Quest for the right Drug
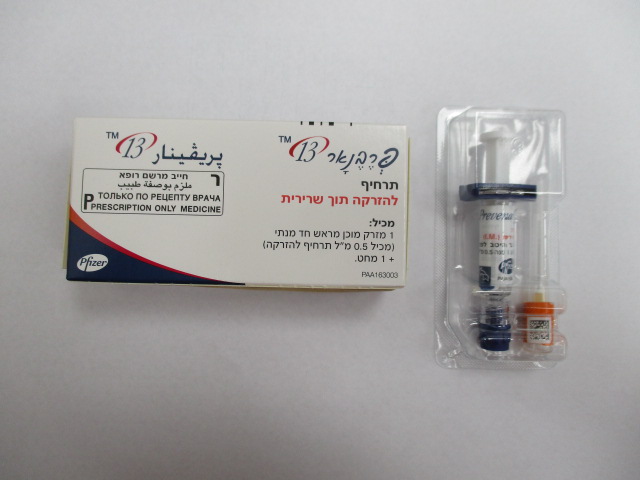
פרבנאר 13 PREVENAR 13 (PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 1, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 14, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 18C, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 19 F, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 19A, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 23F, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 3, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 4, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 5, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 6A, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 6B, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 7F, PNEUMOCOCCAL POLYSACCHARIDE SEROTYPE 9V)
צורת מתן:
תוך-שרירי : I.M
צורת מינון:
תרחיף להזרקה : SUSPENSION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: vaccines, pneumococcal vaccines; ATC code: J07AL02 Prevenar 13 contains the 7 pneumococcal capsular polysaccharides that are in Prevenar (4, 6B, 9V, 14, 18C, 19F, 23F) plus 6 additional polysaccharides (1, 3, 5, 6A, 7F, 19A) all conjugated to CRM197 carrier protein. Burden of disease Infants and children aged 6 weeks to 5 years Based on serotype surveillance in Europe performed before the introduction of Prevenar, Prevenar 13 is estimated to cover 73-100% (depending on the country) of serotypes causing invasive pneumococcal disease (IPD) in children less than 5 years of age. In this age group, serotypes 1, 3, 5, 6A, 7F, and 19A account for 15.6% to 59.7% of invasive disease, depending on the country, the time period studied, and the use of Prevenar. Acute otitis media (AOM) is a common childhood disease with different aetiologies. Bacteria can be responsible for 60-70% of clinical episodes of AOM. S. pneumoniae is one of the most common causes of bacterial AOM worldwide. Prevenar 13 is estimated to cover over 90% of serotypes causing antimicrobial -resistant IPD. Children and adolescents aged 6 to 17 years In children and adolescents aged 6 to 17 years, the incidence of pneumococcal disease is low, however, there is an increased risk of morbidity and mortality in those with underlying comorbidities. Adults ≥18 years and the elderly Pneumonia is the most common clinical presentation of pneumococcal disease in adults. The reported incidence of community-acquired pneumonia (CAP) and IPD in Europe varies by country, increases with age from 50 years and is highest in individuals aged ≥ 65 years. S. pneumoniae is the most frequent cause of CAP, and is estimated to be responsible for approximately 30% of all CAP cases requiring hospitalisation in adults in developed countries. Bacteraemic pneumonia (approximately 80% of IPD in adults), bacteraemia without a focus, and meningitis are the most common manifestations of IPD in adults. Based on surveillance data following the introduction of Prevenar but before the introduction of Prevenar 13 in childhood vaccination programmes, the pneumococcal serotypes in Prevenar 13 may be responsible for at least 50 – 76% (depending on country) of IPD in adults. The risk for CAP and IPD in adults also increases with chronic underlying medical conditions, specifically, anatomical or functional asplenia, diabetes mellitus, asthma, chronic cardiovascular, pulmonary, kidney or liver disease, and it is highest in those who are immune-suppressed such as those with malignant haematological diseases or HIV infection. Prevenar 13 immunogenicity clinical studies in infants, children and adolescents The protective efficacy of Prevenar 13 against IPD has not been studied. As recommended by the World Health Organization (WHO) the assessment of potential efficacy against IPD in infants and young children has been based on a comparison of immune responses to the seven common serotypes shared between Prevenar 13 and Prevenar, for which protective efficacy has been proven. Immune responses to the additional 6 serotypes were also measured. Immune responses following a three-dose primary infant series Clinical studies have been conducted in a number of European countries and the US using a range of vaccination schedules, including two randomised non-inferiority studies (Germany using a 2, 3, 4 month primary series [006] and US using a 2, 4, 6 month primary series [004]). In these two studies pneumococcal immune responses were compared using a set of non-inferiority criteria including the percentage of subjects with serum anti-polysaccharide serotype-specific IgG ≥ 0.35 μg/ml one month after the primary series and the comparison of IgG geometric mean concentrations (ELISA GMCs); in addition, functional antibody titres (OPA) between subjects receiving Prevenar 13 and Prevenar were compared. For the six additional serotypes, these values were compared with the lowest response among all of the seven common serotypes in the Prevenar recipients. The non-inferiority immune response comparisons for study 006, based on the proportion of infants achieving anti-polysaccharide IgG concentrations ≥ 0.35 μg/ml, are shown in Table 1. Results for study 004 were similar. Prevenar 13 non-inferiority (lower bound of the 95% CI for the difference in percentage of responders at 0.35 µg/ml between groups was >-10%) was demonstrated for all 7 common serotypes, except for serotype 6B in study 006 and serotypes 6B and 9V in study 004, which missed by a small margin. All seven common serotypes met pre-defined non-inferiority criteria for IgG ELISA GMCs. Prevenar 13 elicited comparable, although slightly lower, antibody levels than Prevenar for the 7 common serotypes. The clinical relevance of these differences is not known. Non-inferiority was met for the 6 additional serotypes based on the proportion of infants achieving antibody concentrations ≥ 0.35 μg/ml and comparison of IgG ELISA GMCs in study 006 and was met for 5 out of the 6 serotypes, with the exception of serotype 3 for study 004. For serotype 3, the percentages of Prevenar 13 recipients with serum IgG ≥ 0.35 μg/ml were 98.2% (study 006) and 63.5% (study 004). Table 1: Comparison of the proportion of subjects achieving a pneumococcal anti-polysaccharide IgG antibody concentration ≥ 0.35 μg/ml after dose 3 of the infant series – study 006 Prevenar 13 7-valent Prevenar % % Difference Serotypes (N=282-285) (N=277-279) (95 % CI) 7-valent Prevenar serotypes 4 98.2 98.2 0.0 (-2.5, 2.6) 6B 77.5 87.1 -9.6 (-16.0, -3.3) 9V 98.6 96.4 2.2 (-0.4, 5.2) 14 98.9 97.5 1.5 (-0.9, 4.1) 18C 97.2 98.6 -1.4 (-4.2, 1.2) 19F 95.8 96.0 -0.3 (-3.8, 3.3) 23F 88.7 89.5 -0.8 (-6.0, 4.5) Additional serotypes in Prevenar 13 1 96.1 87.1* 9.1 (4.5, 13.9) 3 98.2 87.1 11.2 (7.0, 15.8) 5 93.0 87.1 5.9 (0.8, 11.1) 6A 91.9 87.1 4.8 (-0.3, 10.1) 7F 98.6 87.1 11.5 (7.4, 16.1) 19A 99.3 87.1 12.2 (8.3, 16.8) * The serotype in Prevenar with the lowest percent response rate was 6B in study 006 (87.1 %). Prevenar 13 elicited functional antibodies to all 13 vaccine serotypes in studies 004 and 006. For the 7 common serotypes there were no differences between groups in the proportion of subjects with OPA titres ≥ 1:8. For each of the seven common serotypes, > 96% and >90 % of the Prevenar 13 recipients reached an OPA titre ≥ 1:8 one month after the primary series in studies 006 and 004, respectively. For each of the 6 additional serotypes, Prevenar 13 elicited OPA titres ≥ 1:8 in 91.4% to 100% of vaccinees one month after the primary series in studies 004/006. The functional antibody (OPA) geometric mean titres for serotypes 1, 3 and 5 were lower than the titres for each of the other additional serotypes; the clinical relevance of this observation for protective efficacy is unknown. Immune responses following a two-dose primary infant series The immunogenicity after two doses in infants has been documented in four studies. The proportion of infants achieving a pneumococcal anti-capsular polysaccharide IgG concentration ≥ 0.35 µg/ml one month after the second dose ranged from 79.6% to 98.5% across 11 of the 13 vaccine serotypes. Smaller proportions of infants achieved this antibody concentration threshold for serotype 6B (27.9% to 57.3%) and 23F (55.8% to 68.1%) for all studies using a 2, 4 month regimen, compared to 58.4% for serotype 6B and 68.6% for 23F for a study using a 3, 5 month regimen. After the booster dose, all vaccine serotypes including 6B and 23F had immune responses consistent with adequate priming with a two-dose primary series. In a UK study, the functional antibody (OPA) responses were comparable for all serotypes including 6B and 23F in the Prevenar and Prevenar 13 arms after the primary series at two and four months of age and after the booster dose at 12 months of age. For Prevenar 13 recipients, the proportion of responders with an OPA titre ≥ 1:8 was at least 87 % following the infant series, and at least 93% following the booster dose. The OPA geometric mean titres for serotypes 1, 3 and 5 were lower than the titres for each of the other additional serotypes; the clinical relevance of this observation is unknown. Booster responses following two-dose and three-dose primary infant series Following the booster dose, antibody concentrations increased from the pre-booster level for all 13 serotypes. Post-booster antibody concentrations were higher for 12 serotypes than those achieved after the infant primary series. These observations are consistent with adequate priming (the induction of immunologic memory). The immune response for serotype 3 following the booster dose was not increased above the levels seen after the infant vaccination series; the clinical relevance of this observation regarding the induction of serotype 3 immune memory is unknown. Antibody responses to booster doses following two-dose or three-dose infant primary series were comparable for all 13 vaccine serotypes. For children aged from 7 months to 5 years, age appropriate catch-up immunisation schedules (as described in section 4.2) result in levels of anti-capsular polysaccharide IgG antibody responses to each of the 13 serotypes that are at least comparable to those of a three-dose primary series in infants. Antibody persistence and immunological memory were evaluated in a study in healthy children who received a single dose of Prevenar 13 at least 2 years after they had been previously immunised with either 4 doses of Prevenar, a 3-dose infant series of Prevenar followed by Prevenar 13 at 12 months of age, or 4 doses of Prevenar 13. The single dose of Prevenar 13, in children approximately 3.4 years of age regardless of previous vaccination history with Prevenar or Prevenar 13, induced a robust antibody response for both the 7 common serotypes and the 6 additional serotypes in Prevenar 13. Since the introduction of 7-valent Prevenar in 2000, pneumococcal disease surveillance data have not shown that the immunity elicited by Prevenar in infancy has waned over time. Preterm Infants Safety and immunogenicity of Prevenar 13 given at 2, 3, 4 and 12 months was assessed in approximately 100 prematurely born infants (mean Estimated Gestational Age [EGA], 31 weeks; range, 26 to 36 weeks) and compared with approximately 100 infants born at term (mean EGA, 39 weeks; range, 37 to 42 weeks). Immune responses in preterm and term infants were compared using the proportion of subjects achieving a pneumococcal polysaccharide IgG binding antibody concentration ≥0.35 μg/mL 1 month after the infant series, the approach used for immunogenicity comparisons of Prevenar 13 to Prevenar based on WHO guidelines. More than 85% achieved a pneumococcal polysaccharide IgG binding antibody concentration ≥0.35 µg/mL 1 month after the infant series, except for serotypes 5 (71.7%), 6A (82.7%), and 6B (72.7%) in the preterm group. For these 3 serotypes, the proportion of responders among preterm infants was significantly lower than among term infants. Approximately one month after the toddler dose, the proportion of subjects in each group achieving this same antibody concentration threshold was >97%, except for serotype 3 (71% in preterm infants and 79% in term infants). It is unknown whether immunological memory to all serotypes is induced in pre-term infants. In general, serotype- specific IgG GMCs were lower for preterm infants than term infants. After the infant series, OPA GMTs were similar in preterm infants compared to term infants except for serotype 5, which was lower in preterm infants. OPA GMTs after the toddler dose relative to those after the infant series were similar or lower for 4 serotypes (4, 14, 18C, and 19F) and were statistically significantly higher for 6 of 13 serotypes (1, 3, 5, 7F, 9V, and 19A) in preterm infants compared to 10 of 13 serotypes (1, 3, 4, 5, 6A, 7F, 9V, 18C, 19A, and 23F) in term infants. Children (12-59 months) completely immunised with Prevenar (7-valent) Following administration of a single dose of Prevenar 13 to children (12-59 months) who are considered completely immunised with Prevenar (7-valent) (either 2 or 3 dose primary series plus booster), the proportion achieving serum IgG levels ≥0.35 µg/ml and OPA titres ≥1:8 was at least 90%. However, 3 (serotypes 1, 5 and 6A) of the 6 additional serotypes showed lower IgG GMC and OPA GMT when compared with children who had received at least one previous vaccination with Prevenar 13. The clinical relevance of the lower GMCs and GMTs is currently unknown. Unvaccinated Children (12-23 months) Studies in unvaccinated children (12-23 months) with Prevenar (7-valent) demonstrated that 2 doses were required to achieve serum IgG concentrations for 6B and 23F similar to those induced by a 3- dose infant series. Children and Adolescents 5 to 17 years of age In an open-label study in 592 healthy children and adolescents including those with asthma (17.4%) who may be predisposed to pneumococcal infection, Prevenar 13 elicited immune responses to all 13 serotypes. A single dose of Prevenar 13 was given to children 5 to 10 years of age previously vaccinated with at least 1 dose of Prevenar, and children and adolescents 10 to 17 years of age who had never received a pneumococcal vaccine. In both the children 5 to 10 years of age and children and adolescents aged 10 to 17 years, the immune response to Prevenar 13 was non inferior to Prevenar for the 7 common serotypes and to Prevenar 13 for the 6 additional serotypes compared to the immune response after the fourth dose in infants vaccinated at 2, 4, 6 and 12-15 months of age as measured by serum IgG. In children and adolescents aged 10 to 17 years of age OPA GMTs 1 month after vaccination were noninferior to OPA GMTs in the 5 to 10 year old age group for 12 of the 13 serotypes (except serotype 3). Immune responses after subcutaneous administration Subcutaneous administration of Prevenar 13 was evaluated in a non-comparative study in 185 healthy Japanese infants and children who received 4 doses at 2, 4, 6 and 12-15 months of age. The study demonstrated that safety and immunogenicity were generally comparable with observations made in studies of intramuscular administration. Prevenar 13 Effectiveness Invasive Pneumococcal Disease Data published by Public Health England showed that, four years after the introduction of Prevenar as a two dose primary infant series with booster dose in the second year of life and with a 94% vaccine uptake, there was a 98% (95% CI 95; 99) reduction in disease caused by the 7 vaccine serotypes in England and Wales. Subsequently, four years following the switch to Prevenar 13, the additional reduction in incidence of IPD due to the 7 serotypes in Prevenar ranged from 76% in children less than 2 years of age to 91% in children 5-14 years of age. The serotype specific reductions for each of the 5 additional serotypes in Prevenar 13 (no cases of serotype 5 IPD were observed) by age group are shown in Table 2 and ranged from 68% (serotype 3) to 100% (serotype 6A) for children less than 5 years of age. Significant incidence reductions were also observed in older age groups who had not been vaccinated with Prevenar 13 (indirect effect). Table 2: Serotype specific number of cases and incidence reductions of IPD in 2013/14 compared to 2008/09-2009/10 (2008/10) by age in England and Wales <5 years of age 5 to 64 years of age ≥65 years of age 2008- 2013/ % Incidence 2008- 2013/ % 2008- 2013/ % Incidence 10§ 14§ reduction 10§ 14§ Incidence 10§ 14§ reduction (95% CI*) reduction (95% CI*) (95% CI*) Additional serotypes covered by Prevenar 13 1 59 (54) 5 (5) 91% 458 77 83% 102 13 87% (382) (71) (89) (13) (98%; (88%; (94%; 68%)** 74%)** 72%)** 3 26 (24) 8 (8) 68% 178 73 59% 256 143 44% (148) (68) (224) (146) (89%; 6%) (72%; (57%; 38%)** 27%)** 6A 10 (9) 0 (0) 100% 53 (44) 5 (5) 90% 94 (82) 5 (5) 95% (100%; (97%; (99%; 62%)** 56%)** 81%)** 7F 90 (82) 8 (8) 91% 430 160 63% 173 75 56% (361) (148) (152) (77) (97%; (71%; (70%; 74%)** 50%)** 37%)** 19A 85 (77) 7 (7) 91% 225 104 54% 279 97 65% (191) (97) (246) (99) (97%; (65%; (75%; 75%)** 32%)** 53%)** § Corrected for proportion of samples serotyped, missing age, denominator compared with 2009/10, and for the trend in total invasive pneumococcal disease up to 2009/10 (after which no trend correction was applied). * 95% CI inflated from a Poisson interval based on over-dispersion of 2.1 seen from modelling of 2000-06 pre-Prevenar all IPD data. ** p<0.005 to cover 6A where p=0.002 Otitis media (OM) In a published study performed in Israel, using a two dose primary series plus booster dose in the second year of life the impact of Prevenar 13 on OM was documented in a population based active surveillance system with tympanocentesis culturing of middle ear fluid in Israeli children less than 2 years of age with OM. Following the introduction of Prevenar and subsequently Prevenar 13 there was a decline in incidence from 2.1 to 0.1 cases per 1000 children (95%) for the Prevenar serotypes plus serotype 6A and a decline in incidence from 0.9 to 0.1 cases per 1000 children (89%) for the additional serotypes 1, 3, 5, 7F, and 19A in Prevenar 13. The annual overall pneumococcal incidence of OM declined from 9.6 to 2.1 cases per 1000 children (78%) between July 2004 (prior to the introduction of Prevenar) and June 2013 (post Prevenar 13 introduction). Pneumonia In a multicenter observational study in France comparing the periods before and after the switch from Prevenar to Prevenar 13, there was 16% (2060 to 1725 cases) reduction in all community acquired pneumonia (CAP) cases in emergency departments in children 1 month to 15 years of age. Reductions were 53% (167 to 79 cases) (p<0.001) for CAP cases with pleural effusion and 63% (64 to 24 cases) (p<0.001) for microbiologically confirmed pneumococcal CAP cases. In the second year after the introduction of Prevenar 13 the total number of CAP cases due to the 6 additional vaccine serotypes in Prevenar 13 was reduced from 27 to 7 isolates (74%). The decrease in all cause pneumonia cases was most pronounced in the younger vaccinated age groups with a decrease of 31.8% (757 to 516 cases) and 16.6% (833 to 695 cases) in the age groups <2 years and 2 to 5 years, respectively. The incidence in older, predominantly non-vaccinated children (>5 years) did not change over the duration of the study. In an ongoing surveillance system (2004 to 2013) to document the impact of Prevenar and subsequently Prevenar 13 on CAP in children less than 5 years in Southern Israel using a 2 dose primary series with a booster dose in the second year of life, there was a reduction of 68% (95% CI 73; 61) in outpatient visits and 32% (95% CI 39; 22) in hospitalizations for alveolar CAP following the introduction of Prevenar 13 when compared to the period before the introduction of Prevenar. Effect on nasopharyngeal carriage In a surveillance study in France in children presenting with acute otitis media, changes in nasopharyngeal (NP) carriage of pneumococcal serotypes were evaluated following the introduction of Prevenar (7-valent) and subsequently Prevenar 13. Prevenar 13 significantly reduced NP carriage of the 6 additional serotypes (and serotype 6C) combined and individual serotypes 6C, 7F, 19A when compared with Prevenar. A reduction in carriage was also seen for serotype 3 (2.5% vs 1.1%; p=0.1). There was no carriage of serotypes 1 and 5 observed. The effect of pneumococcal conjugate vaccination on nasopharyngeal carriage was studied in a randomised double-blind study in which infants received either Prevenar 13 or Prevenar (7-valent) at 2, 4, 6 and 12 months of age in Israel. Prevenar 13 significantly reduced newly identified NP acquisition of the 6 additional serotypes (and serotype 6C) combined and of individual serotypes 1, 6A, 6C, 7F, 19A when compared with Prevenar. There was no reduction seen in serotype 3 and for serotype 5 the colonization was too infrequent to assess impact. For 6 of the remaining 7 common serotypes, similar rates of NP acquisition were observed in both vaccine groups; for serotype 19F a significant reduction was observed. In this study, reductions of S. pneumoniae serotypes 19A, 19F, and 6A not susceptible to a number of antibiotics were documented. The reductions ranged between 34% and 62% depending on serotype and antibiotic. Prevenar (7-valent vaccine) protective efficacy in infants and children The efficacy of 7-valent Prevenar was evaluated in two major studies – the Northern California Kaiser Permanente (NCKP) study and the Finnish Otitis Media (FinOM) study. Both studies were randomised, double-blind, active-control studies in which infants were randomised to receive either Prevenar or control vaccine (NCKP, meningococcal serogroup C CRM-conjugate [MnCC] vaccine; FinOM, hepatitis B vaccine) in a four-dose series at 2, 4, 6, and 12-15 months of age. The efficacy results from these studies (for invasive pneumococcal disease, pneumonia, and acute otitis media) are presented below (Table 3). Table 3: Summary of efficacy of 7-valent Prevenar1 Test N VE2 95% CI 3 NCKP: Vaccine-serotype IPD 30,258 97% 85, 100 NCKP: Clinical pneumonia with abnormal chest X-ray 23,746 35% 4, 56 NCKP: Acute Otitis Media (AOM)4 23,746 Total episodes 7% 4, 10 Recurrent AOM (3 episodes in 6 months, or 4 episodes in 1 year) 9% 3, 15 Recurrent AOM (5 episodes in 6 months, or 6 episodes in 1 year) 23% 7, 36 Tympanostomy tube placement 20% 2, 35 FinOM: AOM 1,662 Total episodes 6% -4, 16 All pneumococcal AOM 34% 21, 45 Vaccine-serotype AOM 57% 44, 67 1 Per protocol 2 Vaccine efficacy 3 October 1995 to April 20, 1999 4 October 1995 to April 30, 1998 Prevenar (7-valent) effectiveness The effectiveness (both direct and indirect effect) of 7-valent Prevenar against pneumococcal disease has been evaluated in both three-dose and two-dose primary infant series immunisation programmes, each with booster doses (Table 4). Following the widespread use of Prevenar, the incidence of IPD has been consistently and substantially reduced. Using the screening method, serotype-specific effectiveness estimates for 2 doses under the age of 1 year in the UK were 66 % (-29, 91 %) and 100 % (25, 100 %) for serotype 6B and 23F, respectively. Table 4: Summary of effectiveness of 7-valent Prevenar for invasive pneumococcal disease Country Recommended Disease reduction, % 95% CI (year of introduction) schedule UK (England & Wales)1 2, 4, + 13 months Vaccine serotypes: 49, 95% (2006) Two doses under age 1: 85% USA (2000) 2, 4, 6, + 12-15 months Children < 52 Vaccine serotypes: 98% 97, 99% All serotypes: 77% 73, 79% Persons ≥ 653 Vaccine serotypes: 76% NA All serotypes: 38% NA Canada (Quebec)4 2, 4, + 12 months All serotypes: 73% NA (2004) Vaccine serotypes: 2-dose infant series: 99% 92, 100% Completed schedule:100% 82, 100% 1 Children < 2 years of age. Calculated vaccine effectiveness as of June 2008 (Broome method). 2 2005 data. 3 2004 data. 4 Children < 5 years of age. January 2005 to December 2007. Complete effectiveness for routine 2+1 schedule not yet available. Acute Otitis Media Effectiveness of Prevenar in a 3+1 schedule has also been observed against acute otitis media and pneumonia since its introduction in a national immunisation programme. In a retrospective evaluation of a large US insurance database, AOM visits were reduced by 42.7 % (95 % CI, 42.4-43.1 %), and prescriptions for AOM by 41.9 % in children younger than 2 years of age, compared with a pre-licensure baseline (2004 vs. 1997-99). In a similar analysis, hospitalisations and ambulatory visits for all-cause pneumonia were reduced by 52.4 % and 41.1 %, respectively. For those events specifically identified as pneumococcal pneumonia, the observed reductions in hospitalisations and ambulatory visits were 57.6 % and 46.9 %, respectively, in children younger than 2 years of age, compared with a pre-licensure baseline (2004 vs. 1997-99). While direct cause-and-effect cannot be inferred from observational analyses of this type, these findings suggest that Prevenar plays an important role in reducing the burden of mucosal disease (AOM and pneumonia) in the target population. Efficacy study in adults 65 years and older Efficacy against vaccine-type (VT) pneumococcal CAP and IPD was assessed in a large-scale randomised double-blind, placebo-controlled study (Community-Acquired Pneumonia Immunization Trial in Adults–CAPiTA) in the Netherlands. 84,496 subjects, 65 years and older received a single vaccination of either Prevenar 13 or placebo in a 1:1 randomization. The CAPiTA study enrolled volunteers ≥ 65 years of age whose demographic and health characteristics may differ from those seeking vaccination. A first episode of hospitalised, chest X-ray confirmed pneumonia was identified in about 2% of this population (n=1,814 subjects) of which 329 cases were confirmed pneumococcal CAP and 182 cases were VT pneumococcal CAP in the per protocol and modified intent to treat (mITT) populations. Efficacy was demonstrated for the primary and secondary endpoints in the per protocol population (Table 5). Table 5: Vaccine efficacy (VE) for the primary and secondary endpoints of the CAPiTA study (per protocol population) Cases VE (%) Efficacy endpoint Prevenar 13 Placebo p-value Total (95.2% CI) group group Primary endpoint 45.56 First episode of confirmed VT 139 49 90 0.0006 (21.82, pneumococcal CAP 62.49) Secondary endpoints First episode of confirmed 45.00 NB/NI1 vaccine type 93 33 60 (14.21, 0.0067 pneumococcal CAP 65.31) 75.00 First episode of VT-IPD2 35 7 28 (41.06, 0.0005 90.87) 1 NB/NI – non-bacteraemic/non-invasive 2 VT-IPD – vaccine-type invasive pneumococcal disease The duration of protective efficacy against a first episode of VT pneumococcal CAP, NB/NI VT pneumococcal CAP, and VT-IPD extended throughout the 4-year study. The study was not designed to demonstrate efficacy in subgroups, and the number of subjects ≥ 85 years of age was not sufficient to demonstrate efficacy in this age group. A post-hoc analysis was used to estimate the following public health outcomes against clinical CAP (as defined in the CAPiTA study, and based on clinical findings regardless of radiologic infiltrate or etiologic confirmation): vaccine efficacy (VE), incidence rate reduction (IRR), and number needed to vaccinate (NNV) (Table 6). IRR, also referred to as vaccine preventable disease incidence, is the number of cases of vaccine preventable disease per 100,000 person-years of observation. In Table 6, NNV is a measure that quantifies the number of people that need to be vaccinated in order to prevent one clinical CAP case. Table 6: Vaccine efficacy (VE) against clinical CAP* Episodes Vaccine efficacy1 Incidence per Incidence Number % (95% CI) 100,000 person- rate needed to (1-sided p-value) years of reduction2 vaccinate 3 observation (95% CI) (PYO) Preven Placebo Prevena Placeb ar 13 r 13 o All 1375 1495 8.1 819.1 891.2 72.2 277 episodes (-0.6, 16.1) (-5.3, analysis (0.034) 149.6) First 1126 1214 7.3 670.7 723.7 53.0 378 episode (-0.4, 14.4) (-2.7, analysis (0.031) 108.7) * Patients with at least 2 of the following: Cough; purulent sputum, temperature >38°C or <36.1°C; pneumonia (auscultatory findings); leukocytosis; C-reactive protein value >3 times the upper limit of normal; hypoxemia with a partial oxygen pressure <60 mm Hg while breathing room air. 1 A Poisson regression model with random effects was used to calculate VE. 2 Per 100,000 person-years of observation. IRR is calculated as the incidence in the placebo group minus the incidence in the vaccine group, and was mathematically equivalent to VE × the incidence in the placebo group. 3 Based on a 5-year duration of protection. NNV is not a rate but instead indicates the number of cases prevented for a given number of persons vaccinated. NNV also incorporates the length of the trial or duration of protection and is calculated as 1 divided by the product of the IRR and duration of protection (or length of trial) (=1/(IRR × duration). Immunogenicity studies in adults ≥18 years and the elderly In adults, an antibody threshold of serotype-specific pneumococcal polysaccharide IgG binding antibody concentration associated with protection has not been defined. For all pivotal clinical trials, a serotype-specific opsonophagocytosis assay (OPA) was used as a surrogate to assess potential efficacy against invasive pneumococcal disease and pneumonia. OPA geometric mean titers (GMTs) measured 1-month after each vaccination were calculated. OPA titres are expressed as the reciprocal of the highest serum dilution that reduces survival of the pneumococci by at least 50 %. Pivotal trials for Prevenar 13 were designed to show that functional OPA antibody responses for the 13 serotypes are non-inferior, and for some serotypes superior, to the 12 serotypes in common with the licensed 23-valent pneumococcal polysaccharide vaccine [1, 3, 4, 5, 6B, 7F, 9V, 14, 18C, 19A, 19F, 23F] one month after vaccine administration. The response to serotype 6A, which is unique to Prevenar 13, was assessed by demonstration of a 4-fold increase in the specific OPA titer above pre- immunised levels. Five clinical studies were conducted in Europe and the USA evaluating the immunogenicity of Prevenar 13 in different age groups ranging from 18-95 years of age. Clinical studies with Prevenar 13 currently provide immunogenicity data in adults aged 18 years and older, including adults aged 65 and older previously vaccinated with one or more doses of 23-valent pneumococcal polysaccharide vaccine, 5 years prior to enrollment. Each study included healthy adults and immuno-competent adults with stable underlying conditions known to predispose individuals to pneumococcal infection (i.e., chronic cardiovascular disease, chronic pulmonary disease including asthma, renal disorders and diabetes mellitus, chronic liver disease including alcoholic liver disease), and adults with risk factors such as smoking and alcohol abuse. Immunogenicity and safety of Prevenar 13 has been demonstrated in adults aged 18 years and older including those previously vaccinated with a pneumococcal polysaccharide vaccine. Adults not previously vaccinated with 23-valent pneumococcal polysaccharide vaccine In a head-to-head, comparative trial conducted in adults aged 60-64 years, subjects received a single dose of either Prevenar 13 or 23-valent pneumococcal polysaccharide vaccine. In the same study another group of adults aged 50-59 years and another group of adults aged 18-49 years received a single dose of Prevenar 13. Table 7 compares the OPA GMTs, 1-month post-dose, in 60-64 year olds given either a single dose of Prevenar 13 or 23-valent pneumococcal polysaccharide vaccine, and in 50-59 year olds given a single dose of Prevenar 13. Table 7: OPA GMTs in adults aged 60-64 years given Prevenar 13 or 23-valent pneumococcal polysaccharide vaccine (PPSV23) and in adults aged 50-59 years given Prevenar 13a,b,c Prevenar 13 Prevenar 13 PPSV23 Prevenar 13 Prevenar 13 Relative 50-59 Years 60-64 Years 60-64 Years 50-59 Relative to to PPSV23, N=350-384 N=359-404 N=367-402 60-64 Years 60-64 Years Serotype GMT GMT GMT GMR (95% CI) GMR (95% CI) 1 200 146 104 1.4 (1.08, 1.73) 1.4 (1.10, 1.78) 3 91 93 85 1.0 (0.81, 1.19) 1.1 (0.90, 1.32) 4 2833 2062 1295 1.4 (1.07, 1.77) 1.6 (1.19, 2.13) 5 269 199 162 1.4 (1.01, 1.80) 1.2 (0.93, 1.62) 6A† 4328 2593 213 1.7 (1.30, 2.15) 12.1 (8.63, 17.08) 6B 3212 1984 788 1.6 (1.24, 2.12) 2.5 (1.82, 3.48) 7F 1520 1120 405 1.4 (1.03, 1.79) 2.8 (1.98, 3.87) 9V 1726 1164 407 1.5 (1.11, 1.98) 2.9 (2.00, 4.08) 14 957 612 692 1.6 (1.16, 2.12) 0.9 (0.64, 1.21) 18C 1939 1726 925 1.1 (0.86, 1.47) 1.9 (1.39, 2.51) 19A 956 682 352 1.4 (1.16, 1.69) 1.9 (1.56, 2.41) 19F 599 517 539 1.2 (0.87, 1.54) 1.0 (0.72, 1.28) 23F 494 375 72 1.3 (0.94, 1.84) 5.2 (3.67, 7.33) a Non-inferiority was defined as the lower limit of the 2-sided 95% CI for GMR was greater than 0.5. b Statistically significantly greater response was defined as the lower bound of the 2-sided 95% CI for the GMR was greater than 1. c For serotype 6A†, which is unique to Prevenar 13, a statistically significantly greater response was defined as the lower bound of the 2-sided 95% CI for the GMR being greater than 2. In adults aged 60-64 years, OPA GMTs to Prevenar 13 were non-inferior to the OPA GMTs elicited to the 23-valent pneumococcal polysaccharide vaccine for the twelve serotypes common to both vaccines. For 9 serotypes, the OPA titers were shown to be statistically significantly greater in Prevenar 13 recipients. In adults aged 50-59 years, OPA GMTs to all 13 serotypes in Prevenar 13 were non-inferior to the Prevenar 13 responses in adults aged 60-64 years. For 9 serotypes, immune responses were related to age, with adults in the 50-59 years group showing statistically significantly greater responses than adults aged 60-64 years. In all adults ≥ 50 years who received a single dose of Prevenar 13, the OPA titers to serotype 6A were significantly greater than in adults ≥ 60 years who received a single dose of 23-valent pneumococcal polysaccharide vaccine. One year after vaccination with Prevenar 13 OPA titers had declined compared to one month after vaccination, however, OPA titers for all serotypes remained higher than levels at baseline: OPA GMT levels at baseline OPA GMT levels one year after Prevenar 13 Adults 50-59 years not previously vaccinated with 23-valent 5 to 45 20 to 1234 pneumococcal polysaccharide vaccine Adults 60-64 years not previously vaccinated with 23-valent 5 to 37 19 to 733 pneumococcal polysaccharide vaccine Table 8 shows OPA GMTs 1-month after a single dose of Prevenar 13 in 18-49 year olds compared to 60-64 year olds. Table 8: OPA GMTs in adults aged 18-49 years and 60-64 years given Prevenar 13a,b 18-49 Years 18-49 Years 60-64 Years Relative to N=836-866 N=359-404 60-64 Years Serotype GMTb GMTb GMR (95% CIc) 1 353 146 2.4 (2.03, 2.87) 3 91 93 1.0 (0.84, 1.13) 4 4747 2062 2.3 (1.92, 2.76) 5 386 199 1.9 (1.55, 2.42) 6A 5746 2593 2.2 (1.84, 2.67) 6B 9813 1984 4.9 (4.13, 5.93) 7F 3249 1120 2.9 (2.41, 3.49) 9V 3339 1164 2.9 (2.34, 3.52) 14 2983 612 4.9 (4.01, 5.93) 18C 3989 1726 2.3 (1.91, 2.79) 19A 1580 682 2.3 (2.02, 2.66) 19F 1533 517 3.0 (2.44, 3.60) 23F 1570 375 4.2 (3.31, 5.31) a Non-inferiority was defined as the lower limit of the 2-sided 95% CI for GMR was greater than 0.5. b Statistically significantly greater response was defined as the lower bound of the 2-sided 95% CI for the GMR was greater than 1. c Confidence intervals (CIs) for the ratio are back transformations of a confidence interval based on the Student t distribution for the mean difference of the logarithms of the measures. In adults aged 18-49 years, OPA GMTs to all 13 serotypes in Prevenar 13 were non-inferior to the Prevenar 13 responses in adults aged 60-64 years. One year after vaccination with Prevenar 13 OPA titers had declined compared to one month after vaccination, however OPA titers for all serotypes remained higher than levels at baseline. OPA GMT levels at baseline OPA GMT levels one year after Prevenar 13 Adults 18-49 years not previously vaccinated with 23-valent 5 to 186 23 to 2948 pneumococcal polysaccharide vaccine Adults previously vaccinated with 23-valent pneumococcal polysaccharide vaccine Immune responses to Prevenar 13 and 23-valent pneumococcal polysaccharide vaccine were compared in a head to head trial in adults aged ≥ 70 years, who had received a single dose of pneumococcal polysaccharide vaccine at least 5 years before study vaccination. Table 9 compares the OPA GMTs, 1-month post-dose, in pneumococcal polysaccharide vaccinated adults aged ≥ 70 years given a single dose of either Prevenar 13 or 23-valent pneumococcal polysaccharide vaccine. Table 9: OPA GMTs in pneumococcal polysaccharide vaccinated adults aged ≥ 70 years given either Prevenar 13 or 23-valent pneumococcal polysaccharide vaccine (PPSV23)a,b,c Prevenar 13 PPSV23 Prevenar OPA GMT N=400-426 N=395-445 Relative to PPSV23 Serotype OPA GMT OPA GMT GMR (95% CI) 1 81 55 1.5 (1.17, 1.88) 3 55 49 1.1 (0.91, 1.35) 4 545 203 2.7 (1.93, 3.74) 5 72 36 2.0 (1.55, 2.63) † 6A 903 94 9.6 (7.00, 13.26) 6B 1261 417 3.0 (2.21, 4.13) 7F 245 160 1.5 (1.07, 2.18) 9V 181 90 2.0 (1.36, 2.97) 14 280 285 1.0 (0.73, 1.33) 18C 907 481 1.9 (1.42, 2.50) 19A 354 200 1.8 (1.43, 2.20) 19F 333 214 1.6 (1.17, 2.06) 23F 158 43 3.7 (2.69, 5.09) a Non-inferiority was defined as the lower limit of the 2-sided 95% CI for GMR was greater than 0.5. b Statistically significantly greater response was defined as the lower bound of the 2-sided 95% CI for the GMR was greater than 1. c For serotype 6A†, which is unique to Prevenar 13, a statistically significantly greater response was defined as the lower bound of the 2-sided 95% CI for the GMR greater than 2. In adults vaccinated with pneumococcal polysaccharide vaccine at least 5 years prior to the clinical study, OPA GMTs to Prevenar 13 were non-inferior to the 23-valent pneumococcal polysaccharide vaccine responses for the 12 serotypes in common. Furthermore, in this study statistically significantly greater OPA GMTs were demonstrated for 10 of the 12 serotypes in common. Immune responses to serotype 6A were statistically significantly greater following vaccination with Prevenar 13 than after 23-valent pneumococcal polysaccharide vaccine. One year after vaccination with Prevenar 13 in adults aged 70 years and over who were vaccinated with 23-valent pneumococcal polysaccharide vaccine, at least 5 years prior to study entry, OPA titers had declined compared to one month after vaccination, however, OPA titers for all serotypes remained higher than levels at baseline: OPA GMT levels at OPA GMT levels one year baseline after Prevenar 13 Adults ≥ 70 years vaccinated with 23-valent pneumococcal 9 to 122 18 to 381 polysaccharide vaccine at least 5 years prior Immune responses in Special Populations Individuals with the conditions described below have an increased risk of pneumococcal disease. The clinical relevance of the antibody levels elicited by Prevenar 13 in these special populations is unknown. Sickle cell disease An open label single arm study in France, Italy, UK, US, Lebanon, Egypt and Saudi Arabia with 2 doses of Prevenar 13 given 6 months apart was conducted in 158 children and adolescents ≥ 6 to < 18 years of age with sickle cell disease who were previously vaccinated with one or more doses of 23-valent pneumococcal polysaccharide vaccine at least 6 months prior to enrollment. After the first vaccination, Prevenar 13 elicited antibody levels measured by both IgG GMCs and OPA GMTs that were statistically significantly higher when compared to levels prior to vaccination. After the second dose immune responses were comparable to those after the first dose. One year after the second dose, antibody levels measured by both IgG GMCs and OPA GMTs were higher than levels prior to the first dose of Prevenar 13, except for the IgG GMCs for serotypes 3 and 5 that were numerically similar. Additional Prevenar (7-valent) immunogenicity data: children with sickle cell disease The immunogenicity of Prevenar has been investigated in an open-label, multicentre study in 49 infants with sickle cell disease. Children were vaccinated with Prevenar (3 doses one month apart from the age of 2 months), 46 of these children also received a 23-valent pneumococcal polysaccharide vaccine at the age of 15-18 months. After primary immunisation, 95.6 % of the subjects had antibody levels of at least 0.35 μg/ml for all seven serotypes found in Prevenar. A significant increase was seen in the concentrations of antibodies against the seven serotypes after the polysaccharide vaccination, suggesting that immunological memory was well established. HIV infection Children and adults not previously vaccinated with a pneumococcal vaccine HIV-infected children and adults with CD4 ≥ 200 cells/µL (mean 717.0 cells/μL), viral load < 50,000 copies/ml (mean 2090.0 copies/ml), free of active AIDS-related illness and not previously vaccinated with a pneumococcal vaccine received 3 doses of Prevenar 13. As per general recommendations, a single dose of 23-valent pneumococcal polysaccharide vaccine was subsequently administered. Vaccines were administered at 1 month intervals. Immune responses were assessed in 259-270 evaluable subjects approximately 1 month after each dose of vaccine. After the first dose, Prevenar 13 elicited antibody levels, measured by both IgG GMCs and OPA GMTs that were statistically significantly higher when compared to levels prior to vaccination. After the second and third dose of Prevenar 13, immune responses were similar or higher than those after the first dose. Adults previously vaccinated with 23-valent pneumococcal polysaccharide vaccine HIV-infected adults ≥ 18 years of age with CD4 ≥ 200 cells/µL (mean 609.1 cells/µL) and viral load < 50,000 copies/ml (mean 330.6 copies/ml), who were free of active AIDS-related illness and were previously vaccinated with 23-valent pneumococcal polysaccharide vaccine administered at least 6 months prior to enrollment, received 3 doses of Prevenar 13, at enrollment, 6 months, and 12 months after the first dose of Prevenar 13. Immune responses were assessed in 231-255 evaluable subjects approximately 1 month after each dose of Prevenar 13. After the first dose, Prevenar 13 elicited antibody levels measured by both IgG GMCs and OPA GMTs that were statistically significantly higher when compared to levels prior to vaccination. After the second and third dose of Prevenar 13, immune responses were comparable or higher than those after the first dose. In the study 162 subjects had received one prior dose of 23-valent pneumococcal polysaccharide vaccine, 143 subjects 2 prior doses and 26 subjects more than 2 prior doses of 23-valent polysaccharide vaccine. Subjects who received two or more previous doses of 23-valent pneumococcal polysaccharide vaccine showed a similar immune response compared with subjects who received a single previous dose. Haematopoietic stem cell transplant Children and adults with an allogeneic haematopoietic stem cell transplant (HSCT) at ≥ 2 years of age with complete haematologic remission of underlying disease or with very good partial remission in the case of lymphoma and myeloma received three doses of Prevenar 13 with an interval of at least 1 month between doses. The first dose was administered at 3 to 6 months after HSCT. A fourth (booster) dose of Prevenar 13 was administered 6 months after the third dose. As per general recommendations, a single dose of 23-valent pneumococcal polysaccharide vaccine was administered 1 month after the fourth dose of Prevenar 13. Immune responses as measured by IgG GMCs were assessed in 168-211 evaluable subjects approximately 1 month after vaccination. Prevenar 13 elicited increased antibody levels after each dose of Prevenar 13. Immune responses after the fourth dose of Prevenar 13 were significantly increased for all serotypes compared with after the third dose. Functional antibody titers (OPA titers) were not measured in this study.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Not applicable.

פרטי מסגרת הכללה בסל
התרופה תינתן לילדים החל מגיל 8 שבועות ועד לגיל 59 חודשים, אשר משתייכים לקבוצות הסיכון האלה: 1. הפרעות בפעילות הטחול (אנטומיות או תפקודיות), כגון כריתת טחול, חוסר טחול מולד, אנמיה חרמשית (SCD) וכדומה. 2. ליקויים אימונולוגיים עקב: א. מחלות ממאירות, כגון לוקמיה ולימפומה. ב. טיפול מדכא חסינות (כגון הקרנות, חומרים ציטוטוקסיים). ג. זיהום HIV. ד. כל מצב רפואי אחר, המלווה בליקויים של מערכת החיסון. 3. השתלת איברים, שתל קוכליארי ומח עצם. 4. דליפות נוזל חוט שדרה עם סיכון לדלקת עוצבה חוזרת. 5. אי ספיקת כליות כרונית, תסמונת נפרוטית, טיפול בדיאליזה. 6. חולי Ataxia Telangiectasia.
מידע נוסף
