Quest for the right Drug
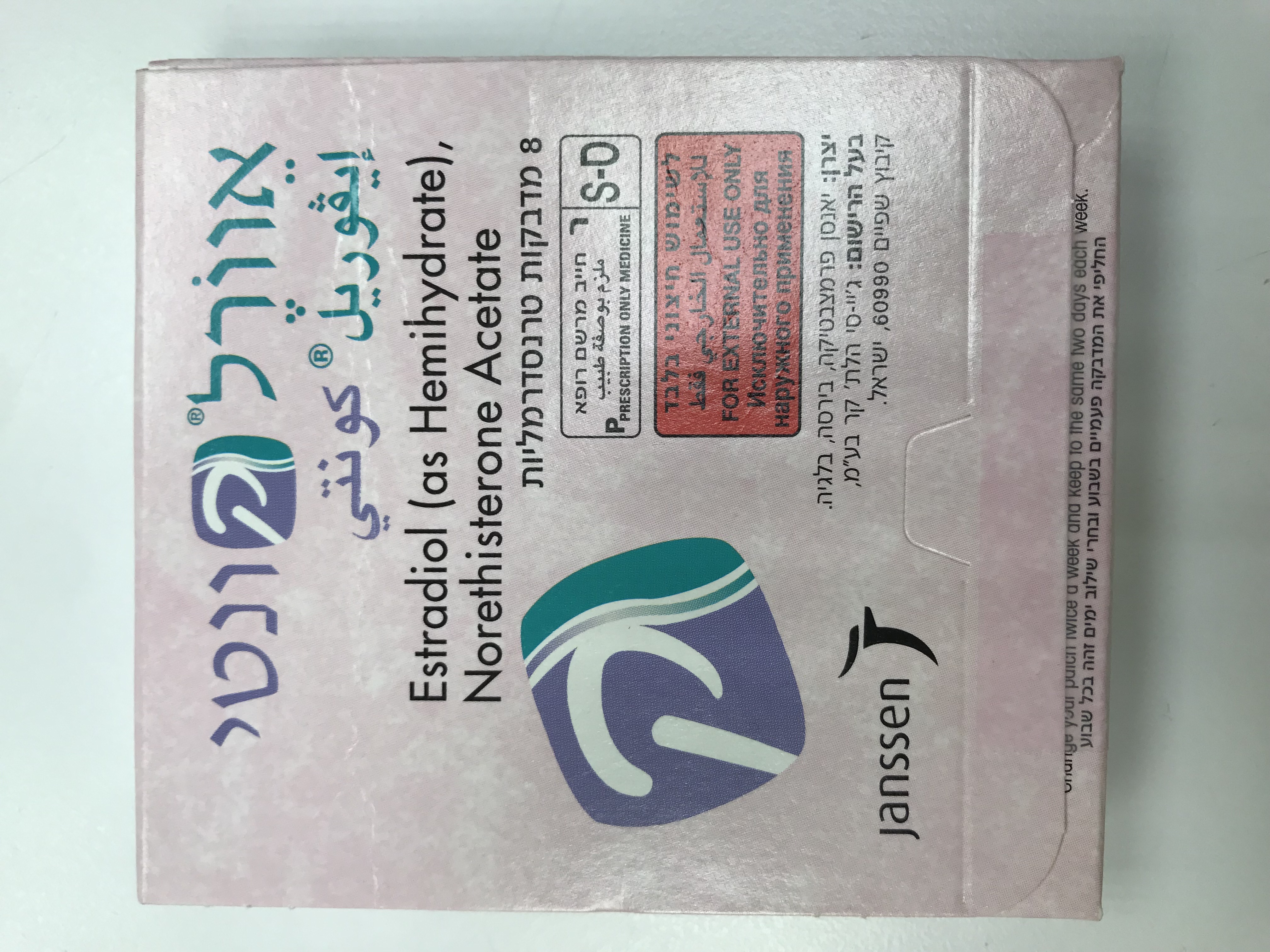
אוורל קונטי EVOREL CONTI (ESTRADIOL AS HEMIHYDRATE, NORETHISTERONE ACETATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
בין-עורי : TRANSDERMAL
צורת מינון:
מדבקות : PATCHES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use For the treatment of menopausal symptoms, HRT should only be initiated for symptoms that adversely affect quality of life. In all cases, a careful appraisal of the risks and benefits should be undertaken at least annually and HRT should only be continued as long as the benefit outweighs the risk. Evidence regarding the risks associated with HRT in the treatment of premature menopause is limited. Due to the low level of absolute risk in younger women, however, the balance of benefits and risks for these women may be more favourable than in older women. Medical examination/follow-up Before initiating or re-instituting HRT, a complete personal and family medical history should be taken. Physical (including pelvic and breast) examination should be guided by this and by the contra-indications and warnings for use. During treatment, periodic check-ups are recommended of a frequency and nature adapted to the individual woman. Women should be advised what changes in their breasts should be reported to their doctor or nurse (see ‘Breast cancer’ below). Investigations, including appropriate imaging tools, e.g. mammography, should be carried out in accordance with currently accepted screening practices, modified to the clinical needs of the individual. Conditions which need supervision If any of the following conditions are present, have occurred previously, and/or have been aggravated during pregnancy or previous hormone treatment, the patient should be closely supervised. It should be taken into account that these conditions may recur or be aggravated during treatment with Evorel Conti, in particular: - Leiomyoma (uterine fibroids) or endometriosis - A history of, or risk factors for, thrombo-embolic disorders (see below) - Risk factors for oestrogen dependent tumours, e.g. 1st degree heredity for breast cancer - Hypertension - Liver disorders (e.g. liver adenoma) - Diabetes mellitus with or without vascular involvement - Cholelithiasis - Migraine or (severe) headache - Systemic lupus erythematosus - A history of endometrial hyperplasia (see below) - Epilepsy - Asthma - Otosclerosis - Mastopathy Conditions which require monitoring while on oestrogen therapy: • Oestrogens may cause fluid retention. Cardiac or renal dysfunction should be carefully observed • Disturbances or mild impairment of liver function • History of cholestatic jaundice • Pre-existing hypertriglyceridaemia. Rare cases of large increases of plasma triglycerides leading to pancreatitis have been reported with oestrogen therapy in this condition Reasons for immediate withdrawal of therapy: Therapy should be discontinued in case a contra-indication is discovered and in the following situations: • Jaundice or deterioration in liver function • Significant increase in blood pressure • New onset of migraine-type headache • Pregnancy Endometrial hyperplasia and carcinoma In women with an intact uterus, the risk of endometrial hyperplasia and carcinoma is increased when oestrogens are administered alone for prolonged periods. The reported increase in endometrial cancer risk among oestrogen-only users, varies from 2 to 12 fold greater compared with non-users, depending on the duration of treatment and oestrogen dose (see Section 4.8). After stopping treatment, the risk may remain elevated for at least 10 years. The addition of a progestogen for 12-14 days per cycle or continuous combined oestrogen/progestogen therapy in non-hysterectomised women prevents the excess risk associated with oestrogen-only HRT. Break-through bleeding and spotting may occur during the first months of treatment. If break-through bleeding or spotting appears after some time on therapy, or continues after treatment has been discontinued, the reason should be investigated, which may include endometrial biopsy to exclude endometrial malignancy. Breast cancer The overall evidence shows an increased risk of breast cancer in women taking combined oestrogen-progestogen or oestrogen-only HRT, that is dependent on the duration of taking HRT. Combined oestrogen-progestogen therapy: The randomised placebo-controlled trial, the Women’s Health Initiative study (WHI), and a meta-analysis of prospective epidemiological studies are consistent in finding an increased risk of breast cancer in women taking combined oestrogen-progestogen for HRT that becomes apparent after about 3 (1-4) years (see Section 4.8). Oestrogen-only therapy: The WHI trial found no increase in the risk of breast cancer in hysterectomised women using oestrogen-only HRT. Observational studies have mostly reported a small increase in risk of having breast cancer diagnosed that is lower than that found in users of oestrogen-progestogen combinations (see Section 4.8). Results from a large meta-analysis showed that after stopping treatment, the excess risk will decrease with time and the time needed to return to baseline depends on the duration of prior HRT use. When HRT was taken for more than 5 years, the risk may persist for 10 years or more. HRT, especially oestrogen-progestogen combined treatment, increases the density of mammographic images which may adversely affect the radiological detection of breast cancer. Ovarian cancer Ovarian cancer is much rarer than breast cancer. Epidemiological evidence from a large meta-analysis suggests a slightly increased risk in women taking oestrogen-only or combined oestrogen-progestogen HRT, which becomes apparent within 5 years of use and diminishes over time after stopping. Some other studies, including the WHI trial, suggest that the use of combined HRTs may be associated with a similar or slightly smaller risk (see Section 4.8). Venous thrombo-embolism HRT is associated with a 1.3-3 fold risk of developing venous thrombo- embolism (VTE), i.e. deep vein thrombosis or pulmonary embolism. The occurrence of such an event is more likely in the first year of HRT than later (See Section 4.8). Generally recognised risk factors for VTE include a personal history or family history, major surgery, prolonged immobilisation, severe obesity (BMI > 30 kg/m2), use of oestrogens, older age, pregnancy/ postpartum period, systemic lupus erythematosus (SLE) and cancer. There is no consensus about the possible role of varicose veins in VTE. Patients with a history of VTE or known thrombophilic states have an increased risk of VTE. HRT may add to this risk, HRT is therefore contraindicated in these patients (see section 4.3). In women with no personal history of VTE but with a first degree relative with a history of thrombosis at young age or recurrent spontaneous abortion, screening may be offered after careful counselling regarding its limitations (only a proportion of thrombophilic defects are identified by screening). If a thrombophilic defect is identified which segregates with thrombosis in family members or if the defect is ‘severe’ (e.g, antithrombin, protein S, or protein C deficiencies or a combination of defects), HRT is contraindicated. The women already on anticoagulant treatment require careful consideration of the benefit-risk of use of HRT. The risk of VTE may be temporarily increased with prolonged immobilisation, major trauma or major surgery. As in all postoperative patients, scrupulous attention should be given to prophylactic measures to prevent VTE following surgery. Where prolonged immobilisation is liable to follow elective surgery, particularly abdominal or orthopaedic surgery to the lower limbs, consideration should be given to temporarily stopping HRT 4 to 6 weeks earlier, if possible. Treatment should not be restarted until the woman is completely mobilised. If VTE develops after initiating therapy, the drug should be discontinued. Patients should be told to contact their doctors immediately when they are aware of a potential thrombo-embolic symptom (eg, painful swelling of a leg, sudden pain in the chest, dyspnoea). Smoking Smoking is a risk factor of VTE. Women should be advised not to smoke if they wish to use Evorel Conti. Coronary artery disease (CAD) There is no evidence from randomised controlled trials of protection against myocardial infarction in women with or without existing CAD who received combined oestrogen-progestogen or oestrogen-only HRT. Oestrogen-only: Randomised controlled data found no increased risk of CAD in hysterectomised women using oestrogen-only therapy. Combined oestrogen-progestogen therapy: The relative risk of CAD during use of combined oestrogen-progestogen HRT is slightly increased. The absolute risk of CAD is strongly dependent on age. The number of extra cases of CAD due to oestrogen-progestogen use is very low in healthy women close to menopause, but will rise with more advanced age. Ischaemic Stroke Combined oestrogen-progestogen and oestrogen-only therapy are associated with an up to 1.5-fold increase in risk of ischaemic stroke. The relative risk does not change with age or time since menopause. However, as the baseline risk of stroke is strongly age-dependent, the overall risk of stroke in women who use HRT will increase with age (see Section 4.8). Hypothyroidism Patients who require thyroid hormone replacement therapy should have their thyroid function monitored regularly while on HRT to ensure that thyroid hormone levels remain in an acceptable range. Angioedema Oestrogens may induce or exacerbate symptoms of angioedema, in particular in women with hereditary angioedema. Other conditions Oestrogens may cause fluid retention, and therefore patients with cardiac or renal dysfunction should be carefully observed. Women with pre-existing hypertriglyceridaemia should be followed closely during oestrogen replacement or hormone replacement therapy, since rare cases of large increases of plasma triglycerides leading to pancreatitis have been reported with oestrogen therapy in this condition. Exogenous estrogens may induce or exacerbate symptoms of hereditary and acquired angioedema. Oestrogens increase thyroid binding globulin (TBG), leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 levels (by column or radio-immunoassay) or T3 levels (by radio- immunoassay). T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Other binding proteins may be elevated in serum, i.e. corticoid binding globulin (CBG), sex-hormone-binding globulin (SHBG) leading to increased circulating corticosteroids and sex steroids, respectively. Free or biological active hormone concentrations are unchanged. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-l-antitrypsin, ceruloplasmin). Dementia HRT use does not improve cognitive function. There is some evidence of increased risk of probable dementia in women who start using continuous combined or oestrogen-only HRT after the age of 65. ALT elevations During clinical trials with patients treated for hepatitis C virus (HCV) infections with the combination regimen ombitasvir/paritaprevir/ritonavir with and without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN) were significantly more frequent in women using ethinylestradiol-containing medicinal products such as CHCs. Additionally, also in patients treated with glecaprevir/pibrentasvir, ALT elevations were observed in women using ethinylestradiol-containing medications such as CHCs. Women using medicinal products containing oestrogens other than ethinylestradiol, such as estradiol, had a rate of ALT elevation similar to those not receiving any oestrogens; however, due to the limited number of women taking these other oestrogens, caution is warranted for co-administration with the combination drug regimen ombitasvir/paritaprevir/ritonavir with or without dasabuvir and also the regimen glecaprevir/pibrentasvir. See section 4.5. Contact sensitisation is known to occur with all topical applications. Although it is extremely rare, women who develop contact sensitisation to any of the components of the patch should be warned that a severe hypersensitivity reaction may occur with continuing exposure to the causative agent. Evorel Conti is not to be used for contraception. Women of child-bearing potential should be advised to use non-hormonal contraceptive methods to avoid pregnancy.
Effects on Driving
4.7 Effects on ability to drive and use machines There are no known data on the effects of Evorel Conti on the ability to drive or use machinery.

שימוש לפי פנקס קופ''ח כללית 1994
Menopausal & post menopausal estrogen replacement therapy
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לרופא
07.08.22 - עלון לרופאעלון מידע לצרכן
01.03.22 - עלון לצרכן אנגלית 07.08.22 - עלון לצרכן עברית 01.03.22 - עלון לצרכן ערבית 19.09.22 - עלון לצרכן אנגלית 19.09.22 - עלון לצרכן עברית 19.09.22 - עלון לצרכן ערבית 23.11.23 - עלון לצרכן עברית 30.11.23 - עלון לצרכן אנגלית 30.11.23 - עלון לצרכן עברית 30.11.23 - עלון לצרכן ערבית 01.12.11 - החמרה לעלון 22.07.15 - החמרה לעלון 09.01.22 - החמרה לעלון 07.08.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אוורל קונטי