Quest for the right Drug
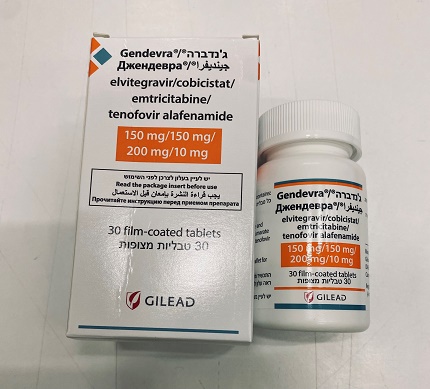
ג'נדברה GENDEVRA (COBICISTATE, ELVITEGRAVIR, EMTRICITABINE, TENOFOVIR ALAFENAMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antivirals for systemic use; antivirals for treatment of HIV infections, combinations. ATC code: J05AR18. Mechanism of action Elvitegravir is an HIV-1 integrase strand transfer inhibitor (INSTI). Integrase is an HIV-1 encoded enzyme that is required for viral replication. Inhibition of integrase prevents the integration of HIV-1 deoxyribonucleic acid (DNA) into host genomic DNA, blocking the formation of the HIV-1 provirus and propagation of the viral infection. Cobicistat is a selective, mechanism-based inhibitor of cytochrome P450 (CYP) enzymes of the CYP3A subfamily. Inhibition of CYP3A-mediated metabolism by cobicistat enhances the systemic exposure of CYP3A substrates, such as elvitegravir, where bioavailability is limited and half-life is shortened by CYP3A-dependent metabolism. Emtricitabine is a nucleoside reverse transcriptase inhibitor (NRTI) and nucleoside analogue of 2’-deoxycytidine. Emtricitabine is phosphorylated by cellular enzymes to form emtricitabine triphosphate. Emtricitabine triphosphate inhibits HIV replication through incorporation into viral DNA by the HIV reverse transcriptase (RT), which results in DNA chain-termination. Emtricitabine has activity against HIV-1, HIV-2, and HBV. Tenofovir alafenamide is a nucleotide reverse transcriptase inhibitor (NtRTI) and phosphonamidate prodrug of tenofovir (2’-deoxyadenosine monophosphate analogue). Tenofovir alafenamide is permeable into cells and due to increased plasma stability and intracellular activation through hydrolysis by cathepsin A, tenofovir alafenamide is more efficient than tenofovir disoproxil in concentrating tenofovir in peripheral blood mononuclear cells (PBMCs) (including lymphocytes and other HIV target cells) and macrophages. Intracellular tenofovir is subsequently phosphorylated to the pharmacologically active metabolite tenofovir diphosphate. Tenofovir diphosphate inhibits HIV replication through incorporation into viral DNA by the HIV RT, which results in DNA chain-termination. Tenofovir has activity against HIV-1, HIV-2, and HBV. Antiviral activity in vitro Elvitegravir, emtricitabine, and tenofovir alafenamide demonstrated synergistic antiviral activity in cell culture. Antiviral synergy was maintained for elvitegravir, emtricitabine, and tenofovir alafenamide when tested in the presence of cobicistat. The antiviral activity of elvitegravir against laboratory and clinical isolates of HIV-1 was assessed in lymphoblastoid cells, monocyte/macrophage cells, and peripheral blood lymphocytes and the 50% effective concentration (EC50) values were in the range of 0.02 to 1.7 nM. Elvitegravir displayed antiviral activity in cell culture against HIV-1 clades A, B, C, D, E, F, G, and O (EC50 values ranged from 0.1 to 1.3 nM) and activity against HIV-2 (EC50 of 0.53 nM). Cobicistat has no detectable antiviral activity against HIV-1 and does not antagonise the antiviral effects of elvitegravir, emtricitabine, or tenofovir. The antiviral activity of emtricitabine against laboratory and clinical isolates of HIV-1 was assessed in lymphoblastoid cell lines, the MAGI CCR5 cell line, and PBMCs. The EC50 values for emtricitabine were in the range of 0.0013 to 0.64 µM. Emtricitabine displayed antiviral activity in cell culture against HIV-1 clades A, B, C, D, E, F, and G (EC50 values ranged from 0.007 to 0.075 µM) and showed strain specific activity against HIV-2 (EC50 values ranged from 0.007 to 1.5 µM). The antiviral activity of tenofovir alafenamide against laboratory and clinical isolates of HIV-1 subtype B was assessed in lymphoblastoid cell lines, PBMCs, primary monocyte/macrophage cells and CD4+-T lymphocytes. The EC50 values for tenofovir alafenamide were in the range of 2.0 to 14.7 nM. Tenofovir alafenamide displayed antiviral activity in cell culture against all HIV-1 groups (M, N, and O), including subtypes A, B, C, D, E, F, and G (EC50 values ranged from 0.10 to 12.0 nM) and showed strain specific activity against HIV-2 (EC50 values ranged from 0.91 to 2.63 nM). Resistance In vitro Reduced susceptibility to elvitegravir is most commonly associated with the primary integrase mutations T66I, E92Q, and Q148R. Additional integrase mutations observed in cell culture selection included H51Y, F121Y, S147G, S153Y, E157Q, and R263K. HIV-1 with the raltegravir-selected substitutions T66A/K, Q148H/K, and N155H showed cross-resistance to elvitegravir. No in vitro resistance can be demonstrated with cobicistat due to its lack of antiviral activity. Reduced susceptibility to emtricitabine is associated with M184V/I mutations in HIV-1 RT. HIV-1 isolates with reduced susceptibility to tenofovir alafenamide express a K65R mutation in HIV-1 RT; in addition, a K70E mutation in HIV-1 RT has been transiently observed. HIV-1 isolates with the K65R mutation have low-level reduced susceptibility to abacavir, emtricitabine, tenofovir, and lamivudine. In treatment-naïve patients In a pooled analysis, genotyping was performed on plasma HIV-1 isolates from antiretroviral-naïve patients receiving Gendevra in Phase 3 studies GS-US-292-0104 and GS-US-292-0111 with HIV-1 RNA ≥ 400 copies/mL at confirmed virologic failure, Week 144, or time of early study drug discontinuation. Up to Week 144, the development of one or more primary elvitegravir, emtricitabine, or tenofovir alafenamide resistance-associated mutations was observed in HIV-1 isolates from 12 of 22 patients with evaluable genotypic data from paired baseline and Gendevra treatment-failure isolates (12 of 866 patients [1.4%]) compared with 12 of 20 treatment-failure isolates from patients with evaluable genotypic data in the E/C/F/TDF treatment group (12 of 867 patients [1.4%]). Of the HIV-1 isolates from 12 patients with resistance development in the Gendevra group, the mutations that emerged were M184V/I (n = 11) and K65R/N (n = 2) in RT and T66T/A/I/V (n = 2), E92Q (n = 4), Q148Q/R (n = 1) and N155H (n = 2) in integrase. Of the HIV-1 isolates from 12 patients with resistance development in the E/C/F/TDF group, the mutations that emerged were M184V/I (n = 9), K65R/N (n = 4), and L210W (n = 1) in RT and E92Q/V (n = 4), and Q148R (n = 2), and N155H/S (n = 3) in integrase. Most HIV-1 isolates from patients in both treatment groups who developed resistance mutations to elvitegravir developed resistance mutations to both emtricitabine and elvitegravir. In phenotypic analyses of patients in the final resistance analysis population, 7 of 22 patients (32%) had HIV-1 isolates with reduced susceptibility to elvitegravir in the Gendevra group compared with HIV-1 isolates from 7 of 20 patients (35%) in the E/C/F/TDF group, HIV-1 isolates from 8 patients (36%) had reduced susceptibility to emtricitabine in the Gendevra group compared with HIV-1 isolates from 7 patients (35%) in the E/C/F/TDF group. One patient in the Gendevra group (1 of 22 [4.5%]) and 2 patients in the E/C/F/TDF group (2 of 20 [10%]) had reduced susceptibility to tenofovir. In virologically suppressed patients Three patients with emergent HIV-1 resistance to Gendevra were identified (M184M/I; M184I+E92G; M184V+E92Q) up to Week 96 in a clinical study of virologically suppressed patients who switched from a regimen containing emtricitabine/tenofovir disoproxil and a third agent (GS-US-292-0109, n = 959). In patients co-infected with HIV and HBV In a clinical study of HIV virologically suppressed patients co-infected with chronic hepatitis B, who received Gendevra for 48 weeks (GS-US-292-1249, n = 72), 2 patients qualified for resistance analysis. In these 2 patients, no amino acid substitutions associated with resistance to any of the components of Gendevra were identified in HIV-1 or HBV. Cross-resistance in HIV-1 infected, treatment-naïve or virologically suppressed patients Elvitegravir-resistant viruses show varying degrees of cross-resistance to the INSTI raltegravir depending on the type and number of mutations. Viruses expressing the T66I/A mutations maintain susceptibility to raltegravir, while most other patterns showed reduced susceptibility to raltegravir. Viruses expressing elvitegravir or raltegravir resistance mutations maintain susceptibility to dolutegravir. Emtricitabine-resistant viruses with the M184V/I substitution were cross-resistant to lamivudine, but retained sensitivity to didanosine, stavudine, tenofovir, and zidovudine. The K65R and K70E mutations result in reduced susceptibility to abacavir, didanosine, lamivudine, emtricitabine, and tenofovir, but retain sensitivity to zidovudine. Clinical data HIV-1 infected, treatment-naïve patients In studies GS-US-292-0104 and GS-US-292-0111, patients were randomised in a 1:1 ratio to receive either Gendevra (n = 866) once daily or elvitegravir 150 mg/cobicistat 150 mg/emtricitabine 200 mg/tenofovir disoproxil (as fumarate) 245 mg (E/C/F/TDF) (n = 867) once daily. The mean age was 36 years (range 18-76), 85% were male, 57% were White, 25% were Black, and 10% were Asian. Nineteen percent of patients were identified as Hispanic/Latino. The mean baseline plasma HIV-1 RNA was 4.5 log10 copies/mL (range 1.3-7.0) and 23% had baseline viral loads > 100,000 copies/mL. The mean baseline CD4+ cell count was 427 cells/mm3 (range 0-1,360) and 13% had a CD4+ cell count < 200 cells/mm3. Gendevra demonstrated statistical superiority in achieving HIV-1 RNA < 50 copies/mL when compared to E/C/F/TDF at Week 144. The difference in percentage was 4.2% (95% CI: 0.6% to 7.8%). Pooled treatment outcomes at 48 and 144 weeks are shown in Table 3. Table 3: Pooled virologic outcomes of studies GS-US-292-0104 and GS-US-292-0111 at Weeks 48 and 144a,b Week 48 Week 144 Gendevra E/C/F/TDF Gendevra E/C/F/TDF (n = 866) (n = 867) (n = 866) (n = 867) HIV-1 RNA < 50 copies/mL 92% 90% 84% 80% Treatment difference 2.0% (95% CI: -0.7% to 4.7%) 4.2% (95% CI: 0.6% to 7.8%) HIV-1 RNA ≥ 50 copies/mLc 4% 4% 5% 4% No virologic data at Week 48 4% 6% 11% 16% or 144 window Discontinued study drug due 1% 2% 1% 3% to AE or deathd Discontinued study drug due 2% 4% 9% 11% to other reasons and last available HIV-1 RNA < 50 copies/mLe Missing data during window 1% < 1% 1% 1% but on study drug Week 48 Week 144 Gendevra E/C/F/TDF Gendevra E/C/F/TDF (n = 866) (n = 867) (n = 866) (n = 867) Proportion (%) of patients with HIV-1 RNA < 50 copies/mL by subgroup Age < 50 years 716/777 (92%) 680/753 (90%) 647/777 (83%) 602/753 (80%) ≥ 50 years 84/89 (94%) 104/114 (91%) 82/89 (92%) 92/114 (81%) Sex Male 674/733 (92%) 673/740 (91%) 616/733 (84%) 603/740 (81%) Female 126/133 (95%) 111/127 (87%) 113/133 (85%) 91/127 (72%) Race Black 197/223 (88%) 177/213 (83%) 168/223 (75%) 152/213 (71%) Non-black 603/643 (94%) 607/654 (93%) 561/643 (87%) 542/654 (83%) Baseline viral load ≤ 100,000 copies/mL 629/670 (94%) 610/672 (91%) 567/670 (85%) 537/672 (80%) > 100,000 copies/mL 171/196 (87%) 174/195 (89%) 162/196 (83%) 157/195 (81%) Baseline CD4+ cell count < 200 cells/mm3 96/112 (86%) 104/117 (89%) 93/112 (83%) 94/117 (80%) ≥ 200 cells/mm3 703/753 (93%) 680/750 (91%) 635/753 (84%) 600/750 (80%) HIV-1 RNA < 20 copies/mL 84.4% 84.0% 81.1% 75.8% Treatment difference 0.4% (95% CI: -3.0% to 3.8%) 5.4% (95% CI: 1.5% to 9.2%) E/C/F/TDF = elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate a Week 48 window was between Day 294 and 377 (inclusive); Week 144 window was between Day 966 and 1,049 (inclusive). b In both studies, patients were stratified by baseline HIV-1 RNA (≤ 100,000 copies/mL, > 100,000 copies/mL to ≤ 400,000 copies/mL, or > 400,000 copies/mL), by CD4+ cell count (< 50 cells/μL, 50-199 cells/μL, or ≥ 200 cells/μL), and by region (US or ex-US). c Includes patients who had ≥ 50 copies/mL in the Week 48 or 144 window; patients who discontinued early due to lack or loss of efficacy; patients who discontinued for reasons other than an adverse event (AE), death or lack or loss of efficacy and at the time of discontinuation had a viral value of ≥ 50 copies/mL. d Includes patients who discontinued due to AE or death at any time point from Day 1 through the time window if this resulted in no virologic data on treatment during the specified window. e Includes patients who discontinued for reasons other than an AE, death or lack or loss of efficacy; e.g., withdrew consent, loss to follow-up, etc. The mean increase from baseline in CD4+ cell count was 230 cells/mm3 in Gendevra-treated patients and 211 cells/mm3 in E/C/F/TDF-treated patients (p = 0.024) at Week 48, and 326 cells/mm3 in Gendevra-treated patients and 305 cells/mm3 in E/C/F/TDF-treated patients (p = 0.06) at Week 144. HIV-1 infected virologically suppressed patients In Study GS-US-292-0109, the efficacy and safety of switching from either efavirenz (EFV)/emtricitabine (FTC)/tenofovir disoproxil, FTC/tenofovir disoproxil plus atazanavir (boosted by either cobicistat or ritonavir), or E/C/F/TDF to Gendevra were evaluated in a randomised, open-label study of virologically suppressed (HIV-1 RNA < 50 copies/mL) HIV-1 infected adults (n = 1,436). Patients must have been stably suppressed (HIV-1 RNA < 50 copies/mL) on their baseline regimen for at least 6 months and had HIV-1 with no resistance mutations to any of the components of Gendevra prior to study entry. Patients were randomised in a 2:1 ratio to either switch to Gendevra at baseline (n = 959), or stay on their baseline antiretroviral regimen (n = 477). Patients had a mean age of 41 years (range 21-77), 89% were male, 67% were White, and 19% were Black. The mean baseline CD4+ cell count was 697 cells/mm3 (range 79-1,951). Patients were stratified by prior treatment regimen. At screening, 42% of patients were receiving FTC/tenofovir disoproxil plus atazanavir (boosted by either cobicistat or ritonavir), 32% of patients were receiving E/C/F/TDF, and 26% of patients were receiving EFV/FTC/tenofovir disoproxil. Switching from a tenofovir disoproxil-based regimen to Gendevra was superior in maintaining HIV-1 RNA < 50 copies/mL compared to staying on the baseline regimen (Table 4). Table 4: Virologic outcomes of Study GS-US-292-0109 at Weeks 48a and 96b Week 48 Week 96 Gendevra Baseline regimen Gendevra Baseline regimen (n = 959) (n = 477) (n = 959) (n = 477) HIV-1 RNA < 50 copies/mL 97% 93% 93% 89% Treatment difference 4.1% (95% CI: 1.6% to 6.7%, 3.7% (95% CI: 0.4% to 7.0%, p < 0.001c) p < 0.017c) HIV-1 RNA ≥ 50 copies/mLd 1% 1% 2% 2% No virologic data at Week 48/ 2% 6% 5% 9% Week 96 window Discontinued study drug due 1% 1% 1% 3% to AE or deathe Discontinued study drug due to other reasons and last 1% 4% 3% 6% available HIV-1 RNA < 50 copies/mLf Missing data during window 0% < 1% 1% < 1% but on study drug Proportion (%) of patients with HIV-1 RNA < 50 copies/mL by prior treatment regimen EFV/FTC/tenofovir 96% 90% 90% 86% disoproxil FTC/tenofovir disoproxil 97% 92% 92% 88% plus boosted atazanavir E/C/F/TDF 98% 97% 96% 93% EFV = efavirenz; FTC = emtricitabine; E/C/F/TDF = elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate a Week 48 window was between Day 294 and 377 (inclusive). b Week 96 window was between Day 630 and 713 (inclusive). c P-value for the superiority test comparing the percentages of virologic success was from the CMH test stratified by the prior treatment regimen (EFV/FTC/tenofovir disoproxil, FTC/tenofovir disoproxil plus boosted atazanavir, or E/C/F/TDF). d Includes patients who had ≥ 50 copies/mL in the Week 48 or Week 96 window; patients who discontinued early due to lack or loss of efficacy; patients who discontinued for reasons other than an adverse event (AE), death or lack or loss of efficacy and at the time of discontinuation had a viral value of ≥ 50 copies/mL. e Includes patients who discontinued due to AE or death at any time point from Day 1 through the time window if this resulted in no virologic data on treatment during the specified window. f Includes patients who discontinued for reasons other than an AE, death or lack or loss of efficacy; e.g., withdrew consent, loss to follow-up, etc. HIV-1 infected patients with mild to moderate renal impairment In Study GS-US-292-0112, the efficacy and safety of Gendevra were evaluated in an open-label clinical study of 242 HIV-1 infected patients with mild to moderate renal impairment (eGFRCG: 30-69 mL/min). Patients were virologically suppressed (HIV-1 RNA < 50 copies/mL) for at least 6 months before switching to Gendevra. The mean age was 58 years (range 24-82), with 63 patients (26%) who were ≥ 65 years of age. Seventy-nine percent were male, 63% were White, 18% were Black, and 14% were Asian. Thirteen percent of patients were identified as Hispanic/Latino. At baseline, 80 patients (33%) had eGFRCG < 50 mL/min and 162 patients had eGFRCG ≥ 50 mL/min. At baseline, median eGFR was 56 mL/min. The mean baseline CD4+ cell count was 664 cells/mm3 (range 126-1,813). At Week 144, 83.1% (197/237 patients) maintained HIV-1 RNA < 50 copies/mL after switching to Gendevra. In Study GS-US-292-1825, the efficacy and safety of Gendevra were evaluated in a single-arm, open-label clinical study in which 55 HIV-1 infected adults with end stage renal disease (eGFRCG < 15 mL/min) on chronic haemodialysis for at least 6 months before switching to Gendevra. Patients were virologically suppressed (HIV-1 RNA < 50 copies/mL) for at least 6 months before switching to Gendevra. The mean age was 48 years (range 23-64). Seventy-six percent were male, 82% were Black and 18% were White. Fifteen percent of patients identified as Hispanic/Latino. The mean baseline CD4+ cell count was 545 cells/mm3 (range 205-1473). At Week 48, 81.8% (45/55 patients) maintained HIV-1 RNA < 50 copies/mL after switching to Gendevra. There were no clinically significant changes in fasting lipid laboratory tests in patients who switched to Gendevra. Patients co-infected with HIV and HBV In open-label Study GS-US-292-1249, the efficacy and safety of Gendevra were evaluated in adult patients co-infected with HIV-1 and chronic hepatitis B. Sixty-nine of the 72 patients were on prior tenofovir disoproxil-containing antiretroviral therapy. At the start of treatment with Gendevra, the 72 patients had been HIV-suppressed (HIV-1 RNA < 50 copies/mL) for at least 6 months with or without suppression of HBV DNA and had compensated liver function. The mean age was 50 years (range 28-67), 92% of patients were male, 69% were White, 18% were Black, and 10% were Asian. The mean baseline CD4+ cell count was 636 cells/mm3 (range 263-1,498). Eighty-six percent of patients (62/72) were HBV suppressed (HBV DNA < 29 IU/mL) and 42% (30/72) were HBeAg positive at baseline. Of the patients who were HBeAg positive at baseline, 1/30 (3.3%) achieved seroconversion to anti-HBe at Week 48. Of the patients who were HBsAg positive at baseline, 3/70 (4.3%) achieved seroconversion to anti-HBs at Week 48. At Week 48, 92% of patients (66/72) maintained HIV-1 RNA < 50 copies/mL after switching to Gendevra. The mean change from baseline in CD4+ cell count at Week 48 was -2 cells/mm3. Ninety-two percent (66/72 patients) had HBV DNA < 29 IU/mL using missing = failure analysis at Week 48. Of the 62 patients who were HBV suppressed at baseline, 59 remained suppressed and 3 had missing data. Of the 10 patients who were not HBV suppressed at baseline (HBV DNA ≥ 29 IU/mL), 7 became suppressed, 2 remained detectable, and 1 had missing data. There are limited clinical data on the use of Gendevra in HIV/HBV co-infected patients who are treatment-naïve. Changes in measures of bone mineral density In studies in treatment-naïve patients, Gendevra was associated with smaller reductions in bone mineral density (BMD) compared to E/C/F/TDF as measured by DXA analysis of hip (mean change: −0.8% versus −3.4%, p < 0.001) and lumbar spine (mean change: −0.9% versus −3.0%, p < 0.001) after 144 weeks of treatment. Improvements in BMD were noted at 96 weeks after switching to Gendevra from a tenofovir disoproxil-containing regimen compared to maintaining the tenofovir disoproxil-containing regimen. Changes in measures of renal function In studies in treatment-naïve patients, Gendevra was associated with a lower impact on renal safety parameters (as measured after 144 weeks treatment by estimated glomerular filtration rate by Cockcroft-Gault method, and urine protein to creatinine ratio and after 96 weeks treatment by urine albumin to creatinine ratio) compared to E/C/F/TDF (see also section 4.4). Through 144 weeks of treatment, no subject discontinued Gendevra due to a treatment-emergent renal adverse event compared with 12 subjects who discontinued E/C/F/TDF (p < 0.001). An improved renal safety profile was maintained through Week 96 in patients who switched to Gendevra compared with those who stayed on a tenofovir disoproxil-containing regimen. Paediatric population Study GS-US-292-0106 In Study GS-US-292-0106, the efficacy, safety, and pharmacokinetics of Gendevra were evaluated in an open-label study in HIV-1-infected, treatment-naïve adolescents between the ages of 12 to < 18 years, weighing ≥ 35 kg (n = 50) in Cohort 1, and in virologically-suppressed children between the ages of 7 to < 12 years, weighing > 25 kg (n = 52) in Cohort 2. Patients in Cohort 1 had a mean age of 15 years (range 12 to 17), were 44% male, 12% Asian, and 88% Black. At baseline, mean plasma HIV-1 RNA was 4.6 log10 copies/mL, median CD4+ cell count was 456 cells/mm3 (range: 95 to 1,110), and median CD4+% was 23% (range: 7 to 45%). Overall, 22% had baseline plasma HIV-1 RNA > 100,000 copies/mL. At Week 48, the virologic response rate to Gendevra in treatment-naïve HIV-1 infected adolescents was similar to response rates in studies of treatment-naïve HIV-1 infected adults. In patients treated with Gendevra, 92% (46/50) achieved HIV-1 RNA < 50 copies/mL. The mean increase from baseline in CD4+ cell count at Week 48 was 224 cells/mm3. Three patients had virologic failure at Week 48; there was no virologic resistance detected to Gendevra. Patients in Cohort 2 had a mean age of 10 years (range: 7 to 11), a mean baseline weight of 32 kg (range: 26 to 58), were 42% male, 25% Asian, and 71% Black. At baseline, median CD4+ cell count was 926 cells/mm3 (range: 336 to 1,611), and median CD4+% was 38% (range: 23 to 51%). After switching to Gendevra, 98% (51/52) of patients in Cohort 2 remained suppressed (HIV-1 RNA < 50 copies/mL) at Week 48. The mean change from baseline in CD4+ cell count and percentage at Week 48 was -66 cells/mm3 and -0.6%, respectively. One of 52 patients met the criteria for inclusion in the resistance analysis population through Week 48; no emergent resistance to Gendevra was detected through Week 48. Study GS-US-292-1515 In Study GS-US-292-1515, the efficacy and safety of Gendevra were evaluated in an open-label study in HIV-1-infected, virologically-suppressed adolescents between the ages of 12 and 18 years, weighing ≥ 35 kg (n = 50). Patients in the study had a median age of 15 years (range: 12 to 17 years), 64% were female and 98% were Black. At baseline, median CD4+ cell count was 742 cells/mm3 (range: 255 to 1,246) and median CD4+% was 34% (range: 21 to 53%). After switching to Gendevra, 90% (45/50) of patients remained suppressed (HIV-1 RNA < 50 copies/mL) at Week 48. The mean change from baseline in CD4+ cell count and percentage at Week 48 was -43 cells/mm3 and -0.1%, respectively. Five subjects had virologic failure through the end of the study; no phenotypic or genotypic resistance to Gendevra was detected.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Following oral administration with food in HIV-1 infected patients, peak plasma concentrations were observed approximately 4 hours post-dose for elvitegravir, 3 hours post-dose for cobicistat, 3 hours post-dose for emtricitabine, and 1 hour post-dose for tenofovir alafenamide. The steady-state mean Cmax, AUCtau, and Ctrough (mean ± SD) in HIV-1 infected patients, respectively, were 1.7 ± 0.39 µg/mL, 23 ± 7.5 µg•h/mL, and 0.45 ± 0.26 µg/mL for elvitegravir, which provides inhibitory quotient of ~10 (ratio of Ctrough: protein binding-adjusted IC95 for wild-type HIV-1 virus). Corresponding steady-state mean Cmax, AUCtau, and Ctrough (mean ± SD) were 1.1 ± 0.40 µg/mL, 8.3 ± 3.8 µg•h/mL, and 0.05 ± 0.13 µg/mL for cobicistat; 1.9 ± 0.5 µg/mL, 13 ± 4.5 µg•h/mL, and 0.14 ± 0.25 µg/mL for emtricitabine. Steady-state mean Cmax and AUCtau for tenofovir alafenamide were 0.16 ± 0.08 µg/mL and 0.21 ± 0.15 µg•h/mL, respectively. For elvitegravir, Cmax and AUC increased 22% and 36% with a light meal, and 56% and 91% with a high-fat meal, relative to fasting conditions. Cobicistat exposures were unaffected by a light meal and although there was a modest decrease of 24% and 18% in Cmax and AUC respectively with a high-fat meal, no difference was observed in its pharmacoenhancing effect on elvitegravir. Emtricitabine exposures were unaffected by a light or high-fat meal. Relative to fasting conditions, the administration of Gendevra with a light meal (~400 kcal, 20% fat) or high-fat meal (~800 kcal, 50% fat) did not affect overall exposures of tenofovir alafenamide to a clinically meaningful extent (approximately 15% and 18% higher AUC with a light or high-fat meal, respectively, versus fasted). Distribution Elvitegravir is 98-99% bound to human plasma proteins and binding is independent of drug concentration over the range of 1 ng/mL to 1.6 µg/mL. The mean plasma to blood drug concentration ratio was 1.37. Cobicistat is 97-98% bound to human plasma proteins and the mean plasma to blood drug concentration ratio was 2. In vitro binding of emtricitabine to human plasma proteins was < 4% and independent of concentration over the range of 0.02-200 µg/mL. At peak plasma concentration, the mean plasma to blood drug concentration ratio was ~1.0 and the mean semen to plasma drug concentration ratio was ~4.0. In vitro binding of tenofovir to human plasma proteins is < 0.7% and is independent of concentration over the range of 0.01-25 μg/mL. Ex vivo binding of tenofovir alafenamide to human plasma proteins in samples collected during clinical studies was approximately 80%. Biotransformation Elvitegravir undergoes primarily oxidative metabolism via CYP3A, and is secondarily glucuronidated via UGT1A1/3 enzymes. Following oral administration of boosted [14C]-elvitegravir, elvitegravir was the predominant species in plasma, representing ~94% of the circulating radioactivity. Aromatic and aliphatic hydroxylation or glucuronidation metabolites are present in very low levels, displaying considerably lower antiviral activity against HIV-1 and do not contribute to the overall antiviral activity of elvitegravir. Cobicistat is metabolised via CYP3A (major)- and CYP2D6 (minor)-mediated oxidation and does not undergo glucuronidation. Following oral administration of [14C]-cobicistat, 99% of circulating radioactivity in plasma was unchanged cobicistat. In vitro studies indicate that emtricitabine is not an inhibitor of human CYP enzymes. Following administration of [14C]-emtricitabine, complete recovery of the emtricitabine dose was achieved in urine (~86%) and faeces (~14%). Thirteen percent of the dose was recovered in the urine as three putative metabolites. The biotransformation of emtricitabine includes oxidation of the thiol moiety to form the 3’-sulfoxide diastereomers (~9% of dose) and conjugation with glucuronic acid to form 2’-O-glucuronide (~4% of dose). No other metabolites were identifiable. Metabolism is a major elimination pathway for tenofovir alafenamide in humans, accounting for > 80% of an oral dose. In vitro studies have shown that tenofovir alafenamide is metabolised to tenofovir (major metabolite) by cathepsin A in PBMCs (including lymphocytes and other HIV target cells) and macrophages; and by carboxylesterase-1 in hepatocytes. In vivo, tenofovir alafenamide is hydrolysed within cells to form tenofovir (major metabolite), which is phosphorylated to the active metabolite tenofovir diphosphate. In human clinical studies, a 10 mg oral dose of tenofovir alafenamide in Gendevra resulted in tenofovir diphosphate concentrations > 4-fold higher in PBMCs and > 90% lower concentrations of tenofovir in plasma as compared to a 245 mg oral dose of tenofovir disoproxil (as fumarate) in E/C/F/TDF. In vitro, tenofovir alafenamide is not metabolised by CYP1A2, CYP2C8, CYP2C9, CYP2C19, or CYP2D6. Tenofovir alafenamide is minimally metabolised by CYP3A4. Upon co-administration with the moderate CYP3A inducer probe efavirenz, tenofovir alafenamide exposure was not significantly affected. Following administration of tenofovir alafenamide, plasma [14C]-radioactivity showed a time-dependent profile with tenofovir alafenamide as the most abundant species in the initial few hours and uric acid in the remaining period. Elimination Following oral administration of [14C]-elvitegravir/ritonavir, 94.8% of the dose was recovered in faeces, consistent with the hepatobiliary excretion of elvitegravir; 6.7% of the administered dose was recovered in urine. The median terminal plasma half-life of elvitegravir following administration of E/C/F/TDF is approximately 12.9 hours. Following oral administration of [14C]-cobicistat, 86% and 8.2% of the dose were recovered in faeces and urine, respectively. The median terminal plasma half-life of cobicistat following administration of E/C/F/TDF is approximately 3.5 hours and the associated cobicistat exposures provide elvitegravir Ctrough approximately 10-fold above the protein-binding adjusted IC95 for wild-type HIV-1 virus. Emtricitabine is primarily excreted by the kidneys with complete recovery of the dose achieved in urine (approximately 86%) and faeces (approximately 14%). Thirteen percent of the emtricitabine dose was recovered in urine as three metabolites. The systemic clearance of emtricitabine averaged 307 mL/min. Following oral administration, the elimination half-life of emtricitabine is approximately 10 hours. Renal excretion of intact tenofovir alafenamide is a minor pathway with < 1% of the dose eliminated in urine. Tenofovir alafenamide is mainly eliminated following metabolism to tenofovir. Tenofovir alafenamide and tenofovir have a median plasma half-life of 0.51 and 32.37 hours, respectively. Tenofovir is eliminated from the body by the kidneys by both glomerular filtration and active tubular secretion. Pharmacokinetics in special populations Age, gender, and ethnicity No clinically relevant pharmacokinetic differences due to gender or ethnicity have been identified for cobicistat-boosted elvitegravir, cobicistat, emtricitabine, or tenofovir alafenamide. Exposures of elvitegravir, cobicistat, emtricitabine, tenofovir, and tenofovir alafenamide achieved in 24 adolescent patients aged 12 to < 18 years who received Gendevra in Study GS-US-292-0106 were similar to exposures achieved in treatment-naïve adults following administration of Gendevra (Table 5). Table 5: Pharmacokinetics of elvitegravir, cobicistat, emtricitabine, tenofovir, and tenofovir alafenamide in antiretroviral-naïve adolescents and adults Adolescents aged 12 to < 18 years, ≥ 35 kg Adults Gendevra Gendevra EVGa COBIa FTCa TAFb TFVb EVGe COBIe FTCe TAFf TFVf AUCtau 242.8 275.8 9,459. 206.4 292.6 23,840. 8,240.8 14,424. c 22,797. 11,714. (ng•h/mL (18.4 1 (71.8 (27.4 1 (25.5) (36.1)b 4 (23.9) 0 (34.7) 1 (16.6) ) (57.8) ) (33.9) ) ) Cmax 14.6 1,450. 162.2 15.2 2,229.6 1,202.4 2,265.0 121.7 2,113.1 2,056.3 (ng/mL) (20.0 3 (51.1 (26.1 (19.2) (35.0) (22.5) (46.2) (33.7) (20.2) ) (28.4) ) ) Ctau 25.0 10.0 10.6 300.8 102.4 287.3 20.6 95.2 (ng/mL) (180.0) b N/A (19.6 N/A (28.5 (81.0) d (38.9) (61.7) (85.2) (46.7) ) ) EVG = elvitegravir; COBI = cobicistat; FTC = emtricitabine; TAF = tenofovir alafenamide fumarate; TFV = tenofovir N/A = not applicable Data are presented as mean (%CV). a n = 24 adolescents. b n = 23 adolescents. c AUClast. d n = 15 adolescents. e n = 19 adults. f n = 539 (TAF) or 841 (TFV) adults. Mean exposures of elvitegravir, cobicistat, emtricitabine, tenofovir, and tenofovir alafenamide achieved in children aged 8 to < 12 years (> 25 kg; n = 23) who received Gendevra in study GS-US-292-0106 were higher (20 to 80%) than the mean exposures achieved in adults (Table 6). Table 6: Pharmacokinetics of elvitegravir, cobicistat, emtricitabine, tenofovir, and tenofovir alafenamide in virologically-suppressed children (aged 8 to < 12 years, > 25 kg) and adults Children aged 8 to < 12 years, > 25 kg Adults Gendevra Gendevra EVGa COBIa FTCa TAFa TFVa EVGe COBIe FTCe TAFf TFVf AUCtau 33,813. 15,890. 20,629. 332.9 440.2 9,459. 206.4 292.6 d 22,797. 11,714. (ng•h/mL 9 7 2 (20.9 1 (71.8 (27.4 b c b 0 (34.7) 1 (16.6) ) (57.8) (51.7) (18.9) (44.8) ) (33.9) ) ) Cmax 26.1 1,450. 162.2 15.2 3,055.2 2,079.4 3,397.4 313.3 2,113.1 2,056.3 (ng/mL) (20.8 3 (51.1 (26.1 (38.7) (46.7) (27.0) (61.2) (33.7) (20.2) ) (28.4) ) ) Ctau 15.1 10.6 370.0 96.0 114.9 287.3 20.6 95.2 (ng/mL) N/A (24.9 N/A (28.5 (118.5) (168.7) (24.1) (61.7) (85.2) (46.7) ) ) EVG = elvitegravir; COBI = cobicistat; FTC = emtricitabine; TAF = tenofovir alafenamide fumarate; TFV = tenofovir N/A = not applicable Data are presented as mean (%CV). a n = 23 children. b n = 22 children. c n = 20 children. d AUClast. e n = 19 adults. f n = 539 (TAF) or 841 (TFV) adults. Renal impairment No clinically relevant differences in elvitegravir, cobicistat, tenofovir alafenamide, or tenofovir pharmacokinetics were observed between healthy subjects and patients with severe renal impairment (estimated CrCl ≥ 15 ml/min and but < 30 mL/min) in Phase 1 studies of cobicistat-boosted elvitegravir or of tenofovir alafenamide, respectively. In a separate Phase 1 study of emtricitabine alone, mean systemic emtricitabine exposure was higher in patients with severe renal impairment (estimated CrCl < 30 mL/min) (33.7 µg•h/mL) than in subjects with normal renal function (11.8 µg•h/mL). The safety of Gendevra has not been established in patients with severe renal impairment (estimated CrCl ≥ 15 mL/min and < 30 mL/min). Exposures of emtricitabine and tenofovir in 12 patients with end stage renal disease (estimated CrCl < 15 mL/min) on chronic haemodialysis who received Gendevra in Study GS-US-292-1825 were significantly higher than in patients with normal renal function. No clinically relevant differences in elvitegravir, cobicistat, or tenofovir alafenamide pharmacokinetics were observed in patients with end stage renal disease on chronic haemodialysis as compared to those with normal renal function. There were no new safety issues identified in patients with end stage renal disease on chronic haemodialysis receiving Gendevra (see section 4.8). There are no pharmacokinetic data on elvitegravir, cobicistat, emtricitabine or tenofovir alafenamide in patients with end stage renal disease (estimated CrCl < 15 mL/min) not on chronic haemodialysis. The safety of elvitegravir, cobicistat, emtricitabine or tenofovir alafenamide has not been established in these patients. Hepatic impairment Both elvitegravir and cobicistat are primarily metabolised and eliminated by the liver. A study of the pharmacokinetics of cobicistat-boosted elvitegravir was performed in non-HIV-1 infected patients with moderate hepatic impairment (Child-Pugh Class B). No clinically relevant differences in elvitegravir or cobicistat pharmacokinetics were observed between patients with moderate hepatic impairment and subjects with normal hepatic function. The effect of severe hepatic impairment (Child-Pugh Class C) on the pharmacokinetics of elvitegravir or cobicistat has not been studied. The pharmacokinetics of emtricitabine have not been studied in patients with hepatic impairment; however, emtricitabine is not significantly metabolised by liver enzymes, so the impact of liver impairment should be limited. Clinically relevant changes in the pharmacokinetics of tenofovir alafenamide or its metabolite tenofovir were not observed in patients with mild or moderate hepatic impairment. In patients with severe hepatic impairment, total plasma concentrations of tenofovir alafenamide and tenofovir are lower than those seen in subjects with normal hepatic function. When corrected for protein binding, unbound (free) plasma concentrations of tenofovir alafenamide in severe hepatic impairment and normal hepatic function are similar. Hepatitis B and/or hepatitis C virus co-infection The pharmacokinetics of emtricitabine and tenofovir alafenamide have not been fully evaluated in patients co-infected with hepatitis B and/or C virus. Limited data from population pharmacokinetic analysis (n = 24) indicated that hepatitis B and/or C virus infection had no clinically relevant effect on the exposure of boosted elvitegravir. Pregnancy and postpartum The results reported from a prospective study (IMPAACT P1026s) showed that treatment with cobicistat and elvitegravir-containing regimens during pregnancy results in lower elvitegravir and cobicistat exposures (Table 7). Table 7: Changes in pharmacokinetic parameters from the IMPAACT P1026s study for elvitegravir and cobicistat in women receiving cobicistat and elvitegravir-containing regimens during the second and third trimesters of pregnancy compared to paired postpartum data Comparison to paired Mean % change of elvitegravir Mean % change of cobicistat postpartum data, n pharmacokinetic parametersa pharmacokinetic parametersa AUC24 Cmax C24 AUC24 Cmax C24 2T/PP, n = 14 ↓ 24%b ↓ 8% ↓ 81%b ↓ 44% b ↓ 28% b ↓ 60%b 3T/PP, n = 24 ↓ 44%b ↓ 28% b ↓ 89%b ↓ 59% b ↓ 38% b ↓ 76%b 2T = second trimester; 3T = third trimester; PP =postpartum a paired comparisons b P<0.10 compared with postpartum

פרטי מסגרת הכללה בסל
א.התרופה האמורה תינתן לטיפול בנשאי HIV.ב.מתן התרופה ייעשה לפי מרשם של מנהל מרפאה לטיפול באיידס, במוסד רפואי שהמנהל הכיר בו כמרכז AIDS.ג. משטר הטיפול בתרופה יהיה כפוף להנחיות המנהל, כפי שיעודכנו מזמן לזמן על פי המידע העדכני בתחום הטיפול במחלה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| . התרופה האמורה תינתן לטיפול בנשאי HIV |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
17.04.18 - עלון לצרכן 03.12.20 - עלון לצרכן 22.11.21 - עלון לצרכן אנגלית 22.11.21 - עלון לצרכן עברית 20.12.21 - עלון לצרכן ערבית 19.09.22 - עלון לצרכן אנגלית 19.09.22 - עלון לצרכן עברית 10.10.22 - עלון לצרכן ערבית 03.01.23 - עלון לצרכן אנגלית 03.01.23 - עלון לצרכן עברית 04.01.23 - עלון לצרכן ערבית 01.04.24 - עלון לצרכן אנגלית 01.04.24 - עלון לצרכן עברית 01.04.24 - עלון לצרכן ערבית 25.12.18 - החמרה לעלון 17.01.19 - החמרה לעלון 14.03.19 - החמרה לעלון 01.08.19 - החמרה לעלון 23.11.20 - החמרה לעלון 01.11.21 - החמרה לעלון 22.11.21 - החמרה לעלון 19.09.22 - החמרה לעלון 03.01.23 - החמרה לעלון 01.04.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ג'נדברה