Quest for the right Drug
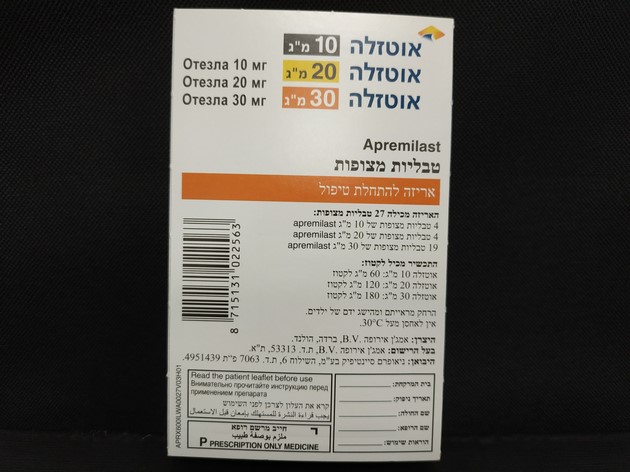
אוטזלה 10 מ"ג OTEZLA 10 MG (APREMILAST)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most commonly reported adverse reactions with apremilast in PsA and PSOR are gastrointestinal (GI) disorders including diarrhea (15.7%) and nausea (13.9%). The other most commonly reported adverse reactions include upper respiratory tract infections (8.4%), headache (7.9%), and tension headache (7.2%) and are mostly mild to moderate in severity. The most commonly reported adverse drug reactions with apremilast in BD are diarrhea (41.3%), nausea (19.2%), headache (14.4%), upper respiratory tract infection (11.5%), upper abdominal pain (8.7%), vomiting (8.7%) and back pain (7.7%) and are mostly mild to moderate in severity. The gastrointestinal adverse reactions generally occurred within the first 2 weeks of treatment and usually resolved within 4 weeks. Hypersensitivity reactions are uncommonly observed (see section 4.3). Tabulated list of adverse reactions The adverse reactions observed in patients treated with apremilast are listed below by system organ class (SOC) and frequency for all adverse reactions. Within each SOC and frequency grouping, adverse reactions are presented in order of decreasing seriousness. The adverse drug reactions were determined based on data from the apremilast clinical development program and post-marketing experience. The frequencies of adverse drug reactions are those reported in the apremilast arms of the four Phase III studies in PsA (n = 1945) or the two Phase III studies in PSOR (n=1184), and in the phase III study in BD (n=207) the highest frequency from either data pool is represented in Table 2. Frequencies are defined as: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); not known (cannot be estimated from the available data). Table 2. Summary of adverse reactions in psoriatic arthritis (PsA), psoriasis (PSOR) and Behçet’s disease (BD) System Organ Class Frequency Adverse reaction Infections and infestations Very common Upper respiratory tract infection a Common Bronchitis Nasopharyngitis* Immune system disorders Uncommon Hypersensitivity Metabolism and nutrition disorders Common Decreased appetite* Psychiatric disorders Common Insomnia Depression Uncommon Suicidal ideation and behavior Nervous system disorders Very common Headache* a Common Migraine* Tension headache* Respiratory, thoracic, and mediastinal Common Cough disorders Gastrointestinal disorders Very Common Diarrhea* Nausea* Common Vomiting* Dyspepsia Frequent bowel movements Upper abdominal pain * Gastroesophageal reflux disease Uncommon Gastrointestinal hemorrhage Skin and subcutaneous tissue disorders Uncommon Rash Urticaria Not known Angioedema Musculoskeletal and connective tissue Common Back pain* disorders General disorders and administration site Common Fatigue conditions Investigations Uncommon Weight decrease *At least one of these adverse reactions was reported as serious a Frequency reported as common in PSA and PSOR Description of selected adverse reactions Psychiatric disorders In clinical studies and post-marketing experience, uncommon cases of suicidal ideation and behavior, were reported, while completed suicide was reported post-marketing. Patients and caregivers should be instructed to notify the prescriber of any suicidal ideation (see section 4.4). Body weight loss Patient weight was measured routinely in clinical studies. The mean observed weight loss in PsA and PSOR patients treated for up to 52 weeks with apremilast was 1.99 kg. A total of 14.3% of patients receiving apremilast had observed weight loss between 5-10% while 5.7% of the patients receiving apremilast had observed weight loss greater than 10%. None of these patients had overt clinical consequences resulting from weight loss. A total of 0.1% of patients treated with apremilast discontinued due to adverse reaction of weight decreased. The mean observed weight loss in BD patients treated with apremilast for 52 weeks was 0.52 kg. A total of 11.8% of patients receving apremilast had observed weight loss between 5-10% while 3.8% of the patients receiving apremilast had observed weight loss greater than 10%. None of these patients had overt clinical consequences from weight loss. None of the patients discontinued the study due to adverse reaction of weight decreased. Please see additional warning in section 4.4 for patients who are underweight at beginning of treatment. Special populations Elderly patients From post-marketing experience, elderly patients ≥ 65 years of age may be at a higher risk of complications of severe diarrhea, nausea and vomiting (see section 4.4). Patients with hepatic impairment The safety of apremilast was not evaluated in PsA, PSOR or BD patients with hepatic impairment. Patients with renal impairment In the PsA, PSOR or BD clinical studies, the safety profile observed in patients with mild renal impairment was comparable to patients with normal renal function. The safety of apremilast was not evaluated in PsA, PSOR or BD patients with moderate or severe renal impairment in the clinical studies. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול במקרים האלה:1. חולה בוגר הסובל מדלקת מפרקים פסוריאטית (Psoriatic arthritis), לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs.2. חולה בוגר הסובל מפסוריאזיס, לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs ו/או PUVA ו/או Psoralen.3. טיפול בכיבים בחלל הפה בחולי בכצ'ט אחרי מיצוי טיפול בקולכיצין.ב. התכשיר לא יינתן בשילוב עם תכשירים ביולוגיים.ג. מתן התכשיר יינתן לחולה בהתאם למרשם של מומחה ברפואת עור ומין או מומחה בראומטולוגיה או מומחה בגסטרואנטרולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| כיבים בחלל הפה בחולי בכצ'ט אחרי מיצוי טיפול בקולכיצין | 01/03/2021 | ראומטולוגיה | Behcet disease | |
| מפסוריאזיס, לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs ו/או PUVA ו/או Psoralen | 12/01/2017 | עור ומין | Psoriasis | |
| דלקת מפרקים פסוריאטית (Psoriatic arthritis), לאחר כישלון טיפולי או חוסר סבילות לטיפול בתרופות השייכות למשפחת ה-DMARDs. | 15/01/2015 | ראומטולוגיה | Psoriatic arthritis |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
