Quest for the right Drug
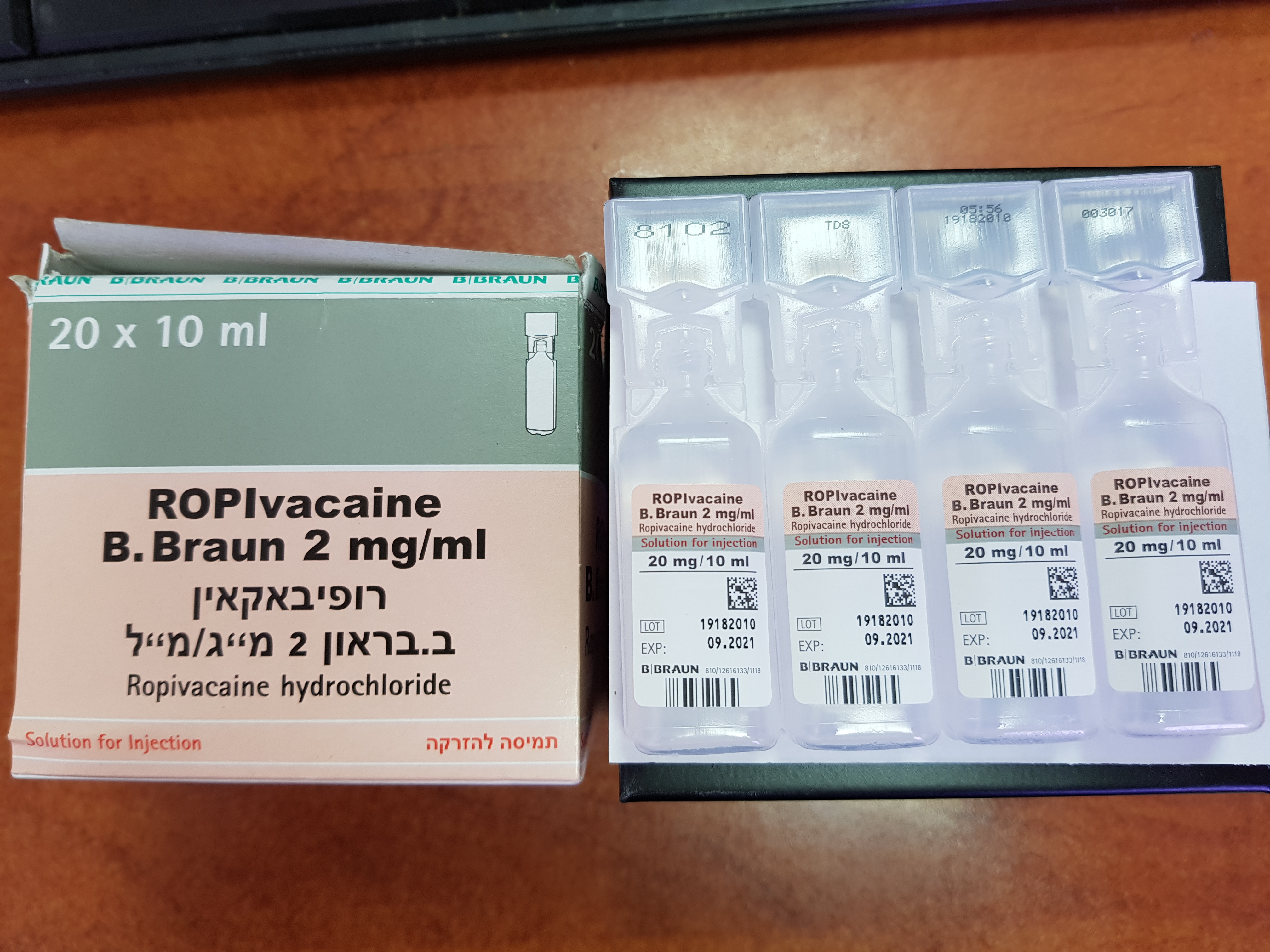
רופיבאקאין ב. בראון 2 מ"ג/ מ"ל ROPIVACAINE B.BRAUN 2 MG/ML (ROPIVACAINE HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
לסביבת העצב, אפידורל : PERINEURAL, EPIDURAL
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Anaesthetics, local, Amides ATC code: N01B B09 Ropivacaine is a long-acting, amide-type local anaesthetic with both anaesthetic and analgesic effects. At high doses ropivacaine produces surgical anaesthesia, while at lower doses it produces sensory block with limited and non-progressive motor block. The mechanism is a reversible reduction of the membrane permeability of the nerve fibre to sodium ions. Consequently the depolarisation velocity is decreased and the excitable threshold increased, resulting in a local blockade of nerve impulses. The most characteristic property of ropivacaine is the long duration of action. Onset and duration of the local anaesthetic efficacy are dependent upon the administration site and dose, but are not influenced by the presence of a vasoconstrictor (e.g. adrenaline (epinephrine)). For details concerning the onset and duration of action of ropivacaine, see table under posology and method of administration. Healthy volunteers exposed to intravenous infusions tolerated ropivacaine well at low doses and with expected CNS symptoms at the maximum tolerated dose. The clinical experience with this drug indicates a good margin of safety when adequately used in recommended doses.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Ropivacaine has a chiral center and is available as the pure S-(-)- enantiomer. It is highly lipid soluble. All metabolites have a local anaesthetic effect but of considerably lower potency and shorter duration than that of ropivacaine. There is no evidence of in vivo racemisation of ropivacaine. The plasma concentration of ropivacaine depends upon the dose, the route of administration and the vascularity of the injection site. Ropivacaine follows linear pharmacokinetics and the Cmax is proportional to the dose. Ropivacaine shows complete and biphasic absorption from the epidural space, with half-lives of the two phases of the order of 14 min and 4 h in adults. The slow absorption is the rate-limiting factor in the elimination of ropivacaine, which explains why the apparent elimination half-life is longer after epidural than after intravenous administration. Distribution Ropivacaine has a mean total plasma clearance in the order of 440 ml/min, a renal clearance of 1 ml/min, a volume of distribution at steady state of 47 liters and a terminal half-life of 1.8 h after i.v. administration. Ropivacaine has an intermediate hepatic extraction ratio of about 0.4. It is mainly bound to α1-acid glycoprotein in plasma with an unbound fraction of about 6%. An increase in total plasma concentrations during continuous epidural and interscalene infusion has been observed, related to a postoperative increase of α1-acid glycoprotein. Variations in unbound, i.e. pharmacologically active, concentration have been much less than in total plasma concentration. Elimination Since ropivacaine has an intermediate to low hepatic extraction ratio, its rate of elimination should depend on the unbound plasma concentration. A postoperative increase in AAG will decrease the unbound fraction due to increased protein binding, which will decrease the total clearance and result in an increase in total plasma concentrations, as seen in the paediatric and adult studies. The unbound clearance of ropivacaine remains unchanged as illustrated by the stable unbound concentrations during postoperative infusion. It is the unbound plasma concentration that is related to systemic pharmacodynamic effects and toxicity. Ropivacaine readily crosses the placenta and equilibrium in regard to unbound concentration will be rapidly reached. The degree of plasma protein binding in the foetus is less than in the mother, which results in lower total plasma concentrations in the foetus than in the mother. Ropivacaine is extensively metabolised, predominantly by aromatic hydroxylation. In total, 86% of the dose is excreted in the urine after intravenous administration, of which only about 1% relates to unchanged drug. The major metabolite is 3-hydroxy-ropivacaine, about 37% of which is excreted in the urine mainly conjugated. Urinary excretion of 4-hydroxy- ropivacaine the N-dealkylated metabolite (PPX) and the 4-hydroxy- dealkylated metabolite accounts for 1-3%. Conjugated and unconjugated 3-hydroxy-ropivacaine shows only detectable concentrations in plasma. Impaired renal function has little or no influence on ropivacaine pharmacokinetics. The renal clearance of PPX is significantly correlated with creatinine clearance. A lack of correlation between total exposure, expressed as AUC, with creatinine clearance indicates that the total clearance of PPX includes a non-renal elimination in addition to renal excretion. Some patients with impaired renal function may show an increased exposure to PPX resulting from a low non-renal clearance. Due to the reduced CNS toxicity of PPX as compared to ropivacaine the clinical consequences are considered negligible in short-term treatment. Patients with end-stage renal disease undergoing dialysis have not been studied.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לרופא
19.12.23 - עלון לרופאעלון מידע לצרכן
לתרופה במאגר משרד הבריאות
רופיבאקאין ב. בראון 2 מ"ג/ מ"ל