice before deciding about any hormonal contraceptive use; − prolonged immobilisation, major surgery, any surgery to the legs, or major trauma. In these situations it is advisable to discontinue use (in the case of elective surgery at least four weeks in advance) and not to resume until two weeks after complete remobilisation. Antithrombotic treatment should be considered if the use of Diane 35 has not been discontinued in advance. − obesity (body mass index over 30 kg/m2). There is no consensus about the possible role of varicose veins and superficial thrombophlebitis in venous thromboembolism. • The risk of arterial thromboembolic complications or of a cerebrovascular accident increases with: − increasing age − smoking (with heavier smoking and increasing age the risk further increases, especially in women over 35 years of age. Women over 35 years of age should be strongly advised not to smoke if they wish to use Diane 35); − dyslipoproteinemia; − obesity (body mass index over 30 kg/m2); − hypertension; − migraine; − valvular heart disease; − atrial fibrillation; − a positive family history (arterial thrombosis ever in a sibling or parent at a relatively early age). If a hereditary predisposition is suspected, the woman should be referred to a specialist for advice before deciding about any hormonal contraceptive use. Other medical conditions, which have been associated with adverse circulatory events, include diabetes mellitus, systemic lupus erythematosus, hemolytic uraemic syndrome, chronic inflammatory bowel disease (e.g. Crohn's disease or ulcerative colitis) and sickle cell disease. The increased risk of thromboembolism in the puerperium must be considered (for information on ‘Pregnancy and lactation’ see section 4.6). An increase in frequency or severity of migraine during use of Diane 35 (which may be prodromal of a cerebrovascular event) may be a reason for immediate discontinuation of Diane 35. Women using Diane 35 should be specifically pointed out to contact their physician in case of possible symptoms of thrombosis. In case of suspected or confirmed thrombosis, Diane 35 use should be discontinued. Adequate contraception should be initiated because of the teratogenicity of anti-coagulant therapy (coumarins). • Other factors affecting circulatory events The user group of Diane 35 as a treatment for acne or moderately severe hirsutism is likely to include patients that may have an inherently increased cardiovascular risk such as that associated with polycystic ovarian syndrome. Biochemical factors that may be indicative of hereditary or acquired predisposition for venous or arterial thrombosis include Activated Protein C (APC) resistance, hyperhomocysteinaemia, antithrombin-III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant). When considering risk/benefit, the physician should take into account that adequate treatment of a condition may reduce the associated risk of thrombosis and that the risk associated with pregnancy is higher than that associated with COC or Diane 35 use. Tumours Like many other steroids, Diane 35, when given in very high doses and for the majority of the animal's life-span, has been found to cause an increase in the incidence of tumours, including carcinoma, in the liver of rats. The relevance of this finding to humans is unknown. Numerous epidemiological studies have been reported on the risks of ovarian, endometrial, cervical and breast cancer in women using combined oral contraceptives. The evidence is clear that high dose combined oral contraceptives offer substantial protection against both ovarian and endometrial cancer. However, it is not clear whether low dose COCs or Diane 35 confer protective effects to the same level. • Breast cancer A meta-analysis from 54 epidemiological studies reported that there is a slightly increased relative risk (RR = 1.24) of having breast cancer diagnosed in women who are currently using combined oral contraceptives (COCs). The observed pattern of increased risk may be due to an earlier diagnosis of breast cancer in COC users, the biological effects of COCs or a combination of both. The additional breast cancers diagnosed in current users of COCs or in women who have used COCs in the last ten years are more likely to be localised to the breast than those in women who never used COCs. Breast cancer is rare among women under 40 years of age whether or not they take COCs. Whilst this background risk increases with age, the excess number of breast cancer diagnoses in current and recent COC users is small in relation to the overall risk of breast cancer (see bar chart). The most important risk factor for breast cancer in COC users is the age women discontinue the COC; the older the age at stopping, the more breast cancers are diagnosed. Duration of use is less important and the excess risk gradually disappears during the course of the 10 years after stopping COC use such that by 10 years there appears to be no excess. The possible increase in risk of breast cancer should be discussed with the user and weighed against the benefits of COCs taking into account the evidence that they offer substantial protection against the risk of developing certain other cancers (e.g. ovarian and endometrial cancer). Estimated cumulative numbers of breast cancers per 10,000 women diagnosed in 5 years of use and up to 10 years after stopping COCs, compared with numbers of breast cancers diagnosed in 10,000 women who had never used COCs • Cervical Cancer The most important risk factor for cervical cancer is persistent HPV infection. Some epidemiological studies have indicated that long-term use of COCs may further contribute to this increased risk but there continues to be controversy about the extent to which this finding is attributable to confounding effects, e.g., cervical screening and sexual behaviour including use of barrier contraceptives. • Liver Cancer In rare cases benign and in even rarer cases malignant liver tumours leading in isolated cases to life- threatening intra -abdominal haemorrhage have been observed after the use of hormonal substances such as those contained in Diane 35. If severe upper abdominal complaints, liver enlargement or signs of intra-abdominal haemorrhage occur, a liver tumour should be included in the differential diagnosis. • Meningioma The occurrence of meningiomas (single and multiple) has been reported in association with use of cyproterone acetate, especially at high doses of 25 mg and above and for prolonged time (see section 5.1). If a patient is diagnosed with meningioma, any cyproterone containing treatment, including Diane 35, must be stopped, as a precautionary measure. Other conditions The possibility cannot be ruled out that certain chronic diseases may occasionally deteriorate during the use of Diane 35. • Known hyperlipidaemias Women with hypertriglyceridemia, or a family history thereof, may be at an increased risk of pancreatitis when using COCs or Diane 35. Women with hyperlipidaemias are at an increased risk of arterial disease (see section 4.4 ‘Circulatory disorders’). However routine screening of women on COCs or Diane 35 is not appropriate. • Blood pressure Hypertension is a risk factor for stroke and myocardial infarction (see section 4.4 ‘Arterial thromboembolic-related conditions’). Although small increases in blood pressure have been reported in many women taking COCs or oestrogen/progestogen combinations like Diane 35, clinically relevant increases are rare. However, if sustained hypertension develops during the use of Diane 35, antihypertensive treatment should normally be instigated at a level of 160/100 mm Hg in uncomplicated patients or at 140/90 mm Hg in those with target organ damage, established cardiovascular disease, diabetes or with increased cardiovascular risk factors. Decisions about the continued use of Diane 35, should be made at lower BP levels, and alternative contraception may be advised. • Conditions which deteriorate with pregnancy or during previous COC or Diane 35 use: The following conditions have been reported to occur or deteriorate with both pregnancy and use of a COC or oestrogen/progestogen combinations like Diane 35. Consideration should be given to stopping Diane 35 if any of the following occur during use: • jaundice and/or pruritus related to cholestasis • COCs or Diane 35 may increase the risk of gallstone formation and may worsen existing disease • systemic lupus erythematosus • herpes gestationis • otosclerosis-related hearing loss • sickle cell anaemia • renal dysfunction • hereditary angioedema • epilepsy • any other condition an individual woman has experienced worsening of during pregnancy or previous use of COCs or Diane 35. • Angioedema Exogenous oestrogens may induce or exacerbate symptoms of hereditary and acquired angioedema. • Disturbances of liver function Acute or chronic disturbances of liver function may necessitate the discontinuation of COC or Diane 35 use until markers of liver function return to normal. • Diabetes (without vascular involvement) Insulin-dependent diabetics without vascular disease can use Diane 35. However it should be remembered that all diabetics are at an increased risk of arterial disease and this should be considered when prescribing COCs or Diane 35. Diabetics with existing vascular disease are contraindicated from using Diane 35 (see section 4.3 Contraindications). Although COCs or oestrogen/progestogen combinations like Diane 35 may have an effect on peripheral insulin resistance and glucose tolerance, there is no evidence for a need to alter the therapeutic regimen in diabetics using low-dose COCs (containing < 0.05 mg ethinylestradiol). However, diabetic women should be carefully observed while taking COCs or Diane 35. • Chloasma Chloasma may occasionally occur, especially in women with a history of chloasma gravidarum. Women with a tendency to chloasma should avoid exposure to the sun or ultraviolet radiation whilst taking Diane 35. • Menstrual Changes Reduction of menstrual flow: This is not abnormal and it is to be expected in some patients. Indeed, it may be beneficial where heavy periods were previously experienced. Missed menstruation: Occasionally, withdrawal bleeding may not occur at all. If the tablets have been taken correctly, pregnancy is unlikely. Should bleeding fail to occur during the tablet-free interval the possibility of pregnancy must be excluded before the next pack is started. Intermenstrual bleeding: Irregular bleeding (spotting or breakthrough bleeding) may occur especially during the first months of use. Therefore, the evaluation of any irregular bleeding is only meaningful after an adaptation interval of about three cycles. If bleeding irregularities persist or occur after previously regular cycles, then non-hormonal causes should be considered and adequate diagnostic measures are indicated to exclude malignancy or pregnancy. This may include curettage. Some women may experience amenorrhoea or oligomenorrhoea after discontinuation of Diane 35, especially when these conditions existed prior to use. Women should be informed of this possibility. • Lactose and Sucrose Intolerance Each tablet of this medicinal product contains 30.965 mg lactose monohydrate and 19.371 mg sucrose per tablet. Patients with rare hereditary problems of galactose intolerance, total lactase deficiency, fructose intolerance or glucose-galactose malabsorption or sucrase-isomaltase should not take this medicine
Effects on Driving
4.7 Effects on ability to drive and use machines None known.

שימוש לפי פנקס קופ''ח כללית 1994
Signs of androgenization in women
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
29.05.22 - עלון לצרכן אנגלית 29.05.22 - עלון לצרכן עברית 29.05.22 - עלון לצרכן ערבית 11.06.23 - עלון לצרכן עברית 30.11.23 - עלון לצרכן אנגלית 30.11.23 - עלון לצרכן עברית 30.11.23 - עלון לצרכן ערבית 09.05.13 - החמרה לעלון 03.12.13 - החמרה לעלון 21.08.14 - החמרה לעלון 20.10.15 - החמרה לעלון 06.10.20 - החמרה לעלון 06.07.21 - החמרה לעלון 14.12.21 - החמרה לעלון 11.06.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
דיאנה 35