Quest for the right Drug
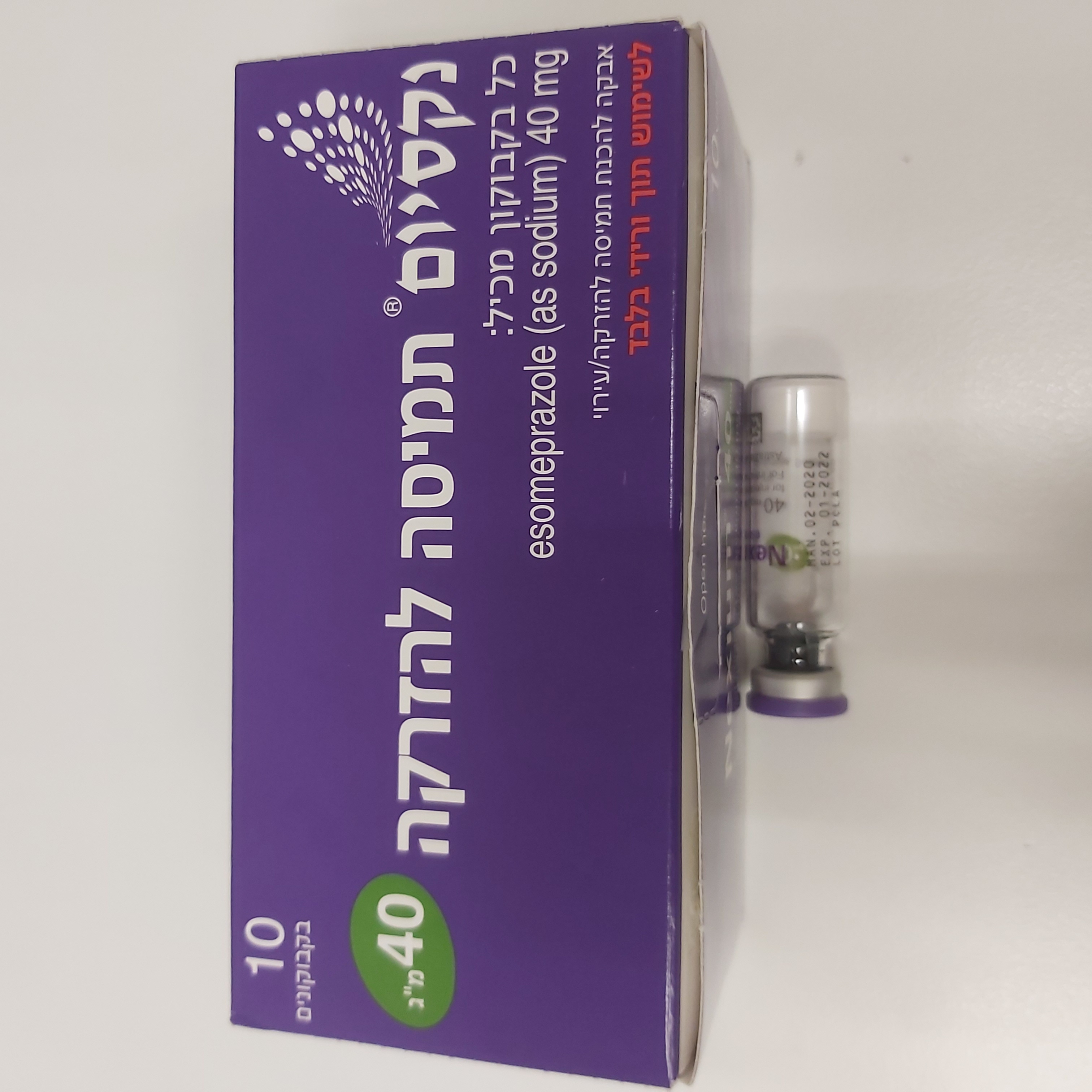
נקסיום אבקה לתמיסה להזרקה/ עירוי 40 מ"ג NEXIUM POWDER FOR SOLUTION FOR INJ/INF 40 MG (ESOMEPRAZOLE AS SODIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להמסה להזרקהאינפוזיה : POWDER FOR SOLUTION FOR INJ/INF
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Proton pump inhibitor. ATC Code: A02B C05 Esomeprazole is the S-isomer of omeprazole and reduces gastric acid secretion through a specific targeted mechanism of action. It is a specific inhibitor of the acid pump in the parietal cell. Both the R- and S-isomer of omeprazole have similar pharmacodynamic activity. Mechanism of action Esomeprazole is a weak base and is concentrated and converted to the active form in the highly acidic environment of the secretory canaliculi of the parietal cell, where it inhibits the enzyme H+K+-ATPase (the acid pump) and inhibits both basal and stimulated acid secretion. Pharmacodynamic effects After 5 days of oral dosing with 20 mg and 40 mg of esomeprazole, intragastric pH above 4 was maintained for a mean time of 13 hours and 17 hours, respectively, over 24 hours in symptomatic GERD patients. The effect is similar irrespective of whether esomeprazole is administered orally or intravenously. Using AUC as a surrogate parameter for plasma concentration, a relationship between inhibition of acid secretion and exposure has been shown, after oral administration of esomeprazole. During intravenous administration of 80 mg esomeprazole as a bolus infusion over 30 minutes followed by a continuous intravenous infusion of 8 mg/hr for 23.5 hours, intragastric pH above 4, and pH above 6 was maintained for a mean time of 21 hours, and 11-13 hours, respectively, over 24 hours in healthy subjects. Healing of reflux esophagitis with esomeprazole 40 mg occurs in approximately 78% of patients after 4 weeks, and 93% after 8 weeks of oral treatment. In a randomized, double blind, placebo-controlled clinical study, patients with endoscopically confirmed peptic ulcer bleeding characterized as Forrest Ia, Ib, IIa or IIb (9%, 43%, 38% and 10% respectively) were randomized to receive NEXIUM® solution for infusion (n=375) or placebo (n=389). Following endoscopic haemostasis, patients received either 80 mg esomeprazole as an intravenous infusion over 30 minutes followed by a continuous infusion of 8 mg per hour or placebo for 72 hours. After the initial 72 hour period, all patients received open-label 40 mg oral NEXIUM® for 27 days for acid suppression. The occurrence of rebleeding within 3 days was 5.9% in the NEXIUM® treated group compared to 10.3% for the placebo group. At 30 days post-treatment, the occurrence of rebleeding in the NEXIUM® treated versus the placebo treated group was and 7.7% vs 13.6%. During treatment with antisecretory drugs serum gastrin increases, in response to the decreased acid secretion. Chromogranin A (CgA) also increases due to decreased gastric acidity. The increased CgA level may interfere with investigations for neuroendocrine tumours. Available published evidence suggests that proton pump inhibitors should be discontinued between 5 days and 2 weeks prior to CgA measurements. This is to allow CgA levels that might be spuriously elevated following PPI treatment to return to reference range. An increased number of ECL cells, possibly related to the increased serum gastrin levels, have been observed in both children and adults during long term treatment with esomeprazole. The findings are considered to be of no clinical significance.4 During long-term oral treatment with antisecretory drugs gastric glandular cysts have been reported to occur at a somewhat increased frequency. These changes are a physiological consequence of pronounced inhibition of acid secretion, are benign, and appear to be reversible. Decreased gastric acidity due to any means including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and in hospitalised patients, possibly also Clostridium difficile. Paediatric population In a placebo-controlled study (98 patients aged 1-11 months) efficacy and safety in patients with signs and symptoms of GERD were evaluated. Esomeprazole 1 mg/kg once daily was given orally for 2 weeks (open-label phase) and 80 patients were included for an additional 4 weeks (doubleblind, treatment-withdrawal phase). There was no significant difference between esomeprazole and placebo for the primary endpoint time to discontinuation due to symptom worsening. In a placebo-controlled study (52 patients aged < 1 month) efficacy and safety in patients with symptoms of GERD were evaluated. Esomeprazole 0.5 mg/kg once daily was given orally for a minimum of 10 days. There was no significant difference between esomeprazole and placebo in the primary endpoint, change from baseline of number of occurrences of symptoms of GERD. Results from the paediatric studies further show that 0.5 mg/kg and 1.0 mg/kg esomeprazole in < 1 month old and 1 to 11-month-old infants, respectively, reduced the mean percentage of time with intra-oesophageal pH < 4. The safety profile appeared to be similar to that seen in adults. In a study in paediatric GERD patients (<1 to 17 years of age) receiving long-term PPI treatment, 61% of the children developed minor degrees of ECL cell hyperplasia with no known clinical significance and with no development of atrophic gastritis or carcinoid tumours.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Distribution The apparent volume of distribution at steady state in healthy subjects is approximately 0.22 L/kg body weight. Esomeprazole is 97% plasma protein bound. Biotransformation Esomeprazole is completely metabolised by the cytochrome P450 system (CYP). The major part of the metabolism of esomeprazole is dependent on the polymorphic CYP2C19, responsible for the formation of the hydroxy- and desmethyl metabolites of esomeprazole. The remaining part is dependent on another specific isoform, CYP3A4, responsible for the formation of esomeprazole sulphone, the main metabolite in plasma. Elimination The parameters below reflect mainly the pharmacokinetics in individuals with a functional CYP2C19 enzyme, extensive metabolisers. Total plasma clearance is about 17 l/h after a single dose and about 9 l/h after repeated administration. The plasma elimination half-life is about 1.3 hours after repeated once daily dosing. Esomeprazole is completely eliminated from plasma between doses with no tendency for accumulation during once daily administration. The major metabolites of esomeprazole have no effect on gastric acid secretion. Almost 80% of an oral dose of esomeprazole is excreted as metabolites in the urine, the remainder in the faeces. Less than 1% of the parent medicinal product is found in urine. Linearity/non-linearity Total exposure (AUC) increases with repeated administration of esomeprazole. This increase is dose-dependent and results in a non-linear dose-AUC relationship after repeated administration. This time- and dose-dependency is due to a decrease of first pass metabolism and systemic clearance probably caused by inhibition of the CYP2C19 enzyme by esomeprazole and/or its sulphone metabolite. Following repeated doses of 40 mg administered as intravenous injections, the mean peak plasma concentration is approx. 13.6 micromol/l. The mean peak plasma concentration after corresponding oral doses is approx. 4.6 micromol/l. A smaller increase (of approx. 30%) can be seen in total exposure after intravenous administration compared to oral administration. There is a dose-linear increase in total exposure following intravenous administration of esomeprazole as a 30-minute infusion (40 mg, 80 mg or 120 mg) followed by a continuous infusion (4 mg/h or 8 mg/h) over 23.5 hours. Special patient population Poor metabolisers Approximately 2.9±1.5% of the population lack a functional CYP2C19 enzyme and are called poor metabolisers. In these individuals the metabolism of esomeprazole is probably mainly catalysed by CYP3A4. After repeated once-daily oral administration of 40 mg esomeprazole, the mean total exposure was approximately 100% higher in poor metabolisers than in subjects with a functional CYP2C19 enzyme (extensive metabolisers). Mean peak plasma concentrations were increased by about 60%. Similar differences have been seen for intravenous administration of esomeprazole. These findings have no implications for the posology of esomeprazole. Gender Following a single oral dose of 40 mg esomeprazole the mean total exposure is approximately 30% higher in females than in males. No gender difference is seen after repeated once-daily administration. Similar differences have been seen for intravenous administration of esomeprazole. These findings have no implications for the posology of esomeprazole. Hepatic impairment The metabolism of esomeprazole in patients with mild to moderate liver impairment may be impaired. The metabolic rate is decreased in patients with severe liver impairment resulting in a doubling of the area under the plasma concentration-time curve of esomeprazole. Therefore, a maximum of 20 mg should not be exceeded in GERD patients with severe impairment. For patients with bleeding ulcers and severe liver impairment, following an initial bolus dose of 80 mg, a maximum continuous intravenous infusion dose of 4 mg/h for 71.5 hours may be sufficient. Esomeprazole or its major metabolites do not show any tendency to accumulate with once-daily dosing. Renal impairment No studies have been performed in patients with decreased renal function. Since the kidney is responsible for the excretion of the metabolites of esomeprazole but not for the elimination of the parent compound, the metabolism of esomeprazole is not expected to be changed in patients with impaired renal function. Elderly The metabolism of esomeprazole is not significantly changed in elderly subjects (71 to 80 years of age). Paediatric population In a randomised, open-label, multi-national, repeated dose study, esomeprazole was given as a once-daily 3-minute injection over four days. The study included a total of 59 paediatric patients 0 to 18 years old of which 50 patients (7 children in the age group 1 to 5 years) completed the study and were evaluated for the pharmacokinetics of esomeprazole. The table below describes the systemic exposure to esomeprazole following the intravenous administration as a 3-minute injection in paediatric patients and adult healthy subjects. The values in the table are geometric means (range). The 20 mg dose for adults was given as a 30-minute infusion. The Css, max was measured 5 minutes post-dose in all paediatric groups and 7 minutes post-dose in adults on the 40 mg dose, and after stop of infusion in adults on the 20 mg dose. Age group Dose group AUC (µmol*h/l) Css,max (µmol/l) 0-1 month* 0.5 mg/kg (n=6) 7.5 (4.5-20.5) 3.7 (2.7-5.8) 1-11 months* 1.0 mg/kg (n=6) 10.5 (4.5-22.2) 8.7 (4.5-14.0) 1-5 years 10 mg (n=7) 7.9 (2.9-16.6) 9.4 (4.4-17.2) 6-11 years 10 mg (n=8) 6.9 (3.5-10.9) 5.6 (3.1-13.2) 20 mg (n=8) 14.4 (7.2-42.3) 8.8 (3.4-29.4) 20 mg (n=6)** 10.1 (7.2-13.7) 8.1 (3.4-29.4) 12-17 years 20 mg (n=6) 8.1 (4.7-15.9) 7.1 (4.8-9.0) 40 mg (n=8) 17.6 (13.1-19.8) 10.5 (7.8-14.2) Adults 20 mg (n=22) 5.1 (1.5-11.8) 3.9 (1.5-6.7) 40 mg (n=41) 12.6 (4.8-21.7) 8.5 (5.4-17.9) * A patient in the age group 0 up to 1 month was defined as a patient with a corrected age of ≥ 32 complete weeks and <44 complete weeks, where corrected age was the sum of the gestational age and the age after birth in complete weeks. A patient in the age group 1 to 11 months had a corrected age of ≥ 44 complete weeks. ** Two patients excluded, 1 most likely a CYP2C19 poor metaboliser and 1 on concomitant treatment with a CYP3A4 inhibitor. Model based predictions indicate that Css,max following intravenous administration of esomeprazole as a 10 minute, 20 minute and 30 minute infusions will be reduced by on average 37% to 49%, 54% to 66% and 61% to 72%, respectively, across all age and dose groups compared to when the dose is administered as a 3 minute injection.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לרופא
19.07.21 - עלון לרופאלתרופה במאגר משרד הבריאות
נקסיום אבקה לתמיסה להזרקה/ עירוי 40 מ"ג