Quest for the right Drug
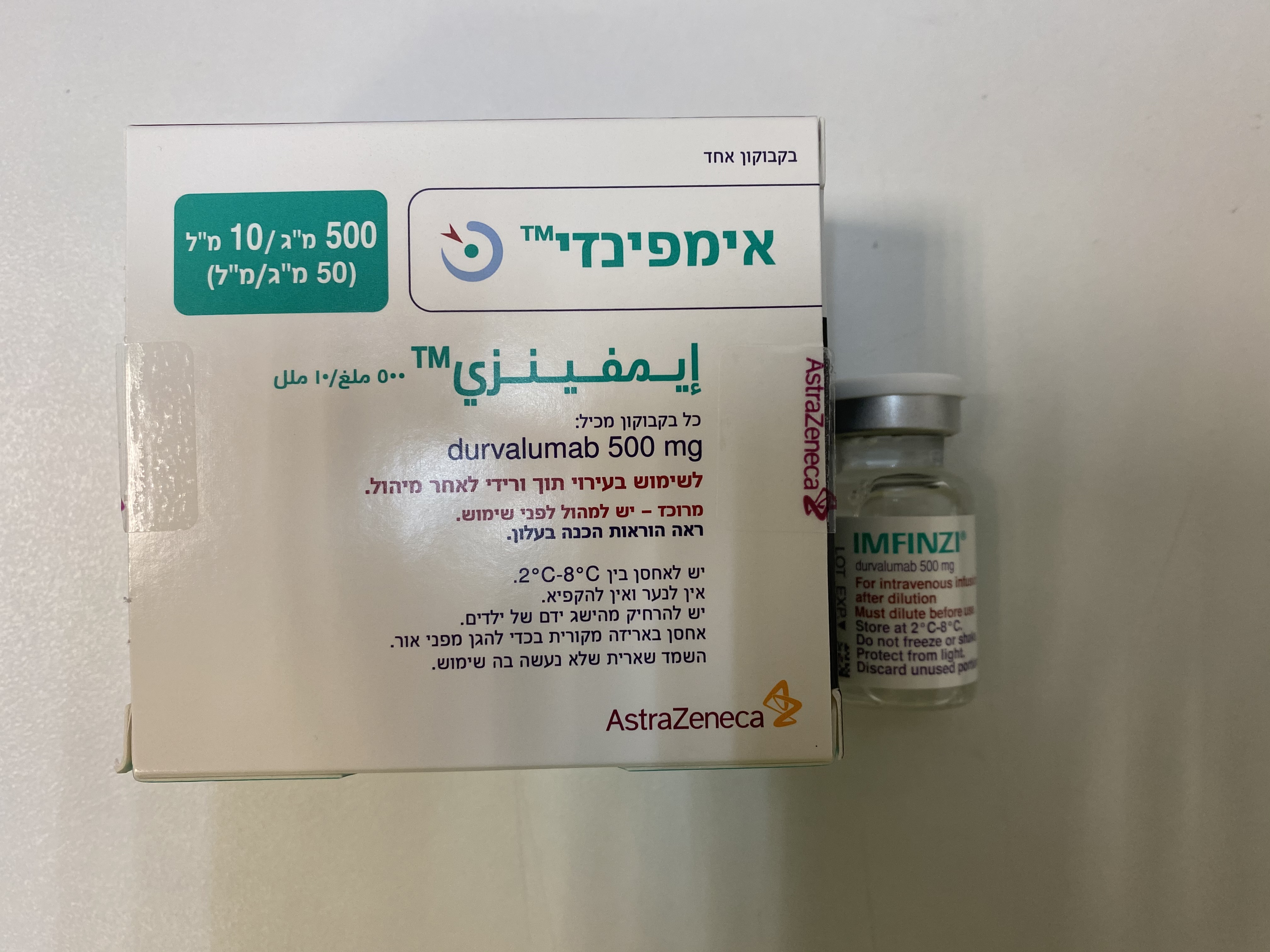
אימפינזי 500 מ"ג/ 10 מ"ל IMFINZI 500 MG/10 ML (DURVALUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה לאינפוזיה : SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
6 ADVERSE REACTIONS The following adverse reactions are discussed in greater detail in other sections of the labeling. • Immune-Mediated Adverse Reactions [see Warnings and Precautions (5.1)]. • Infusion-Related Reactions [see Warnings and Precautions (5.2)]. 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The data described in the Warnings and Precautions section reflect exposure to IMFINZI in 1889 patients from the PACIFIC study (a randomized, placebo-controlled study that enrolled 475 patients with Stage III NSCLC), Study 1108 (an open-label, single-arm, multicohort study that enrolled 191 patients with urothelial carcinoma and 779 patients with other solid tumors), and additional open-label, single-arm trial that enrolled 444 patients with metastatic lung cancer, an indication for which durvalumab is not approved. In these trials, IMFINZI was administered at a dose of 10 mg/kg every 2 weeks. Among the 1889 patients, 38% were exposed for 6 months or more and 18% were exposed for 12 months or more. The data also reflect exposure to IMFINZI in combination with chemotherapy in 265 patients from the CASPIAN study (a randomized, open-label study in patients with ES-SCLC). In the CASPIAN study, IMFINZI was administered at a dose of 1500 mg every 3 or 4 weeks. The data described in this section reflect exposure to IMFINZI in patients with locally advanced or metastatic urothelial carcinoma enrolled in Study 1108, in patients with Stage III NSCLC enrolled in the PACIFIC study and in patients with ES-SCLC enrolled in the CASPIAN study. Urothelial Carcinoma The safety of IMFINZI was evaluated in 182 patients with locally advanced or metastatic urothelial carcinoma in the urothelial carcinoma cohort of Study 1108 whose disease has progressed during or after one standard platinum-based regimen. Patients received 10 mg/kg intravenously every 2 weeks [see Clinical Studies (14.1)]. The median duration of exposure was 2.3 months (range: 1 day to 12.1 months). Thirty-one percent (31%) of patients had a drug delay or interruption for an adverse reaction. The most common (>2%) were liver injury (4.9%), urinary tract infection (3.3%), acute kidney injury (3.3%), and musculoskeletal pain (2.7%). The most common adverse reactions (≥15%) were fatigue (39%), musculoskeletal pain (24%), constipation (21%), decreased appetite (19%), nausea (16%), peripheral edema (15%) and urinary tract infection (15%). The most common Grade 3 or 4 adverse reactions (≥3%) were fatigue, urinary tract infection, musculoskeletal pain, abdominal pain, dehydration, and general physical health deterioration. Eight patients (4.4%) who were treated with IMFINZI experienced Grade 5 adverse events of cardiorespiratory arrest, general physical health deterioration, sepsis, ileus, pneumonitis, or immune- mediated hepatitis. Three additional patients were experiencing infection and disease progression at the time of death. IMFINZI was discontinued for adverse reactions in 3.3% of patients. Serious adverse reactions occurred in 46% of patients. The most frequent serious adverse reactions (>2%) were acute kidney injury (4.9%), urinary tract infection (4.4%), musculoskeletal pain (4.4%), liver injury (3.3%), general physical health deterioration (3.3%), sepsis, abdominal pain, pyrexia/tumor associated fever (2.7% each). Table 3 summarizes the adverse reactions that occurred in ≥10% of patients, while Table 4 summarizes the Grade 3 - 4 laboratory abnormalities that occurred in ≥1% of patients treated with IMFINZI in the urothelial carcinoma cohort of Study 1108. Table 3. Adverse Reactions in ≥10% of Patients in study 1108 Urothelial Carcinoma Cohort IMFINZI (N=182) Adverse Reaction All Grades Grades 3 – 4 (%) (%) Gastrointestinal Disorders Constipation 21 1.1 Nausea 16 1.6 Abdominal pain1 14 2.7 Diarrhea/Colitis 13 1.1 General Disorders and Administration Fatigue2 39 6 Peripheral edema3 15 1.6 Pyrexia/Tumor associated fever 14 0.5 Infections Urinary tract infection4 15 4.4 Metabolism and Nutrition Disorders Decreased appetite/Hypophagia 19 0.5 Musculoskeletal and Connective Tissue Disorders Musculoskeletal pain5 24 3.8 Respiratory, Thoracic, and Mediastinal Disorders Dyspnea/Exertional Dyspnea 13 2.2 Cough/Productive Cough 10 0 Skin and Subcutaneous Tissue Disorders Rash6 11 0.5 1 Includes abdominal pain upper, abdominal pain lower and flank pain Includes asthenia, lethargy, and malaise 2 Includes edema, localized edema, edema peripheral, lymphedema, peripheral swelling, scrotal edema, and scrotal swelling 3 Includes cystitis, candiduria and urosepsis 5 Includes back pain, musculoskeletal chest pain, musculoskeletal pain and discomfort, myalgia, and neck pain 6 Includes dermatitis, dermatitis acneiform, dermatitis psoriasiform, psoriasis, rash maculo-papular, rash pruritic, rash papular, rash pustular, skin toxicity, eczema, erythema, erythema multiforme, rash erythematous, acne, and lichen planus Table 4. Grade 3-4 Laboratory Abnormalities Worsened from Baseline Occurring in ≥1% Patients in Study 1108 Urothelial Carcinoma Cohort Laboratory Abnormality Grade 3 – 4 % Hyponatremia 12 Lymphopenia 11 Anemia 8 Increased alkaline phosphatase 4.1 Hypermagnesemia 4.2 Hypercalcemia 3 Hyperglycemia 3 Increased AST 2.4 Increased ALT 0.6 Hyperbilirubinemia 1.2 Increased creatinine 1.2 Neutropenia 1.2 Hyperkalemia 1.2 Hypokalemia 1.2 Hypoalbuminemia 1.2 Non-Small Cell Lung Cancer The safety of IMFINZI in patients with Stage III NSCLC who completed concurrent platinum-based chemoradiotherapy within 42 days prior to initiation of study drug was evaluated in the PACIFIC study, a multicenter, randomized, double-blind, placebo-controlled study. A total of 475 patients received IMFINZI 10 mg/kg intravenously every 2 weeks. The study excluded patients who had disease progression following chemoradiation, with active or prior autoimmune disease within 2 years of initiation of the study or with medical conditions that required systemic immunosuppression. [see Clinical Studies (14.2)]. The study population characteristics were: median age of 64 years (range: 23 to 90), 45% age 65 years or older, 70% male, 69% White, 27% Asian, 75% former smoker, 16% current smoker, and 51% had WHO performance status of 1. All patients received definitive radiotherapy as per protocol, of which 92% received a total radiation dose of 54 Gy to 66 Gy. The median duration of exposure to IMFINZI was 10 months (range: 0.2 to 12.6). IMFINZI was discontinued due to adverse reactions in 15% of patients. The most common adverse reactions leading to IMFINZI discontinuation were pneumonitis or radiation pneumonitis in 6% of patients. Serious adverse reactions occurred in 29% of patients receiving IMFINZI. The most frequent serious adverse reactions reported in at least 2% of patients were pneumonitis or radiation pneumonitis (7%) and pneumonia (6%). Fatal pneumonitis or radiation pneumonitis and fatal pneumonia occurred in < 2% of patients and were similar across arms. The most common adverse reactions (occurring in ≥ 20% of patients) were cough, fatigue, pneumonitis or radiation pneumonitis, upper respiratory tract infections, dyspnea and rash. Table 5 summarizes the adverse reactions that occurred in at least 10% of patients treated with IMFINZI. Table 5. Adverse Reactions Occurring in ≥ 10% Patients in the PACIFIC Study IMFINZI N=475 Placebo1 N=234 Adverse Reaction All Grades Grades 3-4 (%) All Grades (%) Grades (%) 3-4 (%) Respiratory, Thoracic and Mediastinal Disorders Cough/Productive Cough 40 0.6 30 0.4 Pneumonitis2/Radiation Pneumonitis 34 3.4 25 3 Dyspnea3 25 1.5 25 2.6 Gastrointestinal Disorders Diarrhea 18 0.6 19 1.3 Abdominal pain4 10 0.4 6 0.4 Endocrine Disorders Hypothyroidism5 12 0.2 1.7 0 Skin and Subcutaneous Tissue Disorders Rash6 23 0.6 12 0 Pruritus7 12 0 6 0 General Disorders Fatigue8 34 0.8 32 1.3 Pyrexia 15 0.2 9 0 Infections Upper respiratory tract 26 0.4 19 0 infections9 Pneumonia10 17 7 12 6 1The PACIFIC study was not designed to demonstrate statistically significant difference in adverse reaction rates for IMFINZI, as compared to placebo, for any specific adverse reaction listed in Table 2 includes acute interstitial pneumonitis, interstitial lung disease, pneumonitis, pulmonary fibrosis 3 includes dyspnea and exertional dyspnea 4 includes abdominal pain, abdominal pain lower, abdominal pain upper, and flank pain 5 includes autoimmune hypothyroidism and hypothyroidism 6 includes rash erythematous, rash generalized, rash macular, rash maculopapular, rash papular, rash pruritic, rash pustular, erythema, eczema, rash and dermatitis 7 includes pruritus generalized and pruritus 8 includes asthenia and fatigue 9 includes laryngitis, nasopharyngitis, peritonsillar abscess, pharyngitis, rhinitis, sinusitis, tonsillitis, tracheobronchitis, and upper respiratory tract infection 10 includes lung infection, pneumocystis jirovecii pneumonia, pneumonia, pneumonia adenoviral, pneumonia bacterial, pneumonia cytomegaloviral, pneumonia haemophilus, pneumonia klebsiella, pneumonia necrotising, pneumonia pneumococcal, and pneumonia streptococcal Other adverse reactions occurring in less than 10% of patients treated with IMFINZI were dysphonia, dysuria, night sweats, peripheral edema, and increased susceptibility to infections. Table 6 summarizes the laboratory abnormalities that occurred in at least 20% of patients treated with IMFINZI. Table 6. Laboratory Abnormalities Worsening From Baseline Occurring in ≥ 20% of Patients in the PACIFIC Study IMFINZI Placeb o Laboratory Abnormality Grade 3 or Grade 3 or All All 4 (%) 4 (%) Grades1 Grades1 (%)2 (%)2 Chemistry Hyperglycemia 52 8 51 8 Hypocalcemia 46 0.2 41 0 Increased ALT 39 2.3 22 0.4 Increased AST 36 2.8 21 0.4 Hyponatremia 33 3.6 30 3.1 Hyperkalemia 32 1.1 29 1.8 Increased GGT 24 3.4 22 1.7 Hematology Lymphopenia 43 17 39 18 1 Graded according to NCI CTCAE version 4.0 2 Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: IMFINZI (range: 464 to 470) and placebo (range: 224 to 228) Small Cell Lung Cancer The safety of IMFINZI in combination with etoposide and either carboplatin or cisplatin in previously untreated ES-SCLC was evaluated in CASPIAN, a randomized, open-label, multicenter, active-controlled trial. A total of 265 patients received IMFINZI 1500 mg in combination with chemotherapy every 3 weeks for 4 cycles followed by IMFINZI 1500 mg every 4 weeks until disease progression or unacceptable toxicity. The trial excluded patients with active or prior autoimmune disease or with medical conditions that required systemic corticosteroids or immunosuppressants [see Clinical Studies (14.3)]. Among 265 patients receiving IMFINZI, 49% were exposed for 6 months or longer and 19% were exposed for 12 months or longer. Among 266 patients receiving chemotherapy alone, 57% of the patients received 6 cycles of chemotherapy and 8% of the patients received PCI after chemotherapy. IMFINZI was discontinued due to adverse reactions in 7% of the patients receiving IMFINZI plus chemotherapy. These include pneumonitis, hepatotoxicity, neurotoxicity, sepsis, diabetic ketoacidosis and pancytopenia (1 patient each). Serious adverse reactions occurred in 31% of patients receiving IMFINZI plus chemotherapy. The most frequent serious adverse reactions reported in at least 1% of patients were febrile neutropenia (4.5%), pneumonia (2.3%), anemia (1.9%), pancytopenia (1.5%), pneumonitis (1.1%) and COPD (1.1%). Fatal adverse reactions occurred in 4.9% of patients receiving IMFINZI plus chemotherapy. These include pancytopenia, sepsis, septic shock, pulmonary artery thrombosis, pulmonary embolism, and hepatitis (1 patient each) and sudden death (2 patients). The most common adverse reactions (occurring in ≥ 20% of patients) were nausea, fatigue/asthenia and alopecia. Table 7 summarizes the adverse reactions that occurred in patients treated with IMFINZI plus chemotherapy. Table 7. Adverse Reactions Occurring in ≥ 10% Patients in the CASPIAN study IMFINZI with etoposide and Etoposide and either either carboplatin or cisplatin carboplatin or cisplatin N = N = 265 266 Adverse Reaction All Grades (%) Grade 3-4 (%) All Grades (%) Grade 3-4 (%) Respiratory, thoracic and mediastinal disorders Cough/Productive 15 0.8 9 0 Cough Gastrointestinal disorders Nausea 34 0.4 34 1.9 Constipation 17 0.8 19 0 Vomiting 15 0 17 1.1 Diarrhea 10 1.1 11 1.1 Endocrine disorders Hyperthyroidisma 10 0 0.4 0 Skin and subcutaneous tissue disorders Alopecia 31 1.1 34 0.8 Rashb 11 0 6 0 General disorders and administration site conditions Fatigue/Asthenia 32 3.4 32 2.3 Metabolism and nutrition disorders Decreased appetite 18 0.8 17 0.8 a Includes hyperthyroidism and Basedow's disease b Includes rash erythematous, rash generalized, rash macular, rash maculopapular, rash papular, rash pruritic, rash pustular, erythema, eczema, rash and dermatitis Table 8 summarizes the laboratory abnormalities that occurred in at least 20% of patients treated with IMFINZI plus chemotherapy. Table 8. Laboratory Abnormalities Worsening from Baseline Occurring in ≥ 20%1 of Patients in the CASPIAN study IMFINZI with Etoposide and Etoposide and either either Carboplatin Carboplatin or or Cisplatin Cisplatin Laboratory Abnormality Grade2 3 or 4 (%)3 Grade2 3 or 4 (%)3 Chemistry Hyponatremia 11 13 Hypomagnesemia 11 6 Hyperglycemia 5 5 Increased Alkaline Phosphatase 4.9 3.5 Increased ALT 4.9 2.7 Increased AST 4.6 1.2 Hypocalcemia 3.5 2.4 Blood creatinine increased 3.4 1.1 Hyperkalemia 1.5 3.1 TSH decreased < LLN4 and ≥ LLN at NA NA baseline Hematology Neutropenia 41 48 Lymphopenia 14 13 Anemia 13 22 Thrombocytopenia 12 15 1 The frequency cut off is based on any grade change from baseline 2 Graded according to NCI CTCAE version 4.03 3 Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: IMFINZI (range: 258 to 263) and chemotherapy (range: 253 to 262) except magnesium IMFINZI + chemotherapy(18) and chemotherapy(16) 4 LLN = lower limit of normal 6.2 Immunogenicity As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to durvalumab to the incidence of antibodies to other products may be misleading. Of 2280 patients who received IMFINZI 10 mg/kg every 2 weeks a or 20 mg/kg every 4 weeks as a single-agent, 69 patients (3%) tested positive for treatment-emergent anti-drug antibodies (ADA), and 12 (0.5%) tested positive for neutralizing antibodies. The development of ADA against durvalumab appears to have no clinically relevant effect on its pharmacokinetics or safety. Of 201 patients in the CASPIAN study who received IMFINZI 1500 mg every 3 weeks in combination with chemotherapy for four doses followed by IMFINZI 1500 mg every 4 weeks no patients tested positive for treatment-emergent ADA. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il 8. USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Risk summary Based on its mechanism of action and data from animal studies, IMFINZI can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no data on the use of IMFINZI in pregnant women. In animal reproduction studies, administration of durvalumab to pregnant cynomolgus monkeys from the confirmation of pregnancy through delivery resulted in an increase in premature delivery, fetal loss and premature neonatal death (see Data). Human immunoglobulin G1 (IgG1) is known to cross the placental barrier; therefore, durvalumab has the potential to be transmitted from the mother to the developing fetus. Apprise pregnant women of the potential risk to a fetus. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. Data Animal Data As reported in the literature, the PD-1/PD-L1 pathway plays a central role in preserving pregnancy by maintaining maternal immune tolerance to the fetus. In mouse allogeneic pregnancy models, disruption of PD-L1 signaling was shown to result in an increase in fetal loss. The effects of durvalumab on prenatal and postnatal development were evaluated in reproduction studies in cynomolgus monkeys. Durvalumab was administered from the confirmation of pregnancy through delivery at exposure levels approximately 6 to 20 times higher than those observed at the recommended clinical dose of 10 mg/kg (based on AUC). Administration of durvalumab resulted in premature delivery, fetal loss (abortion and stillbirth) and increase in neonatal deaths. Durvalumab was detected in infant serum on postpartum Day 1, indicating the presence of placental transfer of durvalumab. Based on its mechanism of action, fetal exposure to durvalumab may increase the risk of developing immune-mediated disorders or altering the normal immune response and immune-mediated disorders have been reported in PD-1 knockout mice. 8.2 Lactation Risk Summary There is no information regarding the presence of durvalumab in human milk, the effects on the breastfed infant, or the effects on milk production. Human IgG1 is excreted in human milk. Durvalumab was present in the milk of lactating cynomolgus monkeys and was associated with premature neonatal death (see Data). Because of the potential for adverse reactions in breastfed infants, advise women not to breastfeed during treatment with IMFINZI and for at least 3 months after the last dose. Data In lactating cynomolgus monkeys, durvalumab was present in breast milk at about 0.15% of maternal serum concentrations after administration of durvalumab from the confirmation of pregnancy through delivery at exposure levels approximately 6 to 20 times higher than those observed at the recommended clinical dose of 10 mg/kg (based on AUC). Administration of durvalumab resulted in premature neonatal death. 8.3 Females and Males of Reproductive Potential Contraception Females Based on its mechanism of action and data from animal studies, IMFINZI can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with IMFINZI, and for at least 3 months following the last dose of IMFINZI. 8.4 Pediatric Use The safety and effectiveness of IMFINZI have not been established in pediatric patients. 8.5 Geriatric Use Of the 476 patients treated with IMFINZI in the PACIFIC study, 45% were 65 years or older, while 7.6% were 75 years or older. No overall differences in safety or effectiveness were observed between patients 65 years or older and younger patients. The PACIFIC study did not include sufficient numbers of patients aged 75 years and over to determine whether they respond differently from younger patients. Of the 265 patients with ES-SCLC treated with IMFINZI in combination with chemotherapy, 101 (38%) patients were 65 years or older and 19 (7.2%) patients were 75 years or older. There were no clinically meaningful differences in safety or efficacy between patients 65 years or older and younger patients.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. כמונותרפיה לטיפול בסרטן מתקדם מקומי או גרורתי של דרכי השתן בחולה עם PDL1 גבוה (TC > 25%) והעונה על אחד מאלה: א. מחלתו התקדמה לאחר שקיבל טיפול כימותרפי קודם במשטר שכלל תרכובת פלטינום למחלתו הגרורתית;ב. מחלתו התקדמה בתוך 12 חודשים מטיפול כימותרפי במשטר שכלל תרכובת פלטינום במסגרת משלימה (adjuvant) או noeoadjuvant. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת ה-Checkpoint inhibitors2. כמונותרפיה בסרטן ריאה מסוג NSCLC שלב III לא נתיח, בחולים שמחלתם לא התקדמה לאחר טיפול משולב בכימותרפיה מבוססת פלטינום והקרנות.משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה.במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת ה-Checkpoint inhibitors.לעניין זה סרטן ריאה מסוג NSCLC שלב III לא נתיח לא מוגדר כאותה מחלה כמו סרטן ריאה מסוג NSCLC בשלב IV. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או מומחה באורולוגיה המטפל באורולוגיה אונקולוגית.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מונותרפיה לטיפול בסרטן מתקדם מקומי או גרורתי של דרכי השתן בחולה עם PDL1 גבוה (TC > 25%) והעונה על אחד מאלה: א. מחלתו התקדמה לאחר שקיבל טיפול כימותרפי קודם במשטר שכלל תרכובת פלטינום למחלתו הגרורתית; ב. מחלתו התקדמה בתוך 12 חודשים מטיפול כימותרפי במשטר שכלל תרכובת פלטינום במסגרת משלימה (adjuvant) או noeoadjuvant. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת ה-Checkpoint inhibitors | 03/02/2022 | אונקולוגיה | Urothelial cancer, סרטן מתקדם בדרכי השתן | |
| סרטן ריאה מסוג NSCLC שלב III לא נתיח, בחולים שמחלתם לא התקדמה לאחר טיפול משולב בכימותרפיה והקרנות. משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת ה-Checkpoint inhibitors. לעניין זה סרטן ריאה מסוג NSCLC שלב III לא נתיח לא מוגדר כאותה מחלה כמו סרטן ריאה מסוג NSCLC בשלב IV. | 16/01/2019 | אונקולוגיה | סרטן ריאה מתקדם, Non small cell lung cancer | |
| התרופה תינתן כמונותרפיה לטיפול בסרטן מתקדם מקומי או גרורתי של דרכי השתן בחולה עם PDL1 גבוה (TC > 25%) והעונה על אחד מאלה: 1. קיבל טיפול כימותרפי קודם במשטר שכלל תרכובת פלטינום למחלתו הגרורתית; 2. מחלתו התקדמה בתוך 12 חודשים מטיפול כימותרפי במשטר שכלל תרכובת פלטינום במסגרת משלימה (adjuvant) או noeoadjuvant. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת ה-Checkpoint inhibitors | 11/01/2018 | אונקולוגיה | Urothelial cancer, סרטן מתקדם בדרכי השתן |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
11/01/2018
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
