Quest for the right Drug
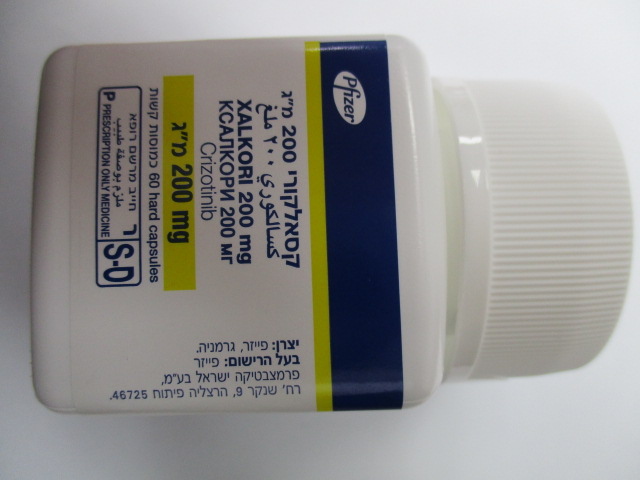
קסאלקורי 200 מ"ג XALKORI 200 MG (CRIZOTINIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Assessment of ALK and ROS1 status When assessing either ALK or ROS1 status of a patient, it is important that a well-validated and robust methodology is chosen to avoid false negative or false positive determinations. Hepatotoxicity Drug-induced hepatotoxicity (including cases with fatal outcome) has been reported in patients treated with crizotinib across clinical studies (see section 4.8). Liver function tests including ALT, AST, and total bilirubin should be monitored once a week during the first 2 months of treatment, then once a month and as clinically indicated, with more frequent repeat testing for Grades 2, 3 or 4 elevations. For patients who develop transaminase elevations, see section 4.2. Interstitial lung disease/pneumonitis Severe, life-threatening, or fatal interstitial lung disease (ILD)/pneumonitis can occur in patients treated with crizotinib. Patients with pulmonary symptoms indicative of ILD/pneumonitis should be monitored. Crizotinib treatment should be withheld if ILD/pneumonitis is suspected. Drug-induced ILD/pneumonitis should be considered in the differential diagnosis of patients with ILD-like conditions such as: pneumonitis, radiation pneumonitis, hypersensitivity pneumonitis, interstitial pneumonitis, pulmonary fibrosis, acute respiratory distress syndrome (ARDS), alveolitis, lung infiltration, pneumonia, pulmonary oedema, chronic obstructive pulmonary disease, pleural effusion, aspiration pneumonia, bronchitis, obliterative bronchiolitis, and bronchiectasis. Other potential causes of ILD/pneumonitis should be excluded, and crizotinib should be permanently discontinued in patients diagnosed with treatment-related ILD/pneumonitis (see sections 4.2 and 4.8). QT interval prolongation QTc prolongation has been observed in clinical studies in patients treated with crizotinib (see sections 4.8 and 5.2) which may lead to an increased risk for ventricular tachyarrhythmias (e.g., Torsade de Pointes) or sudden death. The benefits and potential risks of crizotinib should be considered before beginning therapy in patients with pre-existing bradycardia, who have a history of or predisposition for QTc-prolongation, who are taking antiarrhythmics or other medicinal products that are known to prolong QT-interval and in patients with relevant pre-existing cardiac disease and/or electrolyte disturbances. Crizotinib should be administered with caution in these patients and periodic monitoring of electrocardiograms (ECG), electrolytes and renal function is required. When using crizotinib, ECG and electrolytes (e.g., calcium, magnesium, potassium) should be obtained as close as possible prior to the first dose and periodic monitoring with ECGs and electrolytes is recommended, especially at the beginning of treatment in case of vomiting, diarrhoea, dehydration or impaired renal function. Correct electrolytes as necessary. If QTc increases by greater than or equal to 60 msec from baseline but QTc is < 500 msec, crizotinib should be withheld and cardiologist advice should be sought. If QTc increases to greater than or equal to 500 msec, cardiologist advice must be immediately sought. For patients who develop QTc prolongation, see sections 4.2, 4.8 and 5.2. Bradycardia All-causality bradycardia was reported in clinical studies in 13% of patients treated with crizotinib. Symptomatic bradycardia (e.g., syncope, dizziness, hypotension) can occur in patients receiving crizotinib. The full effect of crizotinib on reduction of heart rate may not develop until several weeks after start of treatment. Avoid using crizotinib in combination with other bradycardic agents (e.g., beta-blockers, non-dihydropyridine calcium channel blockers such as verapamil and diltiazem, clonidine, digoxin) to the extent possible, due to the increased risk of symptomatic bradycardia. Monitor heart rate and blood pressure regularly. Dose modification is not required in cases of asymptomatic bradycardia. For management of patients who develop symptomatic bradycardia, see Dose Modification and Undesirable Effects sections (see sections 4.2 and 4.8). Cardiac failure In clinical studies with crizotinib and during post-marketing surveillance, severe, life- threatening, or fatal adverse reactions of cardiac failure were reported (see section 4.8). Patients with or without pre-existing cardiac disorders, receiving crizotinib, should be monitored for signs and symptoms of heart failure (dyspnoea, oedema, rapid weight gain from fluid retention). Dosing interruption, dose reduction, or discontinuation should be considered as appropriate if such symptoms are observed. Neutropenia and leukopenia In clinical studies with crizotinib in patients with either ALK-positive or ROS1-positive NSCLC, Grade 3 or 4 neutropenia has been very commonly (12%) reported. Grade 3 or 4 leukopenia has been commonly (3%) reported (see section 4.8). Less than 0.5% of patients experienced febrile neutropenia in clinical studies with crizotinib. Complete blood counts including differential white blood cell counts should be monitored as clinically indicated, with more frequent repeat testing if Grade 3 or 4 abnormalities are observed, or if fever or infection occurs (see section 4.2). Gastrointestinal perforation In clinical studies with crizotinib, events of gastrointestinal perforations were reported. There were reports of fatal cases of gastrointestinal perforation during post-marketing use of crizotinib (see section 4.8). Crizotinib should be used with caution in patients at risk for gastrointestinal perforation (e.g., history of diverticulitis, metastases to the gastrointestinal tract, concomitant use of medicinal products with a recognized risk of gastrointestinal perforation). Crizotinib should be discontinued in patients who develop gastrointestinal perforation. Patients should be informed of the first signs of gastrointestinal perforations and be advised to consult rapidly in case of occurrence. Renal effects Blood creatinine increase and creatinine clearance decreased were observed in patients in clinical studies with crizotinib. Renal failure and acute renal failure were reported in patients treated with crizotinib in clinical studies and during post-marketing. Cases with fatal outcome, cases requiring haemodialysis and cases of Grade 4 hyperkalaemia were also observed. Monitoring of patients for renal function at baseline and during therapy with crizotinib is recommended, with particular attention to those who have risk factors or previous history of renal impairment (see section 4.8). Renal impairment If patients have severe renal impairment not requiring peritoneal dialysis or haemodialysis, the dose of crizotinib should be adjusted (see sections 4.2 and 5.2). Visual effects In clinical studies with crizotinib in patients with either ALK-positive or ROS1-positive NSCLC (N=1722), Grade 4 visual field defect with vision loss has been reported in 4 (0.2%) patients. Optic atrophy and optic nerve disorder have been reported as potential causes of vision loss. In patients with new onset of severe visual loss (best corrected visual acuity less than 6/60 in one or both eyes), crizotinib treatment should be discontinued (see section 4.2). Ophthalmological evaluation consisting of best corrected visual acuity, retinal photographs, visual fields, optical coherence tomography (OCT) and other evaluations as appropriate for new onset of severe visual loss, should be performed. There is insufficient information to characterise the risks of resumption of crizotinib in patients with a severe visual loss. A decision to resume crizotinib should consider the potential benefit to the patient. Ophthalmological evaluation is recommended if vision disorder persists or worsens in severity (see section 4.8). Photosensitivity Photosensitivity has been reported in patients treated with Xalkori (see section 4.8). Patients should be advised to avoid prolonged sun exposure while taking Xalkori and, when outdoors, to take protective measures (e.g., use of protective clothing and/or sunscreen). Drug-drug interactions The concomitant use of crizotinib with strong CYP3A4 inhibitors or with strong and moderate CYP3A4 inducers should be avoided (see section 4.5). The concomitant use of crizotinib with CYP3A4 substrates with narrow therapeutic indices should be avoided (see section 4.5). Avoid using crizotinib in combination with other bradycardic agents, medicinal products that are known to prolong QT interval and/or antiarrhythmics (see section 4.4 QT interval prolongation, Bradycardia, and section 4.5). Drug-food interaction Grapefruit or grapefruit juice should be avoided during treatment with crizotinib (see sections 4.2 and 4.5). Non-adenocarcinoma histology Limited information is available in patients with ALK-positive and ROS1-positive NSCLC with non-adenocarcinoma histology, including squamous cell carcinoma (SCC) (see section 5.1). Dietary sodium This medicinal product contains less than 1 mmol sodium (23 mg) per 200 mg or 250 mg capsule, that is to say essentially ‘sodium-free’.
Effects on Driving
4.7 Effects on ability to drive and use machines XALKORI has minor influence on the ability to drive and use machines. Caution should be exercised when driving or operating machines as patients may experience symptomatic bradycardia (e.g., syncope, dizziness, hypotension), vision disorder, or fatigue while taking XALKORI (see sections 4.2, 4.4 and 4.8).

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. התרופה תינתן לטיפול באדנוקרצינומה מתקדמת של הריאה מסוג non small cell(NSCLC) עם מוטציה שלילית ב-EGFR שהם בעלי מוטציה חיובית ב-ALK ( Anaplastic Lymphoma Kinase positive)) במהלך מחלתו יהיה החולה זכאי לטיפול בשלוש תרופות בלבד מהתרופות המפורטות להלן – Alectinib, Brigatinib, Ceritinib, Crizotinib, Lorlatinib.2. התרופה תינתן לטיפול באדנוקרצינומה מתקדמת של הריאה מסוג non small cell (NSCLC) עם מוטציה שלילית ב-EGFR שהם בעלי מוטציה חיובית מסוג ROS1. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול באדנוקרצינומה מתקדמת של הריאה מסוג non small cell(NSCLC) עם מוטציה שלילית ב-EGFR שהם בעלי מוטציה חיובית ב-ALK ( Anaplastic Lymphoma Kinase positive)) | 10/01/2012 | אונקולוגיה | ALK+ NSCLC | |
| ROS1+ NSCLC | 12/01/2017 | אונקולוגיה | ROS1 positive NSCLC |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
10/01/2012
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
