Quest for the right Drug
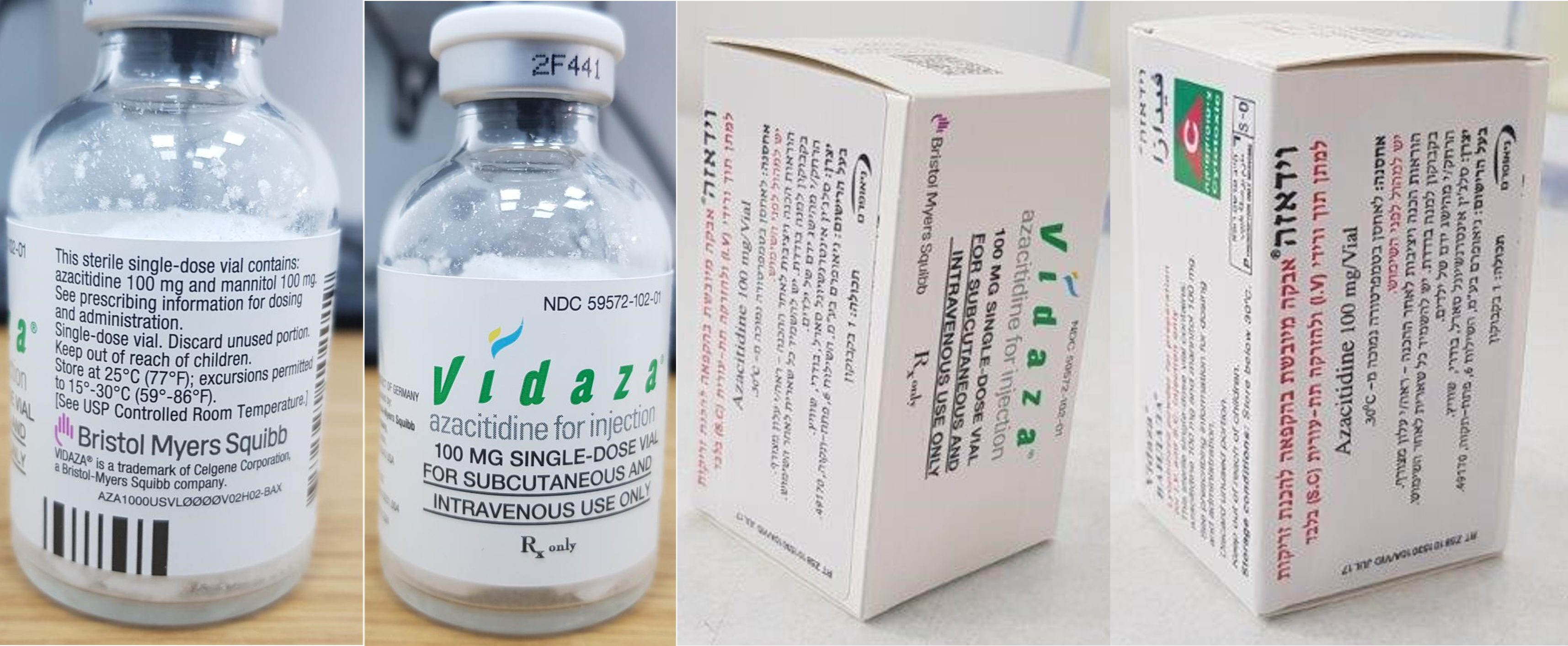
וידאזה VIDAZA (AZACITIDINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי, תת-עורי : I.V, S.C
צורת מינון:
אין פרטים : LYOPHILIZED POWDER FOR SUSPENSION FOR SC INJECTION / SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
6. ADVERSE REACTIONS The following adverse reactions are described in other labeling sections: • Anemia, Neutropenia and Thrombocytopenia [see Warnings and Precautions (5.2)] • Hepatotoxicity in Patients with Severe Pre-existing Hepatic Impairment [see Warnings and Precautions (5.3)] • Renal Toxicity [see Warnings and Precautions (5.4)] • Tumor Lysis Syndrome [see Warnings and Precautions (5.5)] 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. MDS The data described below reflect exposure to VIDAZA in 443 patients with MDS from 4 clinical studies. Study 1 was a supportive-care controlled trial (subcutaneous administration), Studies 2 and 3 were single arm studies (one with subcutaneous administration and one with intravenous administration), and Study 4 was an international randomized trial (subcutaneous administration) [see Clinical Studies (12)]. In Studies 1, 2 and 3, a total of 268 patients were exposed to VIDAZA, including 116 exposed for 6 cycles (approximately 6 months) or more and 60 exposed for greater than 12 cycles (approximately one year). VIDAZA was studied primarily in supportive-care controlled and uncontrolled trials (n=150 and n=118, respectively). The population in the subcutaneous studies (n=220) was 23 to 92 years old (mean 66.4 years), 68% male, and 94% white, and had MDS or AML. The population in the intravenous study (n=48) was 35 to 81 years old (mean 63.1 years), 65% male, and 100% white. Most patients received average daily doses between 50 and 100 mg/m2. In Study 4, a total of 175 patients with higher-risk MDS (primarily RAEB and RAEB-T subtypes) were exposed to VIDAZA. Of these patients, 119 were exposed for 6 or more cycles, and 63 for at least 12 cycles. The mean age of this population was 68.1 years (ranging from 42 to 83 years), 74% were male, and 99% were white. Most patients received daily VIDAZA doses of 75 mg/m2. Most Commonly Occurring Adverse Reactions (Subcutaneous or Intravenous Route) in patients with MDS: nausea, anemia, thrombocytopenia, vomiting, pyrexia, leukopenia, diarrhea, injection site erythema, constipation, neutropenia, ecchymosis. The most common adverse reactions by intravenous route also included petechiae, rigors, weakness and hypokalemia. Adverse Reactions Most Frequently (>2%) Resulting in Clinical Intervention (Subcutaneous or Intravenous Route) in patients with MDS: Discontinuation: leukopenia, thrombocytopenia, neutropenia. Dose Held: leukopenia, neutropenia, thrombocytopenia, pyrexia, pneumonia, febrile neutropenia. Dose Reduced: leukopenia, neutropenia, thrombocytopenia. Table 1 presents adverse reactions occurring in at least 5% of patients treated with VIDAZA (subcutaneous) in Studies 1 and 2. It is important to note that duration of exposure was longer for the VIDAZA-treated group than for the observation group: patients received VIDAZA for a mean of 11.4 months while mean time in the observation arm was 6.1 months. Table 1: Most Frequently Observed Adverse Reactions ( 5% in All Subcutaneous VIDAZA Treated Patients; Studies 1 and 2) Number (%) of Patients System Organ Class All VIDAZAb Observationc Preferred Terma (N=220) (N=92) Blood and lymphatic system disorders Anemia 153 (70) 59 (64) Anemia aggravated 12 (6) 5 (5) Febrile neutropenia 36 (16) 4 (4) Leukopenia 106 (48) 27 (29) Neutropenia 71 (32) 10 (11) Thrombocytopenia 144 (66) 42 (46) Gastrointestinal disorders Abdominal tenderness 26 (12) 1 (1) Constipation 74 (34) 6 (7) Diarrhea 80 (36) 13 (14) Gingival bleeding 21 (10) 4 (4) Loose stools 12 (6) 0 Mouth hemorrhage 11 (5) 1 (1) Nausea 155 (71) 16 (17) Stomatitis 17 (8) 0 Vomiting 119 (54) 5 (5) General disorders and administration site conditions Chest pain 36 (16) 5 (5) Injection site bruising 31 (14) 0 Injection site erythema 77 (35) 0 Injection site granuloma 11 (5) 0 Injection site pain 50 (23) 0 Injection site pigmentation changes 11 (5) 0 Injection site pruritus 15 (7) 0 Table 1: Most Frequently Observed Adverse Reactions ( 5% in All Subcutaneous VIDAZA Treated Patients; Studies 1 and 2) Number (%) of Patients System Organ Class All VIDAZAb Observationc Preferred Terma (N=220) (N=92) Injection site reaction 30 (14) 0 Injection site swelling 11 (5) 0 Lethargy 17 (8) 2 (2) Malaise 24 (11) 1 (1) Pyrexia 114 (52) 28 (30) Infections and infestations Nasopharyngitis 32 (15) 3 (3) Pneumonia 24 (11) 5 (5) Upper respiratory tract infection 28 (13) 4 (4) Injury, poisoning, and procedural complications Post procedural hemorrhage 13 (6) 1 (1) Metabolism and nutrition disorders Anorexia 45 (21) 6 (7) Musculoskeletal and connective tissue disorders Arthralgia 49 (22) 3 (3) Chest wall pain 11 (5) 0 Myalgia 35 (16) 2 (2) Nervous system disorders Dizziness 41 (19) 5 (5) Headache 48 (22) 10 (11) Psychiatric disorders Anxiety 29 (13) 3 (3) Insomnia 24 (11) 4 (4) Respiratory, thoracic and mediastinal disorders Dyspnea 64 (29) 11 (12) Skin and subcutaneous tissue disorders Dry skin 11 (5) 1 (1) Ecchymosis 67 (31) 14 (15) Erythema 37 (17) 4 (4) Rash 31 (14) 9 (10) Skin nodule 11 (5) 1 (1) Urticaria 13 (6) 1 (1) Vascular disorders Hematoma 19 (9) 0 Hypotension 15 (7) 2 (2) Petechiae 52 (24) 8 (9) a Multiple terms of the same preferred terms for a patient are only counted once within each treatment group. b Includes adverse reactions from all patients exposed to VIDAZA, including patients after crossing over from observations. c Includes adverse reactions from observation period only; excludes any adverse events after crossover to VIDAZA. Table 2 presents adverse reactions occurring in at least 5% of patients treated with VIDAZA in Study 4. Similar to Studies 1 and 2 described above, duration of exposure to treatment with VIDAZA was longer (mean 12.2 months) compared with best supportive care (mean 7.5 months). Table 2: Most Frequently Observed Adverse Reactions ( 5% in the VIDAZA Treated Patients and the Percentage with NCI CTC Grade 3/4 Reactions; Study 4) Number (%) of Patients Any Grade Grade 3/4 Best Best Supportive Supportive System Organ Class VIDAZA Care Only VIDAZA Care Only Preferred Terma (N=175) (N=102) (N=175) (N=102) Blood and lymphatic system disorders Anemia 90 (51) 45 (44) 24 (14) 9 (9) Febrile neutropenia 24 (14) 10 (10) 22 (13) 7 (7) Leukopenia 32 (18) 2 (2) 26 (15) 1 (1) Neutropenia 115 (66) 29 (28) 107 (61) 22 (22) Thrombocytopenia 122 (70) 35 (34) 102 (58) 29 (28) Gastrointestinal disorders Abdominal pain 22 (13) 7 (7) 7 (4) 0 Constipation 88 (50) 8 (8) 2 (1) 0 Dyspepsia 10 (6) 2 (2) 0 0 Nausea 84 (48) 12 (12) 3 (2) 0 Vomiting 47 (27) 7 (7) 0 0 General disorders and administration site conditions Fatigue 42 (24) 12 (12) 6 (3) 2 (2) Injection site bruising 9 (5) 0 0 0 Injection site erythema 75 (43) 0 0 0 Injection site hematoma 11 (6) 0 0 0 Injection site induration 9 (5) 0 0 0 Injection site pain 33 (19) 0 0 0 Injection site rash 10 (6) 0 0 0 Injection site reaction 51 (29) 0 1 (1) 0 Pyrexia 53 (30) 18 (18) 8 (5) 1 (1) Infections and infestations Rhinitis 10 (6) 1 (1) 0 0 Upper respiratory tract infection 16 (9) 4 (4) 3 (2) 0 Urinary tract infection 15 (9) 3 (3) 3 (2) 0 Investigations Weight decreased 14 (8) 0 1 (1) 0 Metabolism and nutrition disorders Hypokalemia 11 (6) 3 (3) 3 (2) 3 (3) Nervous system disorders Lethargy 13 (7) 2 (2) 0 1 (1) Psychiatric disorders Anxiety 9 (5) 1 (1) 0 0 Insomnia 15 (9) 3 (3) 0 0 Renal and urinary disorders Hematuria 11 (6) 2 (2) 4 (2) 1 (1) Respiratory, thoracic and mediastinal disorders Dyspnea 26 (15) 5 (5) 6 (3) 2 (2) Dyspnea exertional 9 (5) 1 (1) 0 0 Pharyngolaryngeal pain 11 (6) 3 (3) 0 0 Skin and subcutaneous tissue disorders Erythema 13 (7) 3 (3) 0 0 Petechiae 20 (11) 4 (4) 2 (1) 0 Pruritus 21 (12) 2 (2) 0 0 Rash 18 (10) 1 (1) 0 0 Vascular disorders Hypertension 15 (9) 4 (4) 2 (1) 2 (2) a Multiple reports of the same preferred term from a patient were only counted once within each treatment. In Studies 1, 2 and 4 with subcutaneous administration of VIDAZA, adverse reactions of neutropenia, thrombocytopenia, anemia, nausea, vomiting, diarrhea, constipation, and injection site erythema/reaction tended to increase in incidence with higher doses of VIDAZA. Adverse reactions that tended to be more pronounced during the first 1 to 2 cycles of subcutaneous treatment compared with later cycles included thrombocytopenia, neutropenia, anemia, nausea, vomiting, injection site erythema/pain/bruising/reaction, constipation, petechiae, dizziness, anxiety, hypokalemia, and insomnia. There did not appear to be any adverse reactions that increased in frequency over the course of treatment. Overall, adverse reactions were qualitatively similar between the intravenous and subcutaneous studies. Adverse reactions that appeared to be specifically associated with the intravenous route of administration included infusion site reactions (e.g. erythema or pain) and catheter site reactions (e.g. infection, erythema, or hemorrhage). In clinical studies of either subcutaneous or intravenous VIDAZA, the following serious adverse reactions occurring at a rate of <5% (and not described in Tables 1 or 2) were reported: Blood and lymphatic system disorders: agranulocytosis, bone marrow failure, pancytopenia splenomegaly. Cardiac disorders: atrial fibrillation, cardiac failure, cardiac failure congestive, cardio- respiratory arrest, congestive cardiomyopathy. Eye disorders: eye hemorrhage Gastrointestinal disorders: diverticulitis, gastrointestinal hemorrhage, melena, perirectal abscess. General disorders and administration site conditions: catheter site hemorrhage, general physical health deterioration, systemic inflammatory response syndrome. Hepatobiliary disorders: cholecystitis. Immune system disorders: anaphylactic shock, hypersensitivity. Infections and infestations: abscess limb, bacterial infection, cellulitis, blastomycosis, injection site infection, Klebsiella sepsis, neutropenic sepsis, pharyngitis streptococcal, pneumonia Klebsiella, sepsis, septic shock, Staphylococcal bacteremia, Staphylococcal infection, toxoplasmosis. Metabolism and nutrition disorders: dehydration. Musculoskeletal and connective tissue disorders: bone pain aggravated, muscle weakness, neck pain. Neoplasms benign, malignant and unspecified: leukemia cutis. Nervous system disorders: cerebral hemorrhage, convulsions, intracranial hemorrhage. Renal and urinary disorders: loin pain, renal failure. Respiratory, thoracic and mediastinal disorders: hemoptysis, lung infiltration, pneumonitis, respiratory distress. Skin and subcutaneous tissue disorders: pyoderma gangrenosum, rash pruritic, skin induration. Surgical and medical procedures: cholecystectomy. Vascular disorders: orthostatic hypotension. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il and e-mailed to the Registration Holder’s Patient Safety Unit at: drugsafety@neopharmgroup.com 6.2 Post marketing Experience The following adverse reactions have been identified during post marketing use of VIDAZA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. − Interstitial lung disease − Tumor lysis syndrome − Injection site necrosis − Sweet’s syndrome (acute febrile neutrophilic dermatosis) − Necrotizing fasciitis (including fatal cases) − Differentiation syndrome − Pericardial effusion − Pericarditis − Cutaneous vasculitis 7. USE IN SPECIFIC POPULATIONS 7.1 Pregnancy Risk Summary Based on its mechanism of action and findings in animals, VIDAZA can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (10.1)]. There are no data on the use of azacitidine in pregnant women. Azacitidine was teratogenic and caused embryo-fetal lethality in animals at doses lower than the recommended human daily dose (see Data). Advise pregnant women of the potential risk to the fetus. The background rate of major birth defects and miscarriage is unknown for the indicated population. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. Data Animal Data Early embryotoxicity studies in mice revealed a 44% frequency of intrauterine embryonal death (increased resorption) after a single IP (intraperitoneal) injection of 6 mg/m2 (approximately 8% of the recommended human daily dose on a mg/m2 basis) azacitidine on gestation day 10. Developmental abnormalities in the brain have been detected in mice given azacitidine on or before gestation day 15 at doses of ~3- 12 mg/m2 (approximately 4%-16% the recommended human daily dose on a mg/m2 basis). In rats, azacitidine was clearly embryotoxic when given IP on gestation days 4-8 (postimplantation) at a dose of 6 mg/m2 (approximately 8% of the recommended human daily dose on a mg/m2 basis), although treatment in the preimplantation period (on gestation days 1-3) had no adverse effect on the embryos. Azacitidine caused multiple fetal abnormalities in rats after a single IP dose of 3 to 12 mg/m2 (approximately 8% the recommended human daily dose on a mg/m2 basis) given on gestation day 9, 10, 11 or 12. In this study azacitidine caused fetal death when administered at 3-12 mg/m2 on gestation days 9 and 10; average live animals per litter was reduced to 9% of control at the highest dose on gestation day 9. Fetal anomalies included: CNS anomalies (exencephaly/encephalocele), limb anomalies (micromelia, club foot, syndactyly, oligodactyly), and others (micrognathia, gastroschisis, edema, and rib abnormalities). 7.2 Lactation Risk Summary There is no information regarding the presence of azacitidine in human milk, the effects of VIDAZA on the breastfed infant, or the effects of VIDAZA on milk production. Because many drugs are excreted in human milk and because of the potential for tumorigenicity shown for azacitidine in animal studies [see Nonclinical Toxicology (11)] and the potential for serious adverse reactions in nursing infants from VIDAZA, advise patients not to breastfeed during treatment with VIDAZA and for 1 week after the last dose. 7.3 Females and Males of Reproductive Potential Based on its mechanism of action and findings in animals, VIDAZA can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (7.1)]. Pregnancy Testing Verify the pregnancy status of females of reproductive potential prior to initiating VIDAZA. Contraception Females Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with VIDAZA and for 6 months after the last dose. Males Advise males with female partners of reproductive potential to use effective contraception during treatment with VIDAZA and for 3 months after the last dose. Infertility Based on animal data, azacitidine could have an effect on male or female fertility [see Nonclinical Toxicology (11)]. 7.4 Pediatric Use Safety and effectiveness of VIDAZA in pediatric patients have not been established. 7.5 Geriatric Use Of the total number of patients in Studies 1, 2 and 3, 62% were 65 years and older and 21% were 75 years and older. No overall differences in effectiveness were observed between these patients and younger patients. In addition there were no relevant differences in the frequency of adverse reactions observed in patients 65 years and older compared to younger patients. Of the 179 patients randomized to azacitidine in Study 4, 68% were 65 years and older and 21% were 75 years and older. Survival data for patients 65 years and older were consistent with overall survival results. The majority of adverse reactions occurred at similar frequencies in patients <65 years of age and patients 65 years of age and older. Elderly patients are more likely to have decreased renal function. Monitor renal function in these patients [see Dosage and Administration (3.6) and Warnings and Precautions (5. 4)].

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. תסמונות מיאלודיספלסטיות בהתקיים אחד אלה: א. MDS (תסמונת מיאלודיספלסטית) המסווגת כ-Int 2/high לפי IPSS; ב. MDS בה מתקיימים לפחות שניים משלושת התנאים הבאים: 1. תלות בעירויי דם; 2. טסיות ברמה של 50,000 או פחות; 3. גרנולוציטים ברמה של 1,000 או פחות. ג. חולים סימפטומטיים הסובלים מדימומים או זיהומים חוזרים. 2. בשילוב עם Venetoclax, לטיפול בלוקמיה מסוג AML בחולה שטרם קיבל טיפול סיסטמי למחלתו ואיננו מתאים לטיפול בכימותרפיה אינטנסיבית. ב. לא יינתנו התרופות Decitabine, Azacitidine בו בזמן.ג. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| בשילוב עם Venetoclax, לטיפול בלוקמיה מסוג AML בחולה שטרם קיבל טיפול סיסטמי למחלתו ואיננו מתאים לטיפול בכימותרפיה אינטנסיבית | 16/01/2019 | המטולוגיה | לוקמיה מסוג AML | |
| תסמונות מיאלודיספלסטיות | 01/03/2008 | המטולוגיה | AZACITIDINE, DECITABINE | תסמונות מיאלודיספלסטיות |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2008
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
