Quest for the right Drug
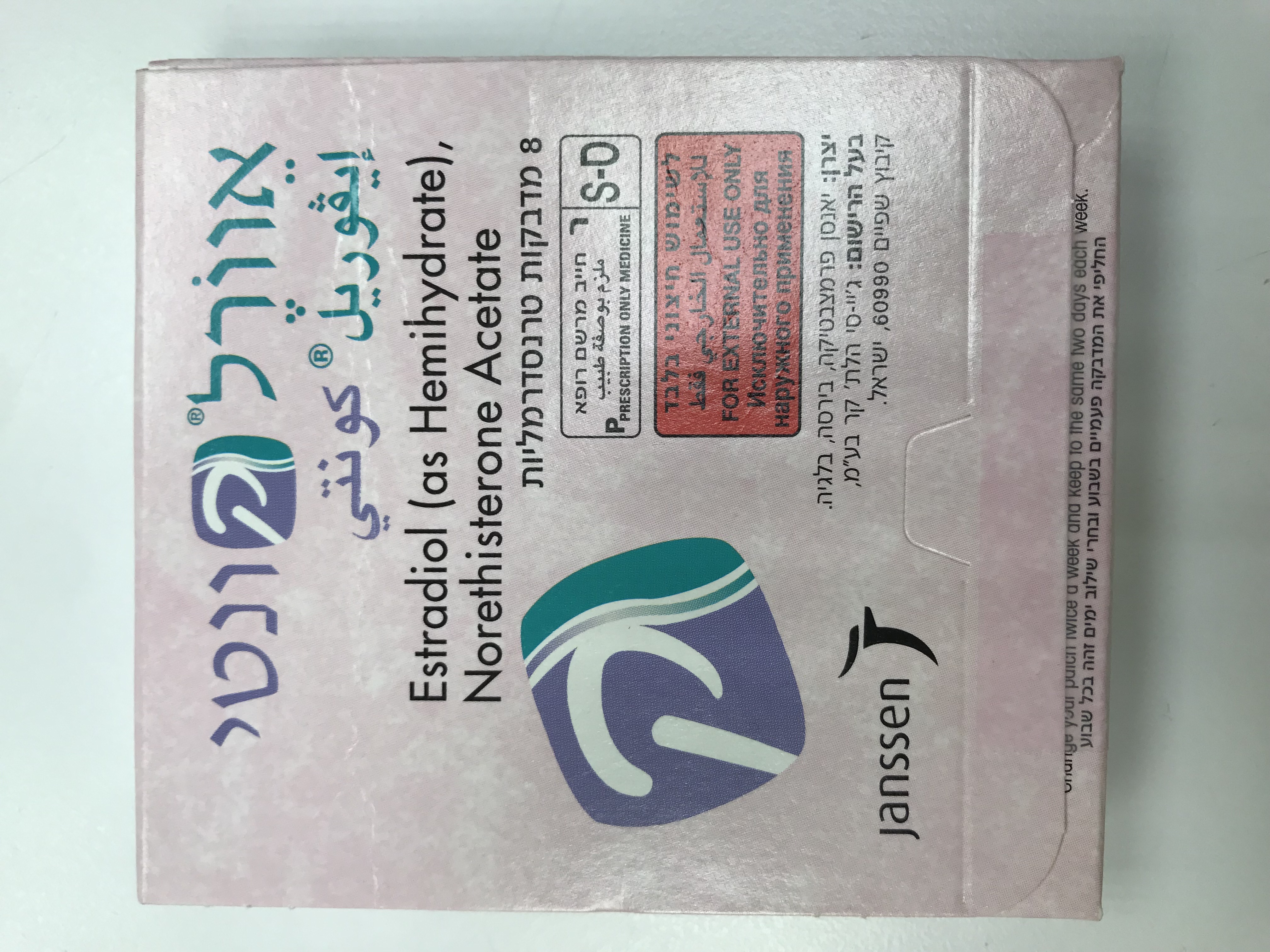
אוורל קונטי EVOREL CONTI (ESTRADIOL AS HEMIHYDRATE, NORETHISTERONE ACETATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
בין-עורי : TRANSDERMAL
צורת מינון:
מדבקות : PATCHES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects The safety of Evorel Conti was evaluated in 196 subjects who participated in 3 clinical trials and received at least one administration of Evorel Conti. Based on safety data from these clinical trials, the most commonly reported (≥5% incidence) adverse drug reactions (ADRs) were (with % incidence): application site reaction (11.7%), menstrual disorder (7.1%), headache (8.2%), and breast pain (5.1%). Including the above-mentioned ADRs, the following table displays ADRs that have been reported with the use of Evorel Conti from either clinical trial or post- marketing experiences, and additional ADRs that have been reported with the use of Evorel (estradiol alone) from clinical trial data. The displayed frequency categories use the following convention: Very common (>1/10); common (>1/100 to <1/10); uncommon (>1/1,000 to <1/100); rare (>1/10,000 to <1/1,000); very rare (<1/10,000); and not known (cannot be estimated from the available clinical trial data). Adverse Drug Reactions Infections and Infestations Uncommon Candidiasis Neoplasms benign, malignant and unspecified (including cysts and polyps) Frequency not known Breast neoplasms, Endometrial cancer Immune System Disorders Common Hypersensitivity Psychiatric disorders Common Depression, Insomnia, Anxiety, Nervousness Uncommon Libido decreased Frequency not known Mood swings Nervous system disorders Common Paraesthesia, Headache Uncommon Migraine Rare Epilepsy* Frequency not known Cerebrovascular accident, Dizziness Cardiac disorders Common Palpitations Vascular disorders Common Hypertension, Varicose vein, Vasodilatation Rare Thrombosis* Frequency not known Deep vein thrombosis, Respiratory, Thoracic and Mediastinal Disorders Frequency not known Pulmonary embolism Gastrointestinal disorders Common Abdominal pain, Diarrhoea*, Nausea Uncommon Flatulence* Frequency not known Abdominal distension Hepato-biliary disorders Frequency not known Cholelithiasis Skin and subcutaneous tissue disorders Common Rash erythematous Uncommon Pruritus, Rash*, Frequency not known Stevens-Johnson syndrome Musculoskeletal and Connective Tissue Disorders Common Arthralgia, Back pain Uncommon Myalgia* Reproductive system and breast disorders Common Breast pain, Cervical polyp, Endometrial hyperplasia, Genital discharge, Dysmenorrhoea, Menorrhagia, Menstrual disorder, Metrorrhagia Frequency not known Breast enlargement General disorders and administration site conditions Very Common Application site erythema, Application site pruritus, Application site rash, Application site reaction Common Pain*, Oedema, Application site oedema* Fatigue Uncommon Generalised oedema, Oedema peripheral*, Investigations Common Weight increased * Additional adverse drug reactions reported in clinical trials of Evorel (estradiol only). The table below reports additional undesirable effects that have been reported in users of other hormone replacement therapy (HRT) by MedDRA system organ classes (MedDRA SOCs). Psychiatric disorders Common Affect lability Nervous system disorders Uncommon Vertigo Gastrointestinal disorders Common Dyspepsia Uncommon Vomiting Hepatobiliary disorders Rare Gallbladder disorder, Very rare Cholestatic jaundice Skin and subcutaneous tissue Common Acne, Dry skin Uncommon Skin discolouration Frequency not known Alopecia Musculoskeletal and connective tissue disorders Common Pain in extremity Rare Myasthenia Reproductive system and breast disorders Very Common Breast tenderness Common Uterine spasms, Vaginal infection Rare Uterine leiomyoma, Fallopian tube cysts, Investigations Uncommon Transaminases increase Breast Cancer Risk An up to 2-fold increased risk of having breast cancer diagnosed is reported in women taking combined oestrogen-progestogen therapy for more than 5 years. - The increased risk in users of oestrogen-only therapy is substantially lower than that seen in users of oestrogen-progestogen combinations. - The level of risk is dependent on the duration of use (see section 4.4). - Absolute risk estimations based on results of the largest randomised placebo- controlled trial (WHI-study) and the largest meta-analysis of prospective epidemiological studies are presented. Largest meta-analysis of prospective epidemiological studies– Estimated additional risk of breast cancer after 5 years’ use in women with BMI 27 (kg/m2) Age at start HRT Incidence per Risk ratio Additional cases per (years) 1000 never-users of 1000 HRT users after HRT over a 5 year 5 years period (50-54 years)* Oestrogen only HRT 50 13.3 1.2 2.7 Combined oestrogen-progestagen 50 13.3 1.6 8.0 *Taken from baseline incidence rates in England in 2015 in with BMI 27 (kg/m2). Note: since the background incidence of breast cancer differs by EU country, the number of additional cases of breast cancer differs by EU country; the number of additional cases of breast cancer will also change proportionately. Estimated additional risk of breast cancer after 10 years’ use in women with BMI 27 (kg/m2) Additional cases Incidence Risk ratio Additional cases per 1000 HRT Age at start HRT per 1000 never-users of HRT users after 10 years (years) over a 10 year period (50-59 years) * Oestrogen only HRT 7.1 50 26.6 1.3 Combined oestrogen-progestagen 20.8 50 26.6 1.8 *Taken from baseline incidence rates in England in 2015 in women with BMI 27 (kg/m2) Note: Since the background incidence of breast cancer differs by EU country, the number of additional cases of breast cancer will also change proportionately. US WHI studies - additional risk of breast cancer after 5 year’s use Age range (years) Incidence per 1000 Risk ratio & 95%CI Additional cases per 1000 women in placebo arm HRT users over 5 years over 5 years (95% CI) CEE oestrogen only 50-79 21 0.8 (0.7-1.0) -4 (-6 - 0)* ‡ CEE + MPA oestrogen & progestagens ‡ 50-79 17 1.2 (1.0-1.5) +4 (0 - 9) ‡ When the analysis was restricted to women who had not used HRT prior to the study there was no increased risk apparent during the first 5 years of treatment: after 5 years the risk was higher than in non- users. * WHI study in women with no uterus, which did not show an increase of breast cancer. Endometrial Cancer Risk Postmenopausal women with a uterus The endometrial cancer risk is about 5 in every 1000 women with a uterus not using HRT. In women with a uterus, use of oestrogen-only HRT is not recommended because it increases the risk of endometrial cancer (see section 4.4). Depending on the duration of oestrogen-only use and oestrogen dose, the increase in risk of endometrial cancer in epidemiology studies varied from between 5 and 55 extra cases diagnosed in every 1000 women between the ages of 50 and 65. Adding a progestogen to oestrogen-only therapy for at least 12 days per cycle can prevent this increased risk. In the Million Women Study, the use of five years of combined (sequential or continuous) HRT did not increase risk of endometrial cancer (RR of 1.0 (0.8-1.2)). Ovarian cancer Use of oestrogen-only or combined oestrogen-progestogen HRT has been associated with a slightly increased risk of having ovarian cancer diagnosed (see Section 4.4). A meta-analysis from 52 epidemiological studies reported an increased risk of ovarian cancer in women currently using HRT compared to women who have never used HRT (RR 1.43, 95% CI 1.31-1.56). For women aged 50 to 54 years taking 5 years of HRT, this results in about 1 extra case per 2000 users. In women aged 50 to 54 who are not taking HRT, about 2 women in 2000 will be diagnosed with ovarian cancer over a 5-year period. Risk of venous thromboembolism HRT is associated with a 1.3-3-fold increased relative risk of developing venous thromboembolism (VTE), i.e. deep vein thrombosis or pulmonary embolism. The occurrence of such an event is more likely in the first year of using HT (see section 4.4). Results of the WHI studies are presented: WHI Studies - Additional risk of VTE over 5 years’ use Age range Incidence per 1000 women Risk ratio & 95%CI Additional cases per 1000 (years) in placebo arm over 5 HRT users years Oral, oestrogen-only* 50-59 7 1.2 (0.6 - 2.4) 1 (-3 - 10) Oral combined, oestrogen -progesterone 50-59 4 2.3 (1.2 - 4.3) 5 (1 - 13) * Study in women with no uterus. Risk of coronary artery disease The risk of coronary artery disease is slightly increased in users of combined oestrogen-progestogen HRT over the age of 60 (see section 4.4). Risk of ischaemic stroke • The use of oestrogen-only and oestrogen + progestogen therapy is associated with an up to 1.5 fold increased relative risk of ischaemic stroke. The risk of haemorrhagic stroke is not increased during use of HRT. • This relative risk is not dependent on age or on duration of use, but as the baseline risk is strongly age- dependent, the overall risk of stroke in women who use HRT will increase with age (see section 4.4). WHI studies combined - Additional risk of ischaemic stroke* over 5 years’ use. Age range Incidence per 1000 women Risk ratio & 95%CI Additional cases per 1000 (years) in placebo arm over 5 years HRT users over 5 years 50-59 8 1.3 (1.1 – 1.6) 3 (1 – 5) * No differentiation was made between ischaemic and haemorrhagic stroke. Adverse events which have been reported in association with oestrogen/ progestogen treatment: Venous thrombo-embolism, ie deep leg or pelvic venous thrombosis and pulmonary embolism, is more frequent among hormone HRT users than among non-users. For further information see Section 4.3 Contra-indications and 4.4 Special warnings and precautions for use. Other adverse reactions have been reported in association with oestrogen/progestogen treatment: • Gall bladder disease • Skin and subcutaneous disorders: chloasma, erythema multiforme, erythema nodosum, vascular purpura • Probable dementia over the age of 65 (see section 4.4) • Dry eyes • Tear film composition changes Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form http://sideeffects.health.gov.il

שימוש לפי פנקס קופ''ח כללית 1994
Menopausal & post menopausal estrogen replacement therapy
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לרופא
07.08.22 - עלון לרופאעלון מידע לצרכן
01.03.22 - עלון לצרכן אנגלית 07.08.22 - עלון לצרכן עברית 01.03.22 - עלון לצרכן ערבית 19.09.22 - עלון לצרכן אנגלית 19.09.22 - עלון לצרכן עברית 19.09.22 - עלון לצרכן ערבית 23.11.23 - עלון לצרכן עברית 30.11.23 - עלון לצרכן אנגלית 30.11.23 - עלון לצרכן עברית 30.11.23 - עלון לצרכן ערבית 01.12.11 - החמרה לעלון 22.07.15 - החמרה לעלון 09.01.22 - החמרה לעלון 07.08.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אוורל קונטי