Quest for the right Drug
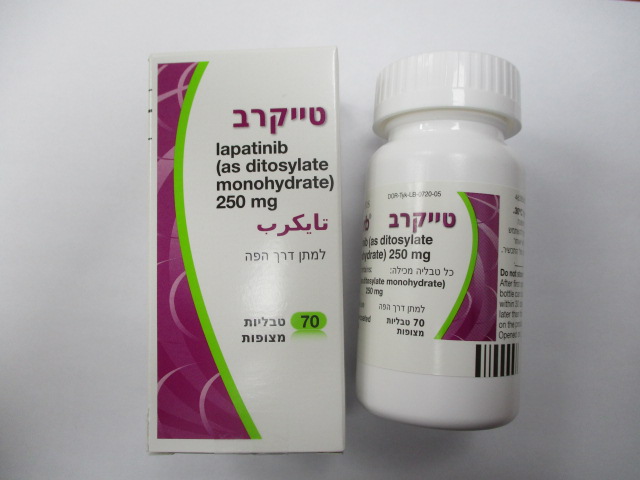
טייקרב TYKERB (LAPATINIB AS DITOSYLATE MONOHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, human epidermal growth factor receptor 2 (HER2) tyrosine kinase inhibitors, ATC code: L01EH01. Mechanism of action Lapatinib, a 4-anilinoquinazoline, is an inhibitor of the intracellular tyrosine kinase domains of both EGFR (ErbB1) and of HER2 (ErbB2) receptors (estimated Kiapp values of 3nM and 13nM, respectively) with a slow off-rate from these receptors (half-life greater than or equal to 300 minutes). Lapatinib inhibits ErbB-driven tumour cell growth in vitro and in various animal models. The growth inhibitory effects of lapatinib were evaluated in trastuzumab-conditioned cell lines. Lapatinib retained significant activity against HER2-amplified breast cancer cell lines selected for long-term growth in trastuzumab-containing medium in vitro. Clinical efficacy and safety Combination treatment with Tykerb and capecitabine The efficacy and safety of Tykerb in combination with capecitabine in breast cancer patients with good performance status was evaluated in a randomised, phase III study. Patients eligible for enrolment had HER2-overexpressing, locally advanced or metastatic breast cancer, progressing after prior treatment that included taxanes, anthracyclines and trastuzumab. LVEF was evaluated in all patients (using echocardiogram [Echo] or multi gated acquisition scan [MUGA]) prior to initiation of treatment with Tykerb to ensure baseline LVEF was within the institutions normal limits. In the clinical study LVEF was monitored at approximately eight week intervals during treatment with Tykerb to ensure it did not decline to below the institutions lower limit of normal. The majority of LVEF decreases (greater than 60 % of events) were observed during the first nine weeks of treatment, however limited data was available for long term exposure. Patients were randomised to receive either Tykerb 1250 mg once daily (continuously) plus capecitabine (2000 mg/m2/day on days 1-14 every 21 days), or to receive capecitabine alone (2500 mg/m2/day on days 1-14 every 21 days). The primary endpoint was time to progression (TTP). Assessments were undertaken by the study investigators and by an independent review panel, blinded to treatment. The study was halted based on the results of a pre-specified interim analysis that showed an improvement in TTP for patients receiving Tykerb plus capecitabine. An additional 75 patients were enrolled in the study between the time of the interim analysis and the end of the enrolment. Investigator analysis on data at the end of enrolment is presented in Table 1. TYK API MAR22 V2 EU SmPC Feb22 Table 1 Time to progression data from Study EGF100151 (Tykerb / capecitabine) Investigator assessment Tykerb (1250 mg/day)+ Capecitabine (2500 capecitabine (2000 mg/m2/day, days 1-14 q21 mg/m2/day, days 1-14 q21 days) days) (N = 198) (N = 201) Number of TTP events 121 126 Median TTP, weeks 23.9 18.3 Hazard Ratio 0.72 (95% CI) (0.56, 0.92) p value 0.008 The independent assessment of the data also demonstrated that Tykerb when given in combination with capecitabine significantly increased time to progression (Hazard Ratio 0.57 [95 % CI 0.43, 0.77] p=0.0001) compared to capecitabine alone. Results of an updated analysis of the overall survival data to 28 September 2007 are presented in Table 2. Table 2 Overall survival data from Study EGF100151 (Tykerb / capecitabine) Tykerb (1250 mg/day)+ Capecitabine (2500 mg/m2/day, capecitabine (2000 mg/m2/day, days 1-14 q21 days) days 1-14 q21 days) (N = 207) (N = 201) Number of subjects who 148 154 died Median overall survival, 74.0 65.9 weeks Hazard Ratio 0.9 (95% CI) (0.71, 1.12) p value 0.3 On the combination arm, there were 4 (2%) progressions in the central nervous system as compared with the 13 (6%) progressions on the capecitabine alone arm. Data are available on the efficacy and safety of Tykerb in combination with capecitabine relative to trastuzumab in combination with capecitabine. A randomised Phase III study (EGF111438) (N=540) compared the effect of the two regimens on the incidence of CNS as site of first relapse in women with HER2 overexpressing metastatic breast cancer. Patients were randomised to either Tykerb 1250 mg once daily (continuously) plus capecitabine (2000 mg/m2/day on days 1-14 every 21 days), or trastuzumab (loading dose of 8mg/kg followed by 6mg/kg q3 weekly infusions) plus capecitabine (2500mg/m2/day, days 1-14, every 21 days). Randomisation was stratified by prior trastuzumab treatment and number of prior treatments for metastatic disease. The study was halted as the interim analysis (N=475) showed a low incidence of CNS events and, superior efficacy of the trastuzumab plus capecitabine arm in terms of progression-free survival and overall survival (see results of final analysis in Table 3). In the Tykerb plus capecitabine arm 8 patients (3.2%) experienced CNS as site of first progression, compared with 12 patients (4.8%) in the trastuzumab plus capecitabine arm. TYK API MAR22 V2 EU SmPC Feb22 Lapatinib effect on CNS metastasis Lapatinib has in terms of objective responses demonstrated modest activity in the treatment of established CNS metastases. In the prevention of CNS metastases in the metastatic and early breast cancer settings the observed activity was limited. TYK API MAR22 V2 EU SmPC Feb22 Table 3 Analyses of investigator-assessed progression-free survival and overall survival Investigator-Assessed PFS Overall Survival Tykerb (1250 Trastuzumab Tykerb (1250 Trastuzumab mg/day) + (loading dose mg/day) + (loading dose capecitabine of 8mg/kg capecitabine of 8mg/kg (2000 followed by (2000 followed by mg/m2/day, 6mg/kg q3 mg/m2/day, 6mg/kg q3 days 1-14 q21 weekly days 1-14 q21 weekly days) infusions) + days) infusions) + capecitabine capecitabine (2500 (2500 mg/m2/day, mg/m2/day, days 1-14 q21 days 1-14 q21 days) days) ITT population N 271 269 271 269 Number (%) with 160 (59) 134 (50) 70 (26) 58 (22) event1 Kaplan-Meier estimate, months a Median (95% CI) 6.6 (5.7, 8.1) 8.0 (6.1, 8.9) 22.7 (19.5, -) 27.3 (23.7, -) Stratified Hazard ratio b HR (95% CI) 1.30 (1.04, 1.64) 1.34 (0.95, 1.90) p-value 0.021 0.095 Subjects who had received prior trastuzumab* N 167 159 167 159 Number (%) with 103 (62) 86 (54) 43 (26) 38 (24) event1 Median (95% CI) 6.6 (5.7, 8.3) 6.1 (5.7, 8.0) 27.3 (22.5, 22.7 (20.1,-) 33.6) HR (95% CI) 1.13 (0.85, 1.50) 1.18 (0.76, 1.83) Subjects who had not received prior trastuzumab* N 104 110 104 110 Number (%) with 57 (55) 48 (44) 27 (26) 20 (18) event1 Median (95% CI) 6.3 (5.6, 8.1) 10.9 (8.3, 15.0) NE2 (14.6, -) NE2 (21.6, -) HR (95% CI) 1.70 (1.15, 2.50) 1.67 (0.94, 2.96) CI = confidence interval a. PFS was defined as the time from randomisation to the earliest date of disease progression or death from any cause, or to the date of censor. b. Pike estimate of the treatment hazard ratio, <1 indicates a lower risk for Tykerb plus capecitabine compared with Trastuzumab plus capecitabine. 1. PFS event is Progressed or Died and OS event is Died due to any cause. 2. NE=median was not reached. * Post hoc analysis Combination treatment with Tykerb and letrozole Tykerb has been studied in combination with letrozole for the treatment of postmenopausal women with hormone receptor-positive (oestrogen receptor [ER] positive and / or TYK API MAR22 V2 EU SmPC Feb22 progesterone receptor [PgR] positive) advanced or metastatic breast cancer. The Phase III study (EGF30008) was randomised, double-blind, and placebo controlled. The study enrolled patients who had not received prior therapy for their metastatic disease. In the HER2-overexpressing population, only 2 patients were enrolled who had received prior trastuzumab, 2 patients had received prior aromatase inhibitor therapy, and approximately half had received tamoxifen. Patients were randomised to letrozole 2.5 mg once daily plus Tykerb 1500 mg once daily or letrozole with placebo. Randomisation was stratified by sites of disease and by time from discontinuation of prior adjuvant anti-oestrogen therapy. HER2 receptor status was retrospectively determined by central laboratory testing. Of all patients randomised to treatment, 219 patients had tumours overexpressing the HER2 receptor, and this was the pre- specified primary population for the analysis of efficacy. There were 952 patients with HER2-negative tumours, and a total of 115 patients whose tumour HER2 status was unconfirmed (no tumour sample, no assay result, or other reason). In patients with HER2-overexpressing MBC, investigator-determined progression-free survival (PFS) was significantly greater with letrozole plus Tykerb compared with letrozole plus placebo. In the HER2-negative population, there was no benefit in PFS when letrozole plus Tykerb was compared with letrozole plus placebo (see Table 4). Table 4 Progression free survival data from Study EGF30008 (Tykerb / letrozole) HER2-overexpressing HER2-negative population population N = 111 N = 108 N = 478 N = 474 Tykerb 1500 Tykerb 1500 mg / day Letrozole 2.5 mg / day Letrozole 2.5 + Letrozole 2.5 mg /day + Letrozole 2.5 mg /day mg /day + placebo mg /day + placebo Median PFS, weeks 35.4 13.0 59.7 58.3 (95% CI) (24.1, 39.4) (12.0, 23.7) (48.6, 69.7) (47.9, 62.0) Hazard ratio 0.71 (0.53, 0.96) 0.90 (0.77, 1.05) P-value 0.019 0.188 Objective response 27.9% 14.8% 32.6% 31.6% rate (ORR) Odds ratio 0.4 (0.2, 0.9) 0.9 (0.7, 1.3) P-value 0.021 0.26 Clinical benefit rate 47.7% 28.7% 58.2% 31.6% (CBR) Odds Ratio 0.4 (0.2, 0.8) 1.0 (0.7, 1.2) P-value 0.003 0.199 CI= confidence interval HER2 overexpression = IHC 3+ and/or FISH positive; HER2 negative = IHC 0, 1+ or 2+ and/or FISH negative Clinical benefit rate was defined as complete plus partial response plus stable disease for ≥6 months. TYK API MAR22 V2 EU SmPC Feb22 At the time of the final PFS analysis (with median follow-up of 2.64 years), the overall survival data were not mature and there was no significant difference between treatment groups in the HER2-positive population; this had not changed with additional follow-up (>7.5 years median follow-up time; Table 5). Table 5 Overall survival (OS) results from study EGF30008 (in the HER2-positive population only) Tykerb 1500 mg / day Letrozole 2.5 mg /day + Letrozole 2.5 mg + placebo /day N = 108 N = 111 Pre-planned OS analysis (conducted at the time of the final PFS analysis, 03 June 2008) Median follow-up (yrs) 2.64 2.64 Deaths (%) 50 (45) 54 (50) Hazard ratio (95% CI), p- a 0.77 (0.52, 1.14); 0.185 valueb Final OS analysis (post-hoc analysis, 07 August 2013) Median follow-up (yrs) 7.78 7.55 Deaths (%) 86 (77) 78 (72) Hazard ratio (95% CI), p- 0.97 (0.07,1.33); 0.848 value Median values from Kaplan-Meier analysis; HR and p-values from Cox regression models adjusting for important prognostic factors. a. Estimate of the treatment hazard ratio, where <1 indicates a lower risk with letrozole 2.5 mg + lapatinib 1500 mg compared with letrozole 2.5 mg + placebo. b. P-value from Cox regression model, stratifying for site of disease and prior anti-adjuvant therapy at screening. Cardiac electrophysiology The effect of lapatinib on the QT-interval was evaluated in a single-blind, placebo-controlled, single sequence (placebo and active treatment) crossover study in patients with advanced solid tumours (EGF114271) (n=58). During the 4-day treatment period, three doses of matching placebo were administered 12 hours apart in the morning and evening on Day 1 and in the morning on Day 2. This was followed by three doses of lapatinib 2000 mg administered in the same way. Measurements, including electrocardiograms (ECGs) and pharmacokinetic samples, were taken at baseline and at the same time points on Day 2 and Day 4. In the evaluable population (n=37), the maximum mean ΔΔQTcF (90% CI) of 8.75 ms (4.08, 13.42) was observed 10 hours after ingestion of the third dose of lapatinib 2000 mg. The ΔΔQTcF exceeded the 5 ms threshold and the upper bound 90% CIs exceeded the 10 ms threshold at multiple time points. The results for the pharmacodynamics population (n=52) were consistent with those from the evaluable population (maximum ΔΔQTcF (90% CI) of 7.91 ms (4.13, 11.68) observed 10 hours after ingestion of the third dose of lapatinib 2000 mg). There is a positive relationship between lapatinib plasma concentrations and ΔΔQTcF. Lapatinib produced a maximum mean concentration of 3920 (3450-4460) ng/ml (geometric mean/95% CI), exceeding the geometric mean Cmax.ss and 95% CI values observed following the approved dosing regimens. An additional increase in peak exposure of lapatinib can be expected when lapatinib is taken repeatedly with food (see sections 4.2 and 5.2) or TYK API MAR22 V2 EU SmPC Feb22 concomitantly with strong CYP3A4 inhibitors. When lapatinib is taken in combination with strong CYP3A4 inhibitors the QTc interval can be expected to be prolonged by 16.1 ms (12.6-20.3 ms) as demonstrated in a model-based prediction (see section 4.4). Food effects on lapatinib exposure The bioavailability and thereby the plasma concentrations of lapatinib are increased by food, in relation to the content and timing of the meal. Dosing of lapatinib one hour after a meal results in approximately 2-3 times higher systemic exposure, compared to dosing one hour before a meal (see sections 4.5 and 5.2).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption The absolute bioavailability following oral administration of lapatinib is unknown, but it is incomplete and variable (approximately 70% coefficient of variation in AUC). Serum concentrations appear after a median lag time of 0.25 hours (range 0 to 1.5 hours). Peak plasma concentrations (Cmax) of lapatinib are achieved approximately 4 hours after administration. Daily dosing of 1250 mg produces steady state geometric mean (coefficient of variation) Cmax values of 2.43 (76%) µg/ml and AUC values of 36.2 (79%) µg*hr/ml. Systemic exposure to lapatinib is increased when administered with food. Lapatinib AUC values were approximately 3- and 4-fold higher (Cmax approximately 2.5 and 3–fold higher) when administered with a low fat (5% fat [500 calories]) or with a high fat (50% fat [1,000 calories]) meal, respectively, as compared with administration in the fasted state. Systemic exposure to lapatinib is also affected by the timing of administration in relation to food intake. Relative to dosing 1 hour before a low fat breakfast, mean AUC values were approximately 2- and 3-fold higher when lapatinib was administered 1 hour after a low fat or high fat meal, respectively. Distribution Lapatinib is highly bound (greater than 99%) to albumin and alpha-1 acid glycoprotein. In vitro studies indicate that lapatinib is a substrate for the transporters BCRP (ABCG1) and p- glycoprotein (ABCB1). Lapatinib has also been shown in vitro to inhibit these efflux transporters, as well as the hepatic uptake transporter OATP 1B1, at clinically relevant concentrations (IC50 values were equal to 2.3 µg/ml). The clinical significance of these effects on the pharmacokinetics of other medicinal products or the pharmacological activity of other anti-cancer medicinal products is not known. Biotransformation Lapatinib undergoes extensive metabolism, primarily by CYP3A4 and CYP3A5, with minor contributions from CYP2C19 and CYP2C8 to a variety of oxidated metabolites, none of which account for more than 14% of the dose recovered in the faeces or 10% of lapatinib concentration in plasma. Lapatinib inhibits CYP3A (Ki 0.6 to 2.3 µg/ml) and CYP2C8 (0.3 µg/ml) in vitro at clinically relevant concentrations. Lapatinib did not significantly inhibit the following enzymes in human liver microsomes: CYP1A2, CYP2C9, CYP2C19, and CYP2D6 or UGT enzymes (in vitro IC50 values were greater than or equal to 6.9 µg/ml). TYK API MAR22 V2 EU SmPC Feb22 Elimination The half-life of lapatinib measured after single doses increases with increasing dose. However, daily dosing of lapatinib results in achievement of steady state within 6 to 7 days, indicating an effective half-life of 24 hours. Lapatinib is predominantly eliminated through metabolism by CYP3A4/5. Biliary excretion may also contribute to the elimination. The primary route of excretion for lapatinib and its metabolites is in faeces. Recovery of unchanged lapatinib in faeces accounts for a median 27% (range 3 to 67%) of an oral dose. Less than 2% of the administered oral dose (as lapatinib and metabolites) excreted in urine. Renal impairment Lapatinib pharmacokinetics have not been specifically studied in patients with renal impairment or in patients undergoing haemodialysis. Available data suggest that no dose adjustment is necessary in patients with mild to moderate renal impairment. Hepatic impairment The pharmacokinetics of lapatinib were examined in patients with moderate (n = 8) or severe (n = 4) hepatic impairment (Child-Pugh scores of 7-9, or greater than 9, respectively) and in 8 healthy control patients. Systemic exposure (AUC) to lapatinib after a single oral 100 mg dose increased approximately 56% and 85% in patients with moderate and severe hepatic impairment, respectively. Administration of lapatinib in patients with hepatic impairment should be undertaken with caution (see sections 4.2 and 4.4).

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בסרטן שד גרורתי ובהתקיים כל התנאים האלה: (1) התחלת הטיפול תיעשה בהתקיים כל התנאים האלה: (א) המטופל אובחן כסובל מסרטן שד גרורתי; (ב) מצבו התפקודי של המטופל מוגדר כסביר עד טוב (בין 0-2) לפי ה-PS (Performance Score);(ג) קיימת עדות להימצאות HER-2 חיובי ברמה של 3+ בבדיקה אימונוהיסטוכימית (IHC) או בדיקת FISH חיובית כאשר הבדיקה האימונוהיסטוכימית היא ברמה של 2+ (כפי שייקבע בבדיקה כמותית); (ד) החולה חווה התקדמות מחלה לאחר טיפול ב-TRASTUZUMAB למחלתו הגרורתית. (2) המשך הטיפול בתרופה האמורה, לאחר שני חודשי טיפול, יינתן בהתקיים אחד מהתנאים האלה: (א) תגובה של נסיגה מלאה של המחלה (CR); (ב) תגובה של נסיגה חלקית של המחלה (PR); (ג) שיפור קליני בולט (לפחות דרגה אחת ב-PS); (ד) שיפור בסימפטומטולוגיה (כגון הפחתה בכאבי עצמות וצריכה מופחתת של משככי כאבים); (3) על אף האמור בפסקת משנה (2), ייפסק הטיפול בתרופה האמורה לאחר שני חודשי טיפול בהתקיים אחד מאלה: (א) הופעת גרורות חדשות, למעט גרורות במוח כאתר התקדמות יחידי; (ב) החמרת המצב הקליני (שייקבע לפי ירידה בדרגות תפקיד לפי PS); (ג) הופעת גוש חדש, בבדיקה פיסיקלית; (ד) קיום ראיה אחרת להתקדמות המחלה. (4) התרופה לא תינתן בשילוב עם TRASTUZUMAB. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בסרטן שד גרורתי |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
03/01/2010
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
