Quest for the right Drug
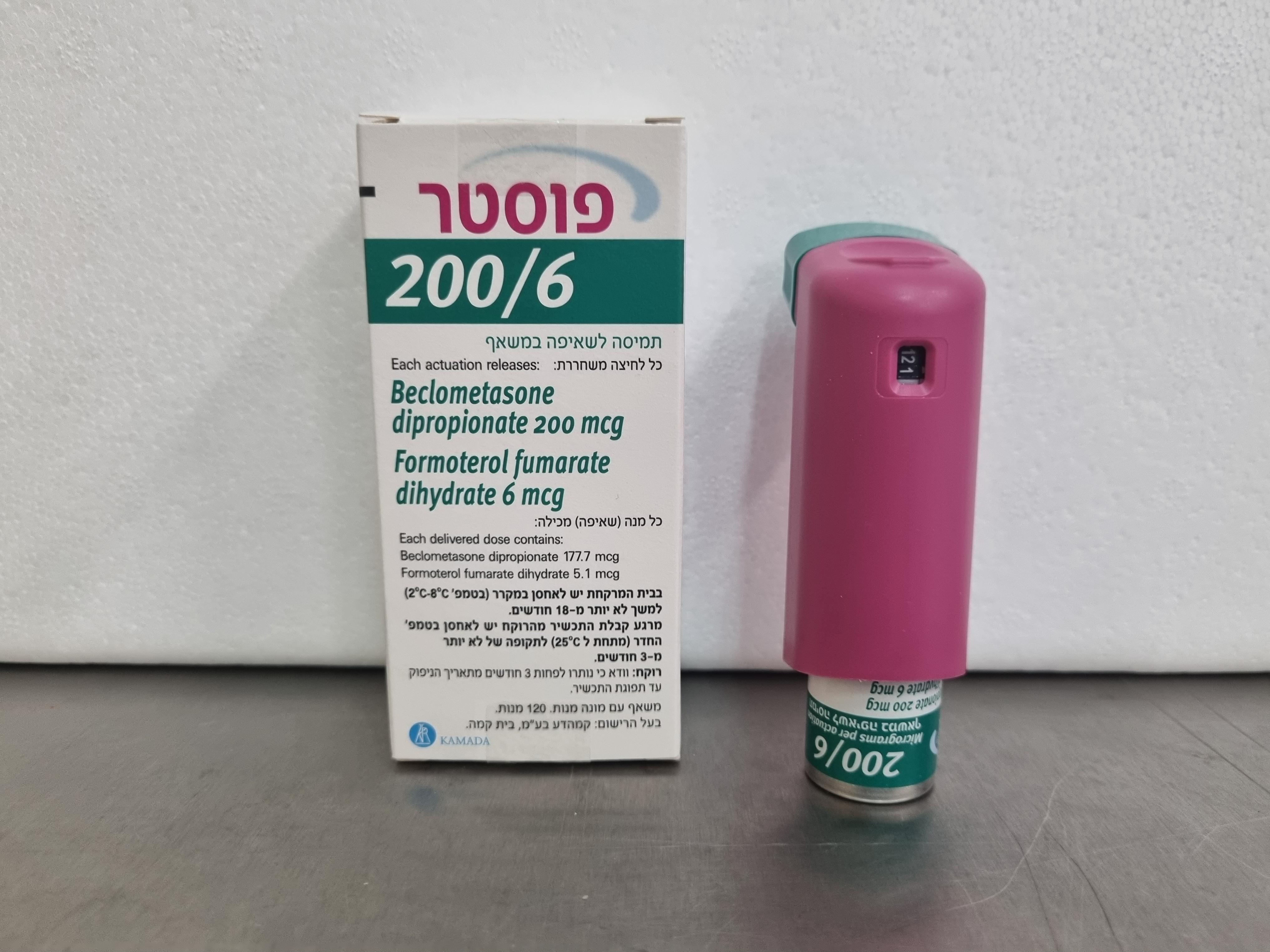
פוסטר 200/6 FOSTER 200/6 (BECLOMETASONE DIPROPIONATE ANHYDROUS, FORMOTEROL FUMARATE DIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
אין פרטים : PRESSURISED SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs for obstructive airway diseases; Adrenergics, inhalants ATC-code: R03 AK08. Mechanisms of action and pharmacodynamic effects Foster 200/6 contains beclometasone dipropionate and formoterol. These two actives have different modes of action. In common with other inhaled corticosteroids and beta2-agonist combinations, additive effects are seen in respect of reduction in asthma exacerbations. Beclometasone dipropionate Beclometasone dipropionate given by inhalation at recommended doses has a glucocorticoid antiinflammatory action within the lungs, resulting in reduced symptoms and exacerbations of asthma with less adverse effects than when corticosteroids are administered systemically. Formoterol Formoterol is a selective beta2-adrenergic agonist that produces relaxation of bronchial smooth muscle in patients with reversible airways obstruction. The bronchodilating effect sets in rapidly, within 1-3 minutes after inhalation, and has a duration of 12 hours after a single dose. Clinical efficacy and safety for Foster 200/6 In clinical trials in adults, the addition of formoterol to beclometasone dipropionate improved asthma symptoms and lung function and reduced exacerbations. In a 24-week study the effect on lung function of Foster 100/6 HFA was at least equal to that of the free combination of beclometasone dipropionate and formoterol, and exceeded that of beclometasone dipropionate alone. The efficacy of Foster 200/6 HFA, 2 puffs twice a day, was evaluated in a 12 week pivotal trial comparing the effect on lung function versus treatment with beclometasone dipropionate monotherapy in asthmatic patients not adequately controlled with previous treatment (high dose ICS or medium dose-ICS+LABAs combinations). The study demonstrated the superiority of Foster 200/6 HFA compared to BDP HFA in terms of change from baseline in the average pre-dose morning PEF (adjusted mean difference 18.53 L). In a 24 week pivotal trial the safety profile of Foster 200/6 HFA, 2 puffs twice a day, was comparable to that of an approved fixed dose combination (fluticasone/salmeterol 500/50, 1 puff twice daily). No clinically relevant effect was observed with Foster 200/6 HFA on the HPA axis after 6 months of treatment. The study showed that both Foster 200/6 µg and the approved fixed dose combination were not superior to non extrafine beclometasone dipropionate monotherapy (2000 µg/day) on the change in pre-dose morning FEV1 and percentage of complete days without asthma symptoms.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties
The systemic exposure to the active substances beclometasone dipropionate and formoterol in the fixed combination Foster have been compared to the single components.
In a pharmacokinetic study conducted in healthy subjects treated with a single dose of Foster fixed combination (4 puffs of 100/6 micrograms) or a single dose of beclometasone dipropionate CFC (4 puffs of 250 micrograms) and formoterol HFA (4 puffs of 6 micrograms), the Area Under the Curve (AUC) of beclometasone dipropionate main active metabolite (beclometasone-17-monopropionate) and its maximal plasma concentration were, respectively, 35% and 19% lower with the fixed combination than with non-extrafine beclometasone dipropionate CFC formulation, in contrast, the rate of absorption was more rapid (0.5 vs 2h) with the fixed combination compared to non-extrafine beclometasone dipropionate CFC formulation alone.
For formoterol, maximal plasma concentration was similar after administration of the fixed or the extemporary combination and the systemic exposure was slightly higher after administration of Foster than with the extemporary combination.
There was no evidence of pharmacokinetic or pharmacodynamic (systemic) interactions between beclometasone dipropionate and formoterol.
A pharmacokinetic study conducted in healthy volunteers with activated charcoal blockade demonstrated that the lung bioavailability of beclometasone-17-monopropionate in the Foster 200/6 formulation is dose proportional with respect to that of the 100/6 strength for AUC only {mean ratio between systemic bioavailability in the 200/6 formulation and in the 100/6 strength equal to 91.63 (90 % Confidence Interval: 83.79; 100.20)}. For formoterol fumarate the mean ratio between systemic bioavailability in the 200/6 formulation and in the 100/6 strength was equal to 86.15 (90% Confidence Interval: 75.94; 97.74).
In another pharmacokinetic study conducted in healthy volunteers without charcoal blockade, the systemic exposure of beclometasone-17-monopropionate in the Foster 200/6 formulation was shown to be dose proportional with respect to that of the 100/6 strength {mean ratio between systemic bioavailability in the 200/6 formulation and in the 100/6 strength equal to 89.2 (90 % Confidence Interval: 79.8; 99.7)}. The total systemic exposure of formoterol fumarate was unchanged;{mean ratio
between systemic bioavailability in the 200/6 formulation and in the 100/6 strength equal to 102.2 (90% Confidence Interval: 90.4; 115.5)}.
The use of Foster 200/6 with AeroChamber Plus® spacer increased the lung delivery of beclometasone dipropionate active metabolite beclometasone 17-monopropionate and formoterol in healthy volunteers by 25 % and 32 % respectively, while the total systemic exposure was slightly reduced for beclometasone 17-monopropionate (by 17%) and formoterol (by 17%) and increased for unchanged beclometasone dipropionate (by 54%).
Beclometasone dipropionate
Beclometasone dipropionate is a pro-drug with weak glucocorticoid receptor binding affinity that is hydrolysed via esterase enzymes to an active metabolite beclometasone-17-monopropionate which has a more potent topical anti-inflammatory activity compared with the pro-drug beclometasone dipropionate.
Absorption, distribution and biotransformation
Inhaled beclometasone dipropionate is rapidly absorbed through the lungs; prior to absorption there is extensive conversion to its active metabolite beclometasone-17-monopropionate via esterase enzymes that are found in most tissues. The systemic availability of the active metabolite arises from lung (36 %) and from gastrointestinal absorption of the swallowed dose. The bioavailability of swallowed beclometasone dipropionate is negligible however, pre-systemic conversion to beclometasone-17- monopropionate results in 41% of the dose being absorbed as the active metabolite.
There is an approximately linear increase in systemic exposure with increasing inhaled dose.
The absolute bioavailability following inhalation is approximately 2% and 62% of the nominal dose for unchanged beclometasone dipropionate and beclometasone-17-monopropionate respectively.
Following intravenous dosing, the disposition of beclometasone dipropionate and its active metabolite are characterised by high plasma clearance (150 and 120L/h respectively), with a small volume of distribution at steady state for beclometasone dipropionate (20L) and larger tissue distribution for its active metabolite (424L).
Plasma protein binding is moderately high.
Elimination
Faecal excretion is the major route of beclometasone dipropionate elimination mainly as polar metabolites. The renal excretion of beclometasone dipropionate and its metabolites is negligible. The terminal elimination half-lives are 0.5 h and 2.7 h for beclometasone dipropionate and beclometasone- 17-monopropionate respectively.
Special populations
The pharmacokinetics of beclometasone dipropionate in patients with renal or hepatic impairment has not been studied; however, as beclometasone dipropionate undergoes a very rapid metabolism via esterase enzymes present in intestinal fluid, serum, lungs and liver, to originate the more polar products beclometasone-21-monopropionate, beclometasone-17-monopropionate and beclometasone, hepatic impairment is not expected to modify the pharmacokinetics and safety profile of beclometasone dipropionate.
As beclometasone dipropionate or its metabolites were not traced in the urine, an increase in systemic exposure is not envisaged in patients with renal impairment.
Formoterol
Absorption and distribution
Following inhalation, formoterol is absorbed both from the lung and from the gastrointestinal tract.
The fraction of an inhaled dose that is swallowed after administration with a metered dose inhaler (MDI) may range between 60% and 90%. At least 65% of the fraction that is swallowed is absorbed from the gastrointestinal tract. Peak plasma concentrations of unchanged drug occur within 0.5 to 1 hours after oral administration. Plasma protein binding of formoterol is 61-64% with 34% bound to albumin. There was no saturation of binding in the concentration range attained with therapeutic doses. The elimination half-life determined after oral administration is 2-3 hours. Absorption of formoterol is linear following inhalation of 12 to 96 μg of formoterol fumarate.
Biotransformation
Formoterol is widely metabolised and the prominent pathway involves direct conjugation at the phenolic hydroxyl group. Glucuronide acid conjugate is inactive. The second major pathway involves O-demethylation followed by conjugation at the phenolic 2’-hydroxyl group. Cytochrome P450 isoenzymes CYP2D6, CYP2C19 and CYP2C9 are involved in the O-demethylation of formoterol.
Liver appears to be the primary site of metabolism. Formoterol does not inhibit CYP450 enzymes at therapeutically relevant concentrations.
Elimination
The cumulative urinary excretion of formoterol after single inhalation from a dry powder inhaler increased linearly in the 12 – 96 μg dose range. On average, 8% and 25% of the dose was excreted as unchanged and total formoterol, respectively. Based on plasma concentrations measured following inhalation of a single 120 μg dose by 12 healthy subjects, the mean terminal elimination half-life was determined to be 10 hours. The (R,R)- and (S,S)-enantiomers represented about 40% and 60% of unchanged drug excreted in the urine, respectively. The relative proportion of the two enantiomers remained constant over the dose range studied and there was no evidence of relative accumulation of one enantiomer over the other after repeated dosing.
After oral administration (40 to 80 μg), 6% to 10% of the dose was recovered in urine as unchanged drug in healthy subjects; up to 8% of the dose was recovered as the glucuronide.
A total 67% of an oral dose of formoterol is excreted in urine (mainly as metabolites) and the remainder in the faeces. The renal clearance of formoterol is 150 ml/min.
Special populations
Hepatic/Renal impairment: the pharmacokinetics of formoterol has not been studied in patients with hepatic or renal impairment; however, as formoterol is primarily eliminated via hepatic metabolism, an increased exposure can be expected in patients with severe liver cirrhosis

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2014
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
