Quest for the right Drug
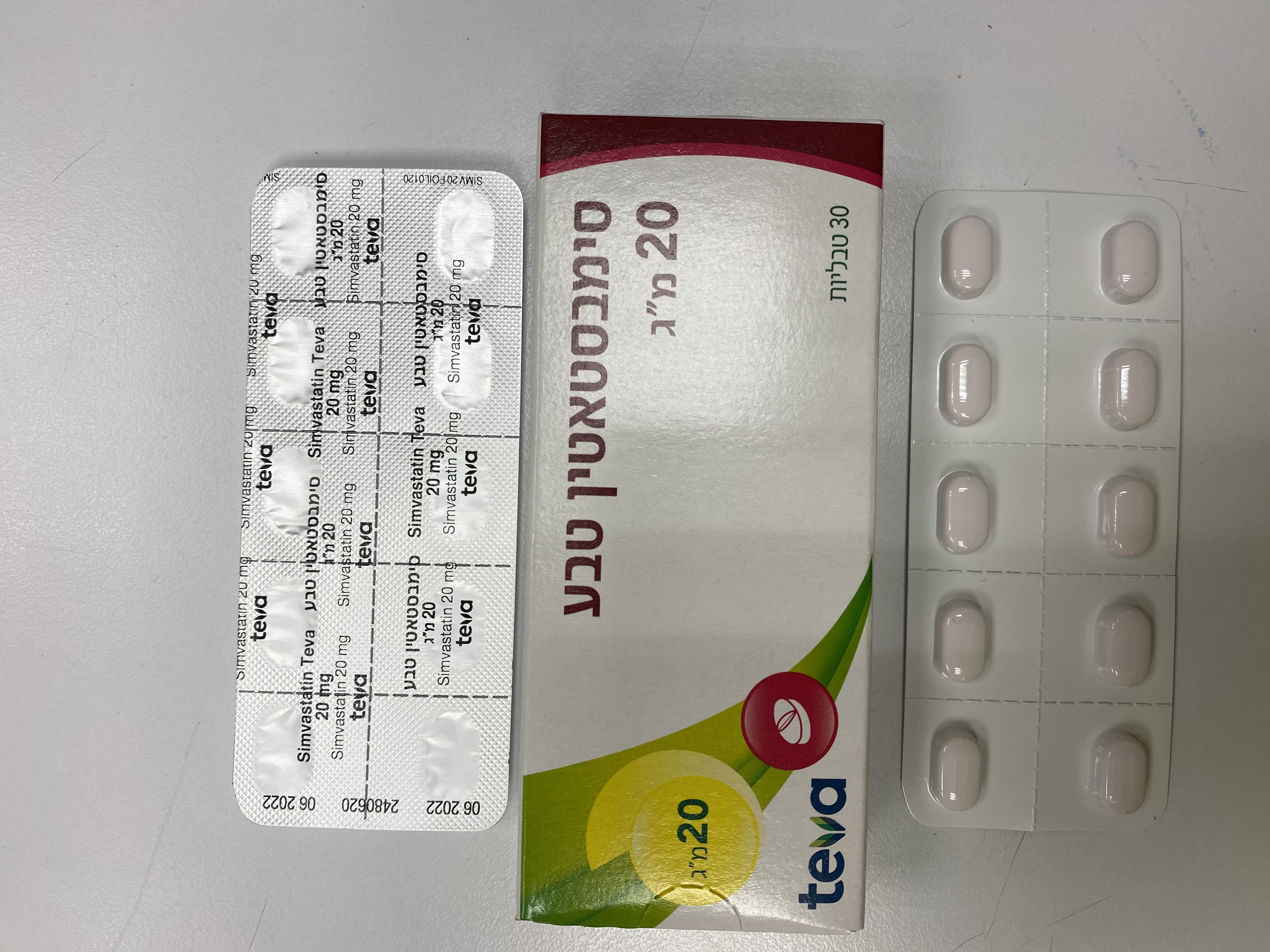
סימבסטאטין טבע 20 מ"ג SIMVASTATIN TEVA 20 MG (SIMVASTATIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: HMG-CoA reductase inhibitor. ATC Code: C10A A01. Mechanism of action After oral ingestion, simvastatin, which is an inactive lactone, is hydrolyzed in the liver to the corresponding active beta-hydroxyacid form which has a potent activity in inhibiting HMG- CoA reductase (3 hydroxy - 3 methylglutaryl CoA reductase). This enzyme catalyses the conversion of HMG-CoA to mevalonate, an early and rate- limiting step in the biosynthesis of cholesterol. Simvastatin has been shown to reduce both normal and elevated LDL-C concentrations. LDL is formed from very-low-density protein (VLDL) and is catabolised predominantly by the high affinity LDL receptor. The mechanism of the LDL-lowering effect of simvastatin may involve both reduction of VLDL-cholesterol (VLDL-C) concentration and induction of the LDL receptor, leading to reduced production and increased catabolism of LDL-C. Apolipoprotein B also falls substantially during treatment with simvastatin. In addition, simvastatin moderately increases HDL-C and reduces plasma TG. As a result of these changes the ratios of total-to HDL-C and LDL- to HDL-C are reduced. Clinical efficacy and safety High Risk of Coronary Heart Disease (CHD) or Existing Coronary Heart Disease In the Heart Protection Study (HPS), the effects of therapy with simvastatin were assessed in 20,536 patients (age 40-80 years), with or without hyperlipidaemia, and with coronary heart disease, other occlusive arterial disease or diabetes mellitus. In this study, 10,269 patients were treated with simvastatin 40 mg/day and 10,267 patients were treated with placebo for a mean duration of 5 years. At baseline, 6,793 patients (33%) had LDL-C levels below 116 mg/dL; 5,063 patients (25%) had levels between 116 mg/dL and 135 mg/dL and 8,680 patients (42%) had levels greater than 135 mg/dL. Treatment with simvastatin 40 mg/day compared with placebo significantly reduced the risk of all-cause mortality (1328 [12.9%] for simvastatin-treated patients versus 1507 [14.7 %] for patients given placebo; p = 0.0003), due to an 18 % reduction in coronary death rate (587 [5.7 %] versus 707 [6.9 %]; p = 0.0005; absolute risk reduction of 1.2%). The reduction in non- vascular deaths did not reach statistical significance. Simvastatin also decreased the risk of major coronary events (a composite endpoint comprised of non-fatal MI or CHD death) by 27% (p < 0.0001). Simvastatin reduced the need for undergoing coronary revascularization procedures (including coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) and peripheral and other non-coronary revascularization procedures by 30% (p< 0.0001) and 16% (p = 0.006), respectively. Simvastatin reduced the risk of stroke by 25% (p < 0.0001), attributable to a 30% reduction in ischemic stroke (p < 0.0001). In addition, within the subgroup of patients with diabetes, simvastatin reduced the risk of developing macrovascular complications, including peripheral revascularization procedures (surgery or angioplasty), lower limb amputations or leg ulcers by 21% (p = 0.0293). The proportional reduction in event rate was similar in each subgroup of patients studied, including those without coronary disease but who had cerebrovascular or peripheral artery disease, men and women, those aged either under or over 70 years at entry into the study, presence or absence of hypertension, and notably those with LDL cholesterol below 3.0 mmol/l at inclusion. In the Scandinavian Simvastatin Survival Study (4S), the effect of therapy with simvastatin on total mortality was assessed in 4,444 patients with CHD and baseline total cholesterol 212-309 mg/dL (5.5 - 8.0 mmol/L). In this multicenter, randomised, double-blind, placebo- controlled study, patients with angina or a previous myocardial infarction (MI) were treated with diet, standard care, and either simvastatin 20-40 mg/day (n = 2,221) or placebo (n = 2,223) for a median duration of 5.4 years. Simvastatin reduced the risk of death by 30% (absolute risk reduction of 3.3%). The risk of CHD death was reduced by 42 % (absolute risk reduction of 3.5 %). Simvastatin also decreased the risk of having major coronary events (CHD death plus hospital- verified and silent nonfatal MI) by 34%. Furthermore, simvastatin significantly reduced the risk of fatal plus nonfatal cerebrovascular events (stroke and transient ischemic attacks) by 28 %. There was no statistically significant difference between groups in non-cardiovascular mortality. The Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) evaluated the effect of treatment with simvastatin 80 mg versus 20 mg (median follow-up 6.7 yrs) on major vascular events (MVEs; defined as fatal CHD, non-fatal MI, coronary revascularization procedure, non-fatal or fatal stroke, or peripheral revascularization procedure) in 12,064 patients with a history of myocardial infarction. There was no significant difference in the incidence of MVEs between the 2 groups; simvastatin 20 mg (n = 1553; 25.7%) vs. simvastatin 80 mg (n = 1477; 24.5%); RR 0.94, 95 % CI: 0.88 to 1.01. The absolute difference in LDL-C between the two groups over the course of the study was 0.35 ± 0.01 mmol/L. The safety profiles were similar between the two treatment groups except that the incidence of myopathy was approximately 1.0 % for patients on simvastatin 80 mg compared with 0.02% for patients on 20 mg. Approximately half of these myopathy cases occurred during the first year of treatment. The incidence of myopathy during each subsequent year of treatment was approximately 0.1%. Primary Hypercholesterolaemia and Combined Hyperlipidaemia In studies comparing the efficacy and safety of simvastatin 10, 20, 40 and 80 mg daily in patients with hypercholesterolaemia, the mean reductions of LDL-C were 30, 38, 41 and 47 %, respectively. In studies of patients with combined (mixed) hyperlipidaemia on simvastatin 40 mg and 80 mg, the median reductions in triglycerides were 28 and 33% (placebo: 2%), respectively, and mean increases in HDL-C were 13 and 16 % (placebo: 3 %), respectively.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Simvastatin is an inactive lactone which is readily hydrolyzed in vivo to the corresponding beta-hydroxyacid, a potent inhibitor of HMG-CoA reductase. Hydrolysis takes place mainly in the liver; the rate of hydrolysis in human plasma is very slow. The pharmacokinetic properties have been evaluated in adults. Pharmacokinetic data in children and adolescents are not available. Absorption In man, simvastatin is well absorbed and undergoes extensive hepatic first-pass extraction. The extraction in the liver is dependent on the hepatic blood flow. The liver is the primary site of action of the active form. The availability of the beta-hydroxyacid to the systemic circulation following an oral dose of simvastatin was found to be less than 5% of the dose. Maximum plasma concentration of active inhibitors is reached approximately 1-2 hours after administration of simvastatin. Concomitant food intake does not affect the absorption. The pharmacokinetics of single and multiple doses of simvastatin showed that no accumulation of medicinal product occurred after multiple dosing. Distribution The protein binding of simvastatin and its active metabolite is >95%. Elimination Simvastatin is a substrate of CYP3A4 (see sections 4.3 and 4.5). The major metabolites of simvastatin present in human plasma are the beta-hydroxyacid and four additional active metabolites. Following an oral dose of radioactive simvastatin to man, 13% of the radioactivity was excreted in the urine and 60% in the faeces within 96 hours. The amount recovered in the faeces represents absorbed medicinal product equivalents excreted in bile as well as unabsorbed medicinal product. Following an intravenous injection of the betahydroxyacid metabolite, its half-life averaged 1.9 hours. An average of only 0.3% of the IV dose was excreted in urine as inhibitors. Simvastatin is taken up actively into the hepatocytes by the transporter OATP1B1. Simvastatin is a substrate of the efflux transporter BCRP. Special Populations SLCO1B1 polymorphism Carriers of the SLCO1B1 gene c.521T>C allele have lower OATP1B1 activity. The mean exposure (AUC) of the main active metabolite, simvastatin acid is 120% in heterozygote carriers (CT) of the C allele and 221% in homozygote (CC) carriers relative to that of patients who have the most common genotype (TT). The C allele has a frequency of 18% in the European population. In patients with SLCO1B1 polymorphism there is a risk of increased exposure of simvastatin, which may lead to an increased risk of rhabdomyolysis (see section 4.4).

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| 09/03/1999 | ליפידים | ATORVASTATIN, CERIVASTATIN, FLUVASTATIN, LOVASTATIN, PRAVASTATIN, SIMVASTATIN, ROSUVASTATIN | היפרליפידמיה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
07.03.22 - עלון לצרכן אנגלית 07.03.22 - עלון לצרכן עברית 07.03.22 - עלון לצרכן ערבית 29.01.24 - עלון לצרכן עברית 04.04.24 - עלון לצרכן אנגלית 04.04.24 - עלון לצרכן עברית 04.04.24 - עלון לצרכן ערבית 18.04.12 - החמרה לעלון 26.11.20 - החמרה לעלון 11.04.21 - החמרה לעלון 20.02.22 - החמרה לעלון 28.11.13 - החמרה לעלון 29.01.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
סימבסטאטין טבע 20 מ"ג