Quest for the right Drug
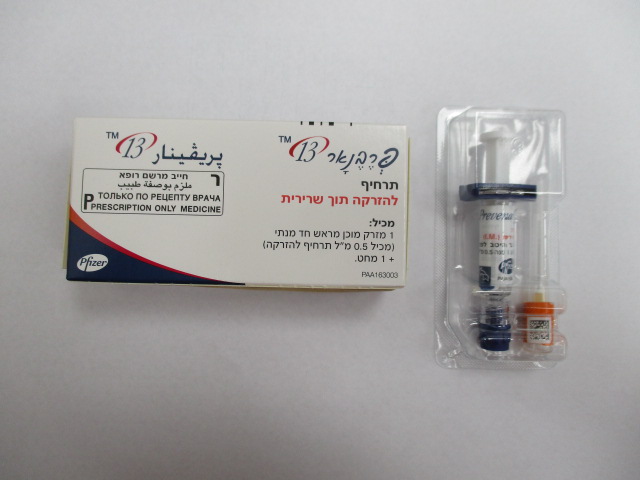
פרבנאר 13 PREVENAR 13 (PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 1, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 14, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 18C, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 19 F, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 19A, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 23F, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 3, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 4, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 5, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 6A, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 6B, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 7F, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 9V)
צורת מתן:
תוך-שרירי : I.M
צורת מינון:
תרחיף להזרקה : SUSPENSION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Analysis of postmarketing reporting rates suggests a potential increased risk of convulsions, with or without fever, and HHE when comparing groups which reported use of Prevenar 13 with Infanrix hexa to those which reported use of Prevenar 13 alone. Adverse reactions reported in clinical studies or from the postmarketing experience for all age groups are listed in this section per system organ class, in decreasing order of frequency and seriousness. The frequency is defined as follows: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), not known (cannot be estimated from available data). Infants and children aged 6 weeks to 5 years The safety of the vaccine was assessed in controlled clinical studies where 14,267 doses were given to 4,429 healthy infants from 6 weeks of age at first vaccination and 11-16 months of age at booster dose. In all infant studies, Prevenar 13 was co-administered with routine paediatric vaccines (see section 4.5). Safety in 354 previously unvaccinated children (7 months to 5 years of age) was also assessed. The most commonly reported adverse reactions in children 6 weeks to 5 years of age were vaccination-site reactions, fever, irritability, decreased appetite, and increased and/or decreased sleep. In a clinical study in infants vaccinated at 2, 3, and 4 months of age, fever ≥ 38°C was reported at higher rates among infants who received Prevenar (7-valent) concomitantly with Infanrix hexa (28.3% to 42.3%) than in infants receiving Infanrix hexa alone (15.6% to 23.1%). After a booster dose at 12 to 15 months of age, fever ≥ 38°C was reported in 50.0% of infants who received Prevenar (7-valent) and Infanrix hexa at the same time as compared to 33.6% of infants receiving Infanrix hexa alone. These reactions were mostly moderate (less than or equal to 39°C) and transient. An increase in vaccination-site reactions was reported in children older than 12 months compared to rates observed in infants during the primary series with Prevenar 13. Adverse reactions from clinical studies In clinical studies, the safety profile of Prevenar 13 was similar to Prevenar. The following frequencies are based on adverse reactions assessed in Prevenar 13 clinical studies: Immune system disorders: Rare: Hypersensitivity reaction including face oedema, dyspnoea, bronchospasm Nervous system disorders: Uncommon: Convulsions (including febrile convulsions) Rare: Hypotonic-hyporesponsive episode Gastrointestinal disorders: Very common: Decreased appetite Common: Vomiting; diarrhoea Skin and subcutaneous tissue disorders: Common: Rash Uncommon: Urticaria or urticaria-like rash General disorders and administration site conditions: Very common: Pyrexia; irritability; any vaccination-site erythema, induration/swelling or pain/tenderness; somnolence; poor quality sleep Vaccination-site erythema or induration/swelling 2.5 cm–7.0 cm (after the booster dose and in older children [age 2 to 5 years]) Common: Pyrexia > 39°C; vaccination-site movement impairment (due to pain); vaccination-site erythema or induration/swelling 2.5 cm–7.0 cm (after infant series) Uncommon: Vaccination-site erythema, induration/swelling > 7.0 cm; crying Additional information in special populations: Apnoea in very premature infants (≤ 28 weeks of gestation) (see section 4.4). Children and adolescents aged 6 to 17 years of age Safety was evaluated in 592 children (294 children aged 5 to 10 years previously immunised with at least one dose of Prevenar and 298 children aged 10 to 17 years who had not received a pneumococcal vaccine). The most common adverse events in children and adolescents 6 to 17 years of age were: Nervous system disorders: Common: Headaches Gastrointestinal disorders: Very common: Decreased appetite Common: Vomiting; diarrhoea Skin and subcutaneous tissue disorders: Common: Rash; urticaria or urticaria-like rash General disorders and administration site conditions: Very common: Irritability; any vaccination-site erythema; induration/swelling or pain/tenderness; somnolence; poor quality sleep; vaccination-site tenderness (including impaired movement) Common: Pyrexia Other adverse events previously observed in infants and children 6 weeks to 5 years of age may also be applicable to this age group but were not seen in this study possibly due to the small sample size. Additional information in special populations Children and adolescents with sickle cell disease, HIV infection, or an haematopoietic stem cell transplant have similar frequencies of adverse reactions, except that headaches, vomiting, diarrhoea, pyrexia, fatigue, arthralgia, and myalgia were very common. Adults ≥ 18 years and the elderly Safety was assessed in 7 clinical studies including 91,593 adults ranging in age from 18 to 101 years. Prevenar 13 was administered to 48,806 adults; 2,616 (5.4%) aged 50 to 64 years, and 45,291 (92.8%) aged 65 years and older. One of the 7 studies included a group of adults (n=899) ranging from 18 to 49 years who received Prevenar 13 and who were not previously vaccinated with 23-valent pneumococcal polysaccharide vaccine. Of the Prevenar 13 recipients 1,916 adults were previously vaccinated with the 23-valent pneumococcal polysaccharide vaccine at least 3 years prior to study vaccination, and 46,890 were 23-valent pneumococcal polysaccharide vaccine unvaccinated. A trend to lower frequency of adverse reactions was associated with greater age; adults > 65 years of age (regardless of prior pneumococcal vaccination status) reported fewer adverse reactions than younger adults, with adverse reactions generally most common in the youngest adults, 18 to 29 years of age. Overall, the frequency categories were similar for all age groups, with the exception of vomiting which was very common (≥ 1/10) in adults aged 18 to 49 years and common (≥ 1/100 to < 1/10) in all other age groups, and pyrexia was very common in adults aged 18 to 29 years and common in all other age groups. Severe vaccination-site pain/tenderness and severe limitation of arm movement was very common in adults 18 to 39 years and common in all other age groups. Adverse reactions from clinical studies Local reactions and systemic events were solicited daily after each vaccination for 14 days in 6 studies and 7 days in the remaining study. The following frequencies are based on adverse reactions assessed in Prevenar 13 clinical studies in adults: Metabolism and nutrition disorders: Very common: Decreased appetite Nervous system disorders: Very common: Headaches Gastrointestinal disorders: Very common: Diarrhoea; vomiting (in adults aged 18 to 49 years) Common: Vomiting (in adults aged 50 years and over) Uncommon: Nausea Immune system disorders: Uncommon: Hypersensitivity reaction including face oedema, dyspnoea, bronchospasm Skin and subcutaneous tissue disorders: Very common: Rash General disorders and administration site conditions: Very common: Chills; fatigue; vaccination-site erythema; vaccination-site induration/swelling; vaccination-site pain/tenderness (severe vaccination-site pain/tenderness very common in adults aged 18 to 39 years); limitation of arm movement (severe limitation of arm movements very common in adults aged 18 to 39 years) Common: Pyrexia (very common in adults aged 18 to 29 years) Uncommon: Lymphadenopathy localized to the region of the vaccination-site Musculoskeletal and connective tissue disorders: Very common: Arthralgia; myalgia Overall, no significant differences in frequencies of adverse reactions were seen when Prevenar 13 was given to adults previously vaccinated with the pneumococcal polysaccharide vaccine. Additional information in special populations Adults with HIV infection have similar frequencies of adverse reactions, except that pyrexia and vomiting were very common and nausea common. Adults with an haematopoietic stem cell transplant have similar frequencies of adverse reactions, except that pyrexia and vomiting were very common. Higher frequency in some solicited systemic reactions was observed when Prevenar 13 was administered concomitantly with trivalent inactivated influenza vaccine (TIV) compared to TIV given alone (headache, chills, rash, decreased appetite, arthralgia, and myalgia) or Prevenar 13 given alone (headache, fatigue, chills, decreased appetite, and arthralgia). Adverse reactions from Prevenar 13 postmarketing experience The following are considered adverse drug reactions for Prevenar 13; because these reactions were derived from spontaneous reports, the frequencies could not be determined and are thus considered as not known. Blood and lymphatic system disorders: Lymphadenopathy (localised to the region of the vaccination-site) Immune system disorders: Anaphylactic/anaphylactoid reaction including shock; angioedema Skin and subcutaneous tissue disorders: Erythema multiforme General disorders and administration site conditions: Vaccination-site urticaria; vaccination-site dermatitis; vaccination-site pruritus; flushing Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/

פרטי מסגרת הכללה בסל
התרופה תינתן לילדים החל מגיל 8 שבועות ועד לגיל 59 חודשים, אשר משתייכים לקבוצות הסיכון האלה: 1. הפרעות בפעילות הטחול (אנטומיות או תפקודיות), כגון כריתת טחול, חוסר טחול מולד, אנמיה חרמשית (SCD) וכדומה. 2. ליקויים אימונולוגיים עקב: א. מחלות ממאירות, כגון לוקמיה ולימפומה. ב. טיפול מדכא חסינות (כגון הקרנות, חומרים ציטוטוקסיים). ג. זיהום HIV. ד. כל מצב רפואי אחר, המלווה בליקויים של מערכת החיסון. 3. השתלת איברים, שתל קוכליארי ומח עצם. 4. דליפות נוזל חוט שדרה עם סיכון לדלקת עוצבה חוזרת. 5. אי ספיקת כליות כרונית, תסמונת נפרוטית, טיפול בדיאליזה. 6. חולי Ataxia Telangiectasia.
מידע נוסף
