Quest for the right Drug
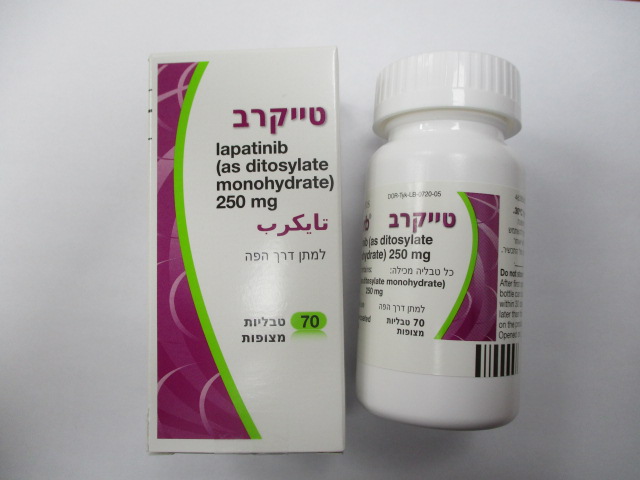
טייקרב TYKERB (LAPATINIB AS DITOSYLATE MONOHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The safety of lapatinib has been evaluated as monotherapy or in combination with other chemotherapies for various cancers in more than 20,000 patients, including 198 patients who received lapatinib in combination with capecitabine and 654 patients who received lapatinib in combination with letrozole (see section 5.1). The most common adverse reactions (>25%) during therapy with lapatinib were gastrointestinal events (such as diarrhoea, nausea, and vomiting) and rash. Palmar-plantar erythrodysesthesia (PPE) was also common (>25%) when lapatinib was administered in combination with capecitabine. The incidence of PPE was similar in the lapatinib plus capecitabine and capecitabine alone treatment arms. Diarrhoea was the most common adverse reaction resulting in discontinuation of treatment when lapatinib was administered in combination with capecitabine, or with letrozole. Tabulated list of adverse reactions The following adverse reactions have been reported to have a causal association with lapatinib alone or lapatinib in combination with capecitabine or letrozole. The following convention has been utilised for the classification of frequency: very common ((≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to <1/1,000) and very rare (<1/10,000), not known (cannot be estimated from the available data). Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness. Immune system disorders Rare Hypersensitivity reactions including anaphylaxis (see section 4.3) Metabolism and nutrition disorders Very common Anorexia Psychiatric disorders Very common Insomnia* TYK API MAR22 V2 EU SmPC Feb22 Nervous system disorders Very common Headache† Common Headache* Cardiac disorders Common Decreased left ventricular ejection fraction (see section 4.2 - dose reduction – cardiac events and section 4.4). Not known Ventricular arrhythmias/Torsades de Pointes, electrocardiogram QT prolonged** Vascular disorders Very common Hot flush† Respiratory, thoracic and mediastinal disorders Very common Epistaxis†, cough†, dyspnoea†. Uncommon Interstitial lung disease/pneumonitis. Not known Pulmonary arterial hypertension**. Gastrointestinal disorders Very common Diarrhoea, which may lead to dehydration (see section 4.2 - dose delay and dose reduction – other toxicities and section 4.4), nausea, vomiting, dyspepsia*, stomatitis*, constipation*, abdominal pain*. Common Constipation† Hepatobiliary disorders Common Hyperbilirubinaemia, hepatotoxicity (see section 4.4). Skin and subcutaneous tissue disorders Very common Rash (including dermatitis acneiform) (see section 4.2 - dose delay and dose reduction – other toxicities), dry skin*†, palmar-plantar erythrodysaesthesia*, alopecia†, pruritus†. Common Nail disorders including paronychia, skin fissures. Notknown Serious cutaneous reactions, including Stevens Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN)** Musculoskeletal and connective tissue disorders Very common Pain in extremity*†, back pain*†, arthralgia†. General disorders and administration site conditions Very common Fatigue, mucosal inflammation*, asthenia†. * These adverse reactions were observed when lapatinib was administered in combination with capecitabine. † These adverse reactions were observed when lapatinib was administered in combination with letrozole. ** Adverse reactions from spontaneous reports and literature Description of selected adverse reactions Decreased left ventricular ejection fraction and QT interval prolongation Left ventricular ejection fraction (LVEF) decreases have been reported in approximately 1% of patients receiving lapatinib and were asymptomatic in more than 70% of cases. LVEF decreases resolved or improved in more than 70 % of cases, in approximately 60 % of these on discontinuation of treatment with lapatinib, and in approximately 40 % of cases lapatinib was continued. Symptomatic LVEF decreases were observed in approximately 0.3% of patients who received lapatinib monotherapy or in combination with other anti-cancer medicinal products. Observed adverse reactions included dyspnoea, cardiac failure and palpitations. Overall 58 % of these symptomatic patients recovered. LVEF decreases were reported in 2.5 % of patients who received lapatinib in combination with capecitabine, as compared to 1.0 % with capecitabine alone. LVEF decreases were reported in 3.1 % of patients who received lapatinib in combination with letrozole as compared to 1.3 % of TYK API MAR22 V2 EU SmPC Feb22 patients receiving letrozole plus placebo. LVEF decreases were reported in 6.7 % of patients who received lapatinib in combination with trastuzumab, as compared to 2.1 % of patients who received lapatinib alone. A concentration dependent increase in QTcF (maximum mean ΔΔQTcF 8.75 ms; 90% CI 4.08, 13.42) was observed in a dedicated QT study in patients with advanced solid tumours (see section 4.4). Diarrhoea Diarrhoea occurred in approximately 65 % of patients who received lapatinib in combination with capecitabine and in 64 % of patients who received lapatinib in combination with letrozole. Most cases of diarrhoea were grade 1 or 2 and did not result in discontinuation of treatment with lapatinib. Diarrhoea responds well to proactive management (see section 4.4). However, a few cases of acute renal failure have been reported secondary to severe dehydration due to diarrhoea. Rash Rash occurred in approximately 28 % of patients who received lapatinib in combination with capecitabine, in 45 % of patients who received lapatinib in combination with letrozole. Rash was generally low grade and did not result in discontinuation of treatment with lapatinib. Prescribing physicians are advised to perform a skin examination prior to treatment and regularly during treatment. Patients experiencing skin reactions should be encouraged to avoid exposure to sunlight and apply broad spectrum sunscreens with a Sun Protection Factor (SPF) ≥ 30. If a skin reaction occurs a full body examination should be performed at every visit until one month after resolution. Patients with extensive or persistent skin reactions should be referred to a dermatologist. Hepatotoxicity The risk of lapatinib-induced hepatotoxicity was associated with carriage of the HLA alleles DQA1*02:01 and DRB1*07:01 (see section 4.4). Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בסרטן שד גרורתי ובהתקיים כל התנאים האלה: (1) התחלת הטיפול תיעשה בהתקיים כל התנאים האלה: (א) המטופל אובחן כסובל מסרטן שד גרורתי; (ב) מצבו התפקודי של המטופל מוגדר כסביר עד טוב (בין 0-2) לפי ה-PS (Performance Score);(ג) קיימת עדות להימצאות HER-2 חיובי ברמה של 3+ בבדיקה אימונוהיסטוכימית (IHC) או בדיקת FISH חיובית כאשר הבדיקה האימונוהיסטוכימית היא ברמה של 2+ (כפי שייקבע בבדיקה כמותית); (ד) החולה חווה התקדמות מחלה לאחר טיפול ב-TRASTUZUMAB למחלתו הגרורתית. (2) המשך הטיפול בתרופה האמורה, לאחר שני חודשי טיפול, יינתן בהתקיים אחד מהתנאים האלה: (א) תגובה של נסיגה מלאה של המחלה (CR); (ב) תגובה של נסיגה חלקית של המחלה (PR); (ג) שיפור קליני בולט (לפחות דרגה אחת ב-PS); (ד) שיפור בסימפטומטולוגיה (כגון הפחתה בכאבי עצמות וצריכה מופחתת של משככי כאבים); (3) על אף האמור בפסקת משנה (2), ייפסק הטיפול בתרופה האמורה לאחר שני חודשי טיפול בהתקיים אחד מאלה: (א) הופעת גרורות חדשות, למעט גרורות במוח כאתר התקדמות יחידי; (ב) החמרת המצב הקליני (שייקבע לפי ירידה בדרגות תפקיד לפי PS); (ג) הופעת גוש חדש, בבדיקה פיסיקלית; (ד) קיום ראיה אחרת להתקדמות המחלה. (4) התרופה לא תינתן בשילוב עם TRASTUZUMAB. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בסרטן שד גרורתי |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
03/01/2010
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
