Quest for the right Drug
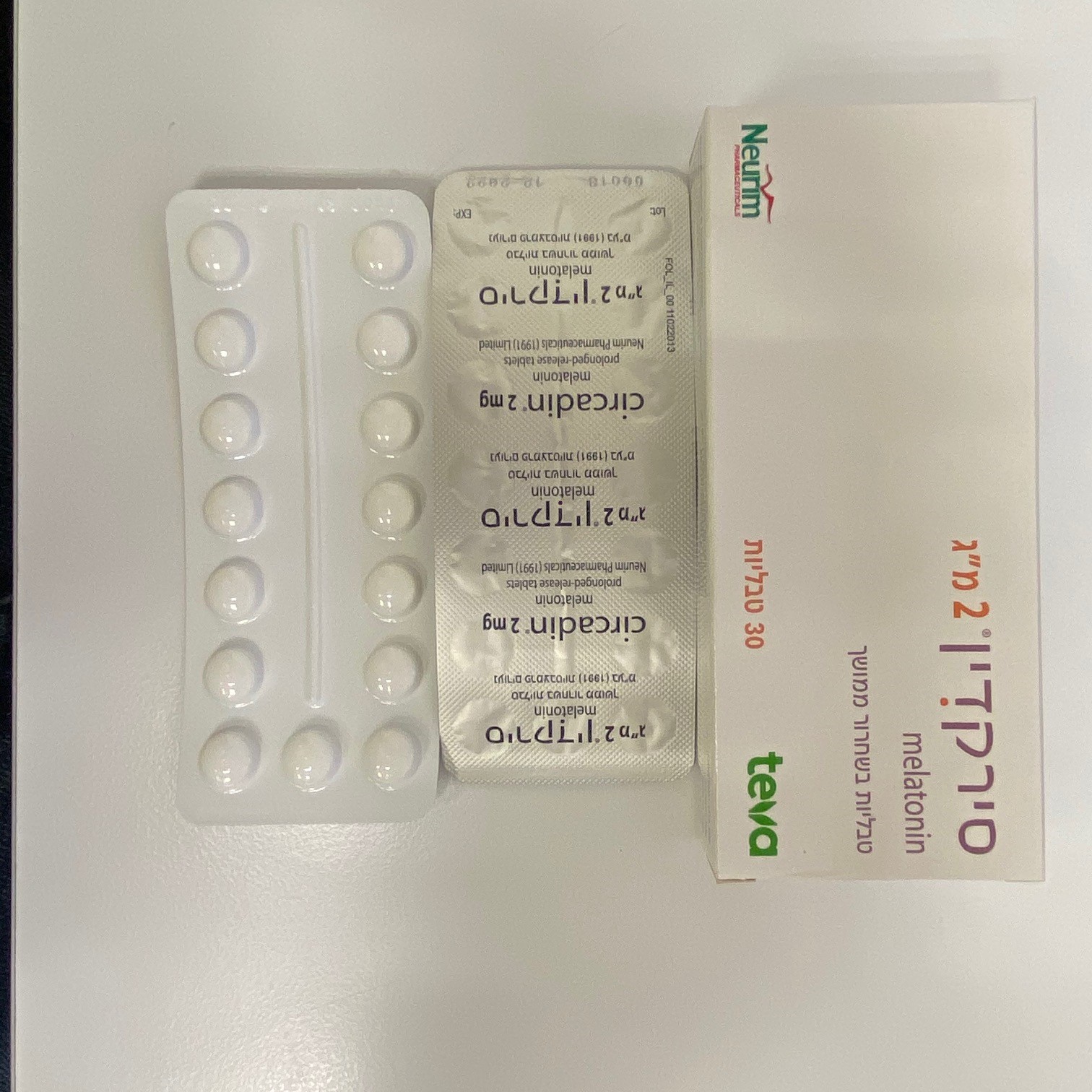
סירקדין CIRCADIN (MELATONIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות בשחרור ממושך : TABLETS PROLONGED RELEASE
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Psycholeptics, melatonin receptor agonists, ATC code: N05CH01 Melatonin is a naturally occurring hormone produced by the pineal gland and is structurally related to serotonin. Physiologically, melatonin secretion increases soon after the onset of darkness, peaks at 2-4 am and diminishes during the second half of the night. Melatonin is associated with the control of circadian rhythms and entrainment to the light-dark cycle. It is also associated with a hypnotic effect and increased propensity for sleep. Mechanism of action The activity of melatonin at the MT1, MT2 and MT3 receptors is believed to contribute to its sleep-promoting properties, as these receptors (mainly MT1 and MT2) are involved in the regulation of circadian rhythms and sleep regulation. Rationale for use Because of the role of melatonin in sleep and circadian rhythm regulation, and the age related decrease in endogenous melatonin production, melatonin may effectively improve sleep quality particularly in patients who are over 55 with primary insomnia. Clinical efficacy and safety In clinical trials, where patients suffering from primary insomnia received Circadin 2 mg every evening for 3 weeks, benefits were shown in treated patients compared to placebo in sleep latency (as measured by objective and subjective means) and in subjective quality of sleep and daytime functioning (restorative sleep) with no impairment of vigilance during the day. In a polysomnographic (PSG) study with a run-in of 2 weeks (single-blind with placebo treatment), followed by a treatment period of 3 weeks (double-blind, placebo-controlled, parallel group design) and a 3-week withdrawal period, sleep latency (SL) was shortened by 9 minutes compared to placebo. There were no modifications of sleep architecture and no effect on REM sleep duration by Circadin. Modifications in diurnal functioning did not occur with Circadin 2 mg. In an outpatient study with 2 week run-in baseline period with placebo, a randomised, double blind, placebo controlled, parallel group treatment period of 3 weeks and 2 week withdrawal period with placebo, the rate of patients who showed a clinically significant improvement in both quality of sleep and morning alertness was 47% in the Circadin group as compared to 27% in the placebo group. In addition, quality of sleep and morning alertness significantly improved with Circadin compared to placebo. Sleep variables gradually returned to baseline with no rebound, no increase in adverse reactions and no increase in withdrawal symptoms. In a second outpatient study with two week run in baseline period with placebo and a randomised, double blind, placebo controlled, parallel group treatment period of 3 weeks, the rate of patients who showed a clinically significant improvement in both quality of sleep and morning alertness was 26% in the Circadin group as compared to 15% in the placebo group. Circadin shortened patients’ reported sleep latency by 24.3 minutes vs 12.9 minutes with placebo. In addition, patients’ self-reported quality of sleep, number of awakenings and morning alertness significantly improved with Circadin compared to placebo. Quality of life was improved significantly with Circadin 2 mg compared to placebo. An additional randomised clinical trial (n=600) compared the effects of Circadin and placebo for up to six months. Patients were re-randomised at 3 weeks. The study demonstrated improvements in sleep latency, quality of sleep and morning alertness, with no withdrawal symptoms and rebound insomnia. The study showed that the benefit observed after 3 weeks is maintained for up to 3 months but failed the primary analysis set at 6 months. At 3 months, about an extra 10% of responders were seen in the Circadin treated group.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption The absorption of orally ingested melatonin is complete in adults and may be decreased by up to 50% in the elderly. The kinetics of melatonin are linear over the range of 2-8 mg. Bioavailability is in the order of 15%. There is a significant first pass effect with an estimated first pass metabolism of 85%. Tmax occurs after 3 hours in a fed state. The rate of melatonin absorption and Cmax following Circadin 2 mg oral administration is affected by food. The presence of food delayed the absorption of the melatonin resulting in a later (T max=3.0 h versus Tmax=0.75 h) and lower peak plasma concentration in the fed state (Cmax=1020pg/ml versus Cmax=1176 pg/ml). Distribution The in vitro plasma protein binding of melatonin is approximately 60%. Circadin is mainly bound to albumin, alpha1-acid glycoprotein and high density lipoprotein. Biotransformation Experimental data suggest that isoenzymes CYP1A1, CYP1A2 and possibly CYP2C19 of the cytochrome P450 system are involved in melatonin metabolism. The principal metabolite is 6-sulphatoxy-melatonin (6-S-MT), which is inactive. The site of biotransformation is the liver. The excretion of the metabolite is completed within 12 hours after ingestion. Elimination Terminal half life (t½) is 3.5-4 hours. Elimination is by renal excretion of metabolites, 89% as sulphated and glucoronide conjugates of 6-hydroxymelatonin and 2% is excreted as melatonin (unchanged active substance). Gender A 3-4-fold increase in Cmax is apparent for women compared to men. A five-fold variability in Cmax between different members of the same sex has also been observed. However, no pharmacodynamic differences between males and females were found despite differences in blood levels. Special populations Older People Melatonin metabolism is known to decline with age. Across a range of doses, higher AUC and Cmax levels have been reported in older patients compared to younger patients, reflecting the lower metabolism of melatonin in the elderly. Cmax levels around 500 pg/ml in adults (18-45) versus 1200 pg/ml in elderly (55-69); AUC levels around 3,000 pg*h/mL in adults versus 5,000 pg*h/mL in the elderly. Renal impairment Company data indicates that there is no accumulation of melatonin after repeated dosing. This finding is compatible with the short half-life of melatonin in humans. The levels assessed in the blood of the patients at 23:00 (2 hours after administration) following 1 and 3 weeks of daily administration were 411.4 ± 56.5 and 432.00 ± 83.2 pg/ml respectively, and are similar to those found in in healthy volunteers following a single dose of Circadin 2 mg. Hepatic impairment The liver is the primary site of melatonin metabolism and therefore, hepatic impairment results in higher endogenous melatonin levels. Plasma melatonin levels in patients with cirrhosis were significantly increased during daylight hours. Patients had a significantly decreased total excretion of 6-sulfatoxymelatonin compared with controls.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
רישום
139 92 31648 12
מחיר
0 ₪
מידע נוסף
