Quest for the right Drug
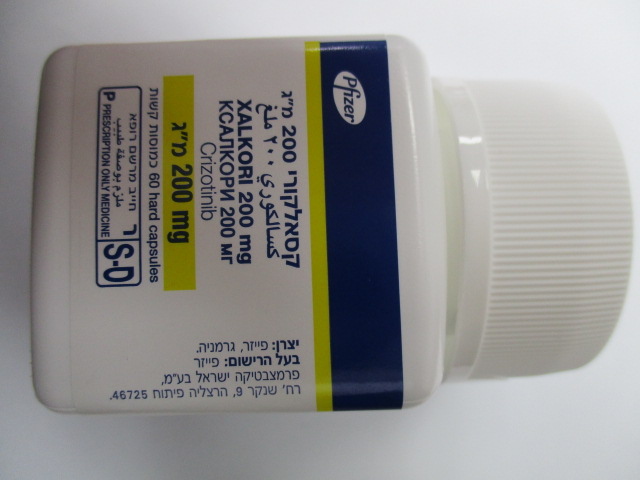
קסאלקורי 200 מ"ג XALKORI 200 MG (CRIZOTINIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The data described below reflect exposure to XALKORI in 1669 patients with ALK-positive advanced NSCLC who participated in 2 randomised Phase 3 studies (Studies 1007 and 1014) and in 2 single-arm studies (Studies 1001 and 1005), and in 53 patients with ROS1-positive advanced NSCLC who participated in single-arm Study 1001, for a total of 1722 patients (see section 5.1). These patients received a starting oral dose of 250 mg taken twice daily continuously. In Study 1014, the median duration of study treatment was 47 weeks for patients in the crizotinib arm (N=171); the median duration of treatment was 23 weeks for patients who crossed over from the chemotherapy arm to receive crizotinib treatment (N=109). In Study 1007, the median duration of study treatment was 48 weeks for patients in the crizotinib arm (N=172). For ALK-positive NSCLC patients in Studies 1001 (N=154) and 1005 (N=1063), the median duration of treatment was 57 and 45 weeks, respectively. For ROS1-positive NSCLC patients in Study 1001 (N=53), the median duration of treatment was 101 weeks. The most serious adverse reactions in 1722 patients with either ALK-positive or ROS1-positive advanced NSCLC were hepatotoxicity, ILD/pneumonitis, neutropenia, and QT interval prolongation (see section 4.4). The most common adverse reactions (≥25%) in patients with either ALK-positive or ROS1-positive NSCLC were vision disorder, nausea, diarrhoea, vomiting, oedema, constipation, elevated transaminases, fatigue, decreased appetite, dizziness, and neuropathy. The most frequent adverse reactions (≥3%, all-causality frequency) associated with dosing interruptions were neutropaenia (11%), elevated transaminases (7%), vomiting (5%), and nausea (4%). The most frequent adverse reactions (≥3%, all-causality frequency) associated with dose reductions were elevated transaminases (4%) and neutropaenia (3%). All-causality adverse events associated with permanent treatment discontinuation occurred in 302 (18%) patients of which the most frequent (≥1%) were ILD (1%) and elevated transaminases (1%). Tabulated list of adverse reactions Table 3 presents adverse reactions reported in 1722 patients with either ALK-positive or ROS1-positive advanced NSCLC who received crizotinib across 2 randomised Phase 3 studies (1007 and 1014) and 2 single-arm clinical studies (1001 and 1005) (see section 5.1). The adverse reactions listed in Table 3 are presented by system organ class and frequency categories, defined using the following convention: very common (≥1/10); common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to <1/1,000), very rare (<1/10,000), not known (cannot be estimated from the available data). Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness. Table 3. Adverse reactions reported in crizotinib clinical studies (N=1722) System organ class Very common Common Uncommon a Blood and lymphatic Neutropaenia (22%) system disorders Anaemiab (15%) Leukopeniac (15%) Metabolism and Decreased appetite Hypophosphataemia (6%) nutrition disorders (30%) Nervous system Neuropathyd (25%) disorders Dysgeusia (21%) Eye disorders Vision disordere (63%) Cardiac disorders Dizzinessf (26%) Cardiac failureh (1%) Bradycardiag (13%) Electrocardiogram QT prolonged (4%) Syncope (3%) Respiratory, thoracic Interstitial lung diseasei and mediastinal (3%) disorders Gastrointestinal Vomiting (51%) Oesophagitisk (2%) Gastrointestinal disorders Diarrhoea (54%) Dyspepsia (8%) perforationl Nausea (57%) (< 1%) Constipation (43%) Abdominal painj (21%) Hepatobiliary Elevated Blood alkaline Hepatic failure disorders transaminasesm (32%) phosphatase increased (< 1%) (7%) Skin and subcutaneous Rash (13%) Photosensitivity tissue disorders (< 1%) Renal and urinary Renal cystn (3%) Acute renal disorders Blood creatinine failure (< 1%) increasedo (8%) Renal failure (< 1%) p General disorders and Oedema (47%) administration site Fatigue (30%) conditions Investigations Blood testosterone Blood creatine q decreased (2%) phosphokinase increased (< 1%)* Event terms that represent the same medical concept or condition were grouped together and reported as a single adverse drug reaction in Table 3. Terms actually reported in the study up to the data cutoff date and contributing to the relevant adverse drug reaction are indicated in parentheses, as listed below. * Creatine phosphokinase was not a standard laboratory test in the crizotinib clinical trials. a. Neutropaenia (Febrile neutropaenia, Neutropaenia, Neutrophil count decreased). b. Anaemia (Anaemia, Haemoglobin decreased, Hypochromic anaemia). c. Leukopenia (Leukopenia, White blood cell count decreased). d. Neuropathy (Burning sensation, Dysaesthesia, Formication, Gait disturbance, Hyperaesthesia, Hypoaesthesia, Hypotonia, Motor dysfunction, Muscle atrophy, Muscular weakness, Neuralgia, Neuritis, Neuropathy peripheral, Neurotoxicity, Paraesthesia, Peripheral motor neuropathy, Peripheral sensorimotor neuropathy, Peripheral sensory neuropathy, Peroneal nerve palsy, Polyneuropathy, Sensory disturbance, Skin burning sensation). e. Vision disorder (Diplopia, Halo vision, Photophobia, Photopsia, Vision blurred, Visual acuity reduced, Visual brightness, Visual impairment, Visual perseveration, Vitreous floaters). f. Dizziness (Balance disorder, Dizziness, Dizziness postural, Presyncope). g. Bradycardia (Bradycardia, Heart rate decreased, Sinus bradycardia). h. Cardiac failure (Cardiac failure, Cardiac failure congestive, Ejection fraction decreased, Left ventricular failure, Pulmonary oedema). Across clinical studies (n=1722), 19 (1.1%) patients treated with crizotinib had any grade cardiac failure, 8 (0.5%) patients had Grade 3 or 4, and 3 (0.2%) patients had fatal outcome. i. Interstitial lung disease (Acute respiratory distress syndrome, Alveolitis, Interstitial lung disease, Pneumonitis). j. Abdominal pain (Abdominal discomfort, Abdominal pain, Abdominal pain lower, Abdominal pain upper, Abdominal tenderness). k. Oesophagitis (Oesophagitis, Oesophageal ulcer). l. Gastrointestinal perforation (Gastrointestinal perforation, Intestinal perforation, Large intestine perforation). m. Elevated transaminases (Alanine aminotransferase increased, Aspartate aminotransferase increased, Gamma-glutamyltransferase increased, Hepatic enzyme increased, Hepatic function abnormal, Liver function test abnormal, Transaminases increased). n. Renal cyst (Renal abscess, Renal cyst, Renal cyst haemorrhage, Renal cyst infection). o. Blood creatinine increased (blood creatinine increased, creatinine renal clearance decreased). p. Oedema (Face oedema, Generalised oedema, Local swelling, Localised oedema, Oedema, Oedema peripheral, Periorbital oedema). q. Blood testosterone decreased (Blood testosterone decreased, Hypogonadism, Secondary hypogonadism). Description of selected adverse reactions Hepatotoxicity Medicinal product-induced hepatotoxicity with fatal outcome occurred in 0.1% of 1722 patients treated with crizotinib across clinical studies. Concurrent elevations in ALT and/or AST ≥3 × ULN and total bilirubin ≥2 × ULN without significant elevations of alkaline phosphatase (≤2 × ULN) have been observed in less than 1% patients treated with crizotinib. Increases to Grade 3 or 4 ALT or AST elevations were observed in 187 (11%) and 95 (6%) of patients, respectively. Seventeen (1%) patients required permanent discontinuation from treatment associated with elevated transaminases, suggesting that these events were generally manageable by dosing modifications as defined in Table 2 (see section 4.2). In randomised Phase 3 Study 1014, increases to Grade 3 or 4 ALT or AST elevations were observed in 15% and 8% of patients receiving crizotinib versus 2% and 1% of patients receiving chemotherapy. In randomised Phase 3 Study 1007, increases to Grade 3 or 4 ALT or AST elevations were observed in 18% and 9% of patients receiving crizotinib and 5% and <1% of patients receiving chemotherapy. Transaminase elevations generally occurred within the first 2 months of treatment. Across studies with crizotinib in patients with either ALK-positive or ROS1-positive NSCLC, median time to onset of increased Grade 1 or 2 transaminases was 23 days. Median time to onset of increased Grade 3 or 4 transaminases was 43 days. Grade 3 and 4 transaminase elevations were generally reversible upon dosing interruption. Across studies with crizotinib in patients with either ALK-positive or ROS1-positive NSCLC (N=1722), dose reductions associated with transaminase elevations occurred in 76 (4%) patients. Seventeen (1%) patients required permanent discontinuation from treatment. Patients should be monitored for hepatotoxicity and managed as recommended in sections 4.2 and 4.4. Gastrointestinal effects Nausea (57%), diarrhoea (54%), vomiting (51%), and constipation (43%) were the most commonly reported all-causality gastrointestinal events. Most events were mild to moderate in severity. Median times to onset for nausea and vomiting were 3 days, and these events declined in frequency after 3 weeks of treatment. Supportive care should include the use of antiemetic medicinal products. Median times to onset for diarrhoea and constipation were 13 and 17 days, respectively. Supportive care for diarrhoea and constipation should include the use of standard antidiarrhoeal and laxative medicinal products, respectively. In clinical studies with crizotinib, events of gastrointestinal perforations were reported. There were reports of fatal cases of gastrointestinal perforation during post-marketing use of crizotinib (see section 4.4). QT interval prolongation Across studies in patients with either ALK-positive or ROS1-positive advanced NSCLC, QTcF (corrected QT by the Fridericia method) ≥500 msec was recorded in 34 (2.1%) of 1619 patients with at least 1 postbaseline ECG assessment and a maximum increase from baseline in QTcF ≥60 msec was observed in 79 (5.0%) of 1585 patients with a baseline and at least 1 postbaseline ECG assessment. All-causality Grade 3 or 4 Electrocardiogram QT prolonged was reported in 27 (1.6%) out of 1722 patients (see sections 4.2, 4.4, 4.5 and 5.2). In a single arm ECG substudy (see section 5.2) using blinded manual ECG measurements 11 (21%) patients had an increase from Baseline in QTcF value ≥30 to <60 msec and 1 (2%) patient had an increase from Baseline in QTcF value of ≥60 msec. No patients had a maximum QTcF ≥480 msec. The central tendency analysis indicated that the largest mean change from baseline in QTcF was 12.3 msec (95% CI 5.1-19.5 msec, least squares mean [LS] from Analysis of Variance [ANOVA]) and occurred at 6 hours post-dose on Cycle 2 Day 1. All upper limits of the 90% CI for the LS mean change from Baseline in QTcF at all Cycle 2 Day 1 time points were <20 msec. QT prolongation can result in arrhythmias and is a risk factor for sudden death. QT prolongation may clinically manifest as bradycardia, dizziness, and syncope. Electrolyte disturbances, dehydration and bradycardia may further increase the risk of QTc prolongation and thus, periodic monitoring of ECG and electrolyte levels is recommended in patients with GI toxicity (see section 4.4). Bradycardia In studies with crizotinib in patients with either ALK-positive or ROS1-positive advanced NSCLC, all-causality bradycardia was experienced by 219 (13%) of 1722 patients treated with crizotinib. Most events were mild in severity. A total of 259 (16%) of 1666 patients with at least 1 postbaseline vital sign assessment had a pulse rate <50 bpm. The use of concomitant medicinal products associated with bradycardia should be carefully evaluated. Patients who develop symptomatic bradycardia should be managed as recommended in the Dose Modification and Warnings and Precautions sections (see sections 4.2, 4.4 and 4.5). Interstitial lung disease/pneumonitis Severe, life-threatening, or fatal ILD/pneumonitis can occur in patients treated with crizotinib. Across studies in patients with either ALK-positive or ROS1-positive NSCLC (N=1722), 50 (3%) patients treated with crizotinib had any grade all-causality ILD, including 18 (1%) patients with Grade 3 or 4, and 8 (<1%) patients with fatal cases. According to an independent review committee (IRC) assessment of patients with ALK-positive NSCLC (N=1669), 20 (1.2%) patients had ILD/pneumonitis, including 10 (<1%) patients with fatal cases. These cases generally occurred within 3 months after the initiation of treatment. Patients with pulmonary symptoms indicative of ILD/pneumonitis should be monitored. Other potential causes of ILD/pneumonitis should be excluded (see sections 4.2 and 4.4). Visual effects In clinical studies with crizotinib in patients with either ALK-positive or ROS1-positive advanced NSCLC (N=1722), Grade 4 visual field defect with vision loss has been reported in 4 (0.2%) patients. Optic atrophy and optic nerve disorder have been reported as potential causes of vision loss (see section 4.4). All-causality, all grade, vision disorder, most commonly visual impairment, photopsia, vision blurred, and vitreous floaters, was experienced by 1084 (63%) of 1722 patients treated with crizotinib. Of the 1084 patients who experienced vision disorder, 95% had events that were mild in severity. Seven (0.4%) patients had temporary treatment discontinuation and 2 (0.1%) patients had a dose reduction associated with vision disorder. There were no permanent discontinuations associated with vision disorder for any of the 1722 patients treated with crizotinib. Based on the Visual Symptom Assessment Questionnaire (VSAQ-ALK), patients treated with crizotinib in Study 1007 and Study 1014 reported a higher incidence of visual disturbances compared to patients treated with chemotherapy. The onset of vision disorders generally started within the first week of medicinal product administration. The majority of patients on the crizotinib arm in randomised Phase 3 Studies 1007 and 1014 (> 50%) reported visual disturbances; which occurred at a frequency of 4 to 7 days each week, lasted up to 1 minute, and had mild or no impact (scores 0 to 3 out of a maximum score of 10) on daily activities as captured by the VSAQ-ALK questionnaire. An ophthalmology substudy using specific ophthalmic assessments at specified time points was conducted in 54 patients with NSCLC who received crizotinib 250 mg twice daily. Thirty-eight (70.4%) of the 54 patients experienced an Eye Disorders System Organ Class treatment-emergent all-causality adverse event of which 30 patients had ophthalmic examinations. Of the 30 patients, an ophthalmic abnormality of any type was reported in 14 (36.8%) patients and no ophthalmic finding was seen in 16 (42.1%) patients. The most common findings concerned slit lamp biomicroscopy (21.1%), fundoscopy (15.8%) and visual acuity (13.2%). Pre-existing ophthalmic abnormalities and concomitant medical conditions which could be contributory to ocular findings were noted in many patients, and no conclusive causal relationship to crizotinib could be determined. There were no findings related to aqueous cell count and anterior chamber aqueous flare assessment. No visual disturbances associated with crizotinib appeared to be related to changes in best corrected visual acuity, the vitreous, the retina, or the optic nerve. In patients with new onset of Grade 4 visual loss, crizotinib treatment should be discontinued and ophthalmological evaluation should be performed. Ophthalmological evaluation is recommended if vision disorder persists or worsens in severity (see sections 4.2 and 4.4). Nervous system effects All-causality neuropathy, as defined in Table 3, was experienced by 435 (25%) out of 1722 patients treated with crizotinib. Dysgeusia was also very commonly reported in these studies, and was primarily Grade 1 in severity. Renal cyst All-causality complex renal cysts were experienced by 52 (3%) of 1722 patients treated with crizotinib. Local cystic invasion beyond the kidney was observed in some patients. Periodic monitoring with imaging and urinalysis should be considered in patients who develop renal cysts. Neutropenia and leukopenia Across studies in patients with either ALK-positive or ROS1-positive advanced NSCLC (N=1722), Grade 3 or 4 neutropenia was observed in 212 (12%) patients treated with crizotinib. Median time to onset of any grade neutropenia was 89 days. Neutropenia was associated with dose reduction or permanent treatment discontinuation for 3% and <1% of patients, respectively. Less than 0.5% of patients experienced febrile neutropenia in clinical studies with crizotinib. Across studies in patients with either ALK-positive or ROS1-positive advanced NSCLC (N=1722), Grade 3 or Grade 4 leukopenia was observed in 48 (3%) patients treated with crizotinib. Median time to onset of any grade leukopenia was 85 days. Leukopenia was associated with a dose reduction for <0.5% of patients, and no patients permanently discontinued crizotinib treatment associated with leukopenia. In clinical studies of crizotinib in patients with either ALK-positive or ROS1-positive advanced NSCLC, shifts to Grade 3 or 4 decreases in leukocytes and neutrophils were observed at frequencies of 4% and 13%, respectively. Complete blood counts including differential white blood cell counts should be monitored as clinically indicated, with more frequent repeat testing if Grade 3 or 4 abnormalities are observed, or if fever or infection occurs. For patients who develop haematologic laboratory abnormalities, see section 4.2. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse event should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il/.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. התרופה תינתן לטיפול באדנוקרצינומה מתקדמת של הריאה מסוג non small cell(NSCLC) עם מוטציה שלילית ב-EGFR שהם בעלי מוטציה חיובית ב-ALK ( Anaplastic Lymphoma Kinase positive)) במהלך מחלתו יהיה החולה זכאי לטיפול בשלוש תרופות בלבד מהתרופות המפורטות להלן – Alectinib, Brigatinib, Ceritinib, Crizotinib, Lorlatinib.2. התרופה תינתן לטיפול באדנוקרצינומה מתקדמת של הריאה מסוג non small cell (NSCLC) עם מוטציה שלילית ב-EGFR שהם בעלי מוטציה חיובית מסוג ROS1. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול באדנוקרצינומה מתקדמת של הריאה מסוג non small cell(NSCLC) עם מוטציה שלילית ב-EGFR שהם בעלי מוטציה חיובית ב-ALK ( Anaplastic Lymphoma Kinase positive)) | 10/01/2012 | אונקולוגיה | ALK+ NSCLC | |
| ROS1+ NSCLC | 12/01/2017 | אונקולוגיה | ROS1 positive NSCLC |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
10/01/2012
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
