Quest for the right Drug
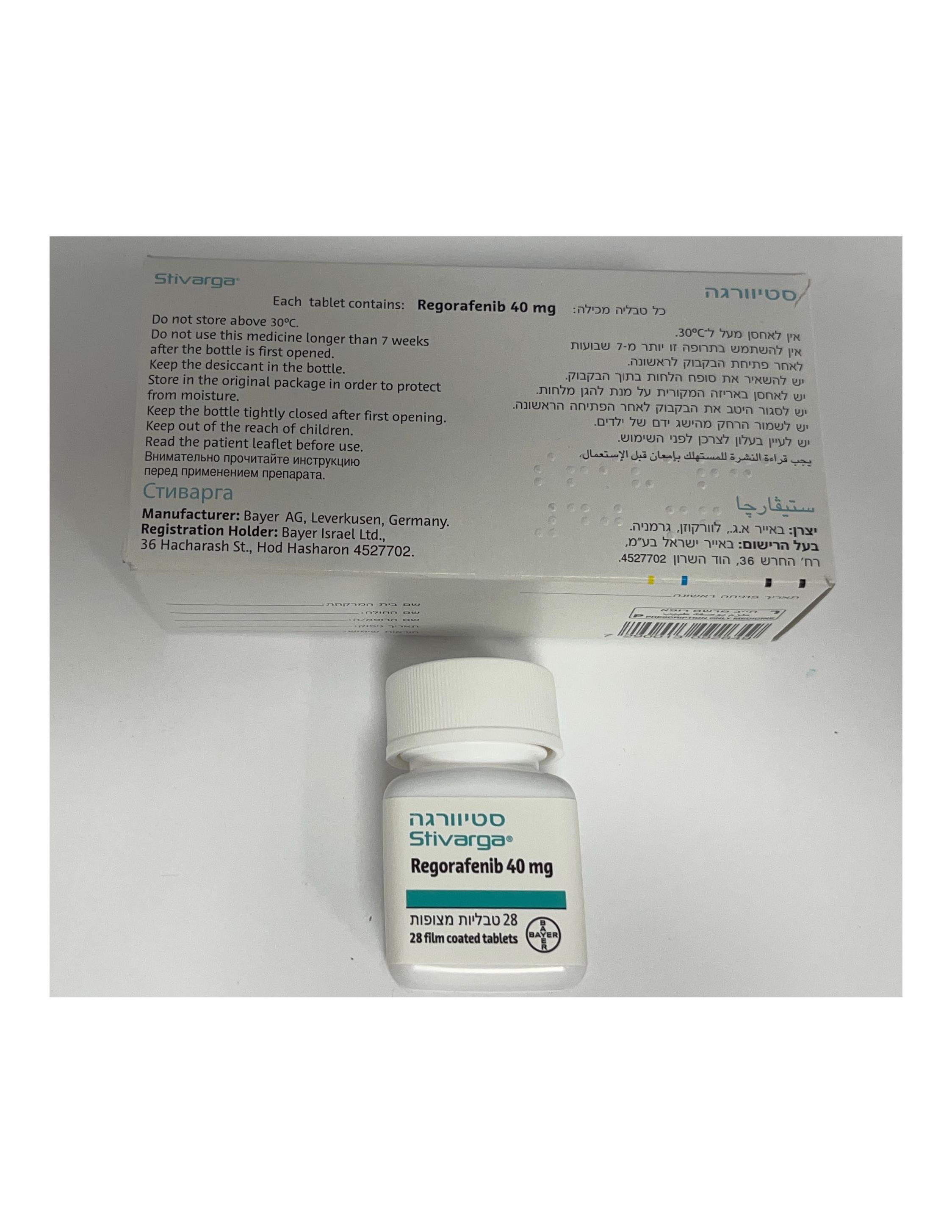
סטיוורגה STIVARGA (REGORAFENIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Stivarga should be prescribed by physicians experienced in the administration of anticancer therapy. Posology The recommended dose of regorafenib is 160 mg (4 tablets of 40 mg) taken once daily for 3 weeks followed by 1 week off therapy. This 4-week period is considered a treatment cycle. If a dose is missed, then it should be taken on the same day as soon as the patient remembers. The patient should not take two doses on the same day to make up for a missed dose. In case of vomiting after regorafenib administration, the patient should not take additional tablets. Treatment should continue as long as benefit is observed or until unacceptable toxicity occurs (see section 4.4). Patients with performance status (PS) 2 or higher were excluded from clinical studies. There is limited data in patients with PS ≥2. Posology adjustments Dose interruptions and/or dose reductions may be required based on individual safety and tolerability. Dose modifications are to be applied in 40 mg (one tablet) steps. The lowest recommended daily dose is 80 mg. The maximum daily dose is 160 mg. For recommended dose modifications and measures in case of hand-foot skin reaction (HFSR) / palmar-plantar erythrodysesthesia syndrome see Table 1. Table 1: Recommended dose modifications and measures for HFSR Skin toxicity grade Occurrence Recommended dose modification and measures Maintain dose level and immediately institute Grade 1 Any supportive measures for symptomatic relief. Decrease dose by 40 mg (one tablet) and immediately institute supportive measures. If no improvement occurs despite dose reduction, 1st occurrence interrupt therapy for a minimum of 7 days, until toxicity resolves to Grade 0-1. A dose re-escalation is permitted at the discretion of the physician. Interrupt therapy until toxicity resolves to Grade 0-1. No improvement When re-starting treatment, decrease dose by 40 mg Grade 2 within 7 days or (one tablet). 2nd occurrence A dose re-escalation is permitted at the discretion of the physician. Interrupt therapy until toxicity resolves to Grade 0-1. When re-starting treatment, decrease dose by 40 mg 3rd occurrence (one tablet). A dose re-escalation is permitted at the discretion of the physician. 4th occurrence Discontinue treatment with Stivarga permanently. Institute supportive measures immediately. Interrupt therapy for a minimum of 7 days until toxicity resolves to Grade 0-1. 1st occurrence When re-starting treatment, decrease dose by 40 mg (one tablet). A dose re-escalation is permitted at the discretion of Grade 3 the physician. Institute supportive measures immediately. Interrupt therapy for a minimum of 7 days until 2nd occurrence toxicity resolves to Grade 0-1. When re-starting treatment, decrease dose by 40 mg (one tablet). 3rd occurrence Discontinue treatment with Stivarga permanently. For recommended measures and dose modifications in case of worsening of liver function tests considered related to treatment with Stivarga see Table 2 (see also section 4.4). Table 2: Recommended measures and dose modifications in case of drug-related liver function test abnormalities Observed elevations Occurrence Recommended measures and dose modification of ALT and/or AST ≤5 times upper limit of Continue Stivarga treatment. normal (ULN) Any occurrence Monitor liver function weekly until transaminases (maximum Grade 2) return to <3 times ULN (Grade 1) or baseline. >5 times ULN Interrupt Stivarga treatment. ≤20 times ULN Monitor transaminases weekly until return to <3 times (Grade 3) ULN or baseline. 1st occurrence Restart: If the potential benefit outweighs the risk of hepatotoxicity, re-start Stivarga treatment, reduce dose by 40 mg (one tablet), and monitor liver function weekly for at least 4 weeks. Re-occurrence Discontinue treatment with Stivarga permanently. >20 times ULN Any occurrence Discontinue treatment with Stivarga permanently. (Grade 4) Discontinue treatment with Stivarga permanently. >3 times ULN Monitor liver function weekly until resolution or return (Grade 2 or higher) to baseline. with concurrent Any occurrence Exception: patients with Gilbert’s syndrome who bilirubin >2 times develop elevated transaminases should be managed as ULN per the above outlined recommendations for the respective observed elevation of ALT and/or AST. Hepatic impairment Regorafenib is eliminated mainly via the hepatic route. In clinical studies, no relevant differences in exposure, safety or efficacy were observed between patients with mild hepatic impairment (Child-Pugh A) and normal hepatic function. No dose adjustment is required in patients with mild hepatic impairment. Since only limited data are available for patients with moderate hepatic impairment (Child Pugh B), no dose recommendation can be provided. Close monitoring of overall safety is recommended in these patients (see sections 4.4 and 5.2). Stivarga is not recommended for use in patients with severe hepatic impairment (Child-Pugh C) as Stivarga has not been studied in this population. Renal impairment Available clinical data indicate similar exposure of regorafenib and its metabolites M-2 and M-5 in patients with mild, moderate or severe renal impairment compared to patients with normal renal function. No dose adjustment is required in patients with mild, moderate or severe renal impairment (see also section 5.2). Elderly population In clinical studies, no relevant differences in exposure, safety or efficacy were observed between elderly (aged 65 years and above) and younger patients (see also section 5.2). Gender In clinical studies, no relevant differences in exposure, safety or efficacy were observed between male and female patients. No dose adjustment is necessary based on gender (see also section 5.2). Ethnic differences In clinical studies, no relevant differences in exposure or efficacy were observed between patients of different ethnic groups. A higher incidence of hand foot skin reaction (HFSR) / palmar-plantar erythrodysesthesia syndrome, severe liver function test abnormalities and hepatic dysfunction was observed in Asian (in particular Japanese) patients treated with Stivarga compared with Caucasians. The Asian patients treated with Stivarga in clinical studies were primarily from East Asia (~90%). There is limited data on regorafenib in the black patient population. No dose adjustment is necessary based on ethnicity (see section 5.2). Paediatric population There is no relevant use of Stivarga in the paediatric population in the indication of metastatic colorectal cancer. The safety and efficacy of regorafenib in patients below 18 years of age in the indication gastrointestinal stromal tumours (GIST) have not been established. No data are available. There is no relevant use of Stivarga in the paediatric population in the indication of hepatocellular carcinoma. Method of administration Stivarga is for oral use. Stivarga should be taken at the same time each day. The tablets should be swallowed whole with water after a light meal that contains less than 30% fat. An example of a light (low-fat) meal would include 1 portion of cereal (about 30 g), 1 glass of skimmed milk, 1 slice of toast with jam, 1 glass of apple juice, and 1 cup of coffee or tea (520 calories, 2 g fat).

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בסרקומה מסוג GIST לחולים שמחלתם התקדמה לאחר טיפול בשני מעכבי טירוזין קינאז (Imatinib, Sunitinib). ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בסרקומה מסוג GIST לחולים שמחלתם התקדמה לאחר טיפול בשני מעכבי טירוזין קינאז |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
21.01.16 - עלון לצרכן 17.05.16 - עלון לצרכן 15.03.18 - עלון לצרכן 10.08.22 - עלון לצרכן אנגלית 10.08.22 - עלון לצרכן עברית 10.08.22 - עלון לצרכן ערבית 18.09.22 - עלון לצרכן עברית 27.02.23 - עלון לצרכן אנגלית 05.06.23 - עלון לצרכן עברית 27.02.23 - עלון לצרכן ערבית 31.07.23 - עלון לצרכן אנגלית 31.07.23 - עלון לצרכן עברית 31.07.23 - עלון לצרכן ערבית 02.08.15 - החמרה לעלון 26.09.16 - החמרה לעלון 25.04.17 - החמרה לעלון 04.12.18 - החמרה לעלון 03.02.20 - החמרה לעלון 26.04.20 - החמרה לעלון 18.11.21 - החמרה לעלון 18.09.22 - החמרה לעלון 05.06.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
סטיוורגה