Quest for the right Drug
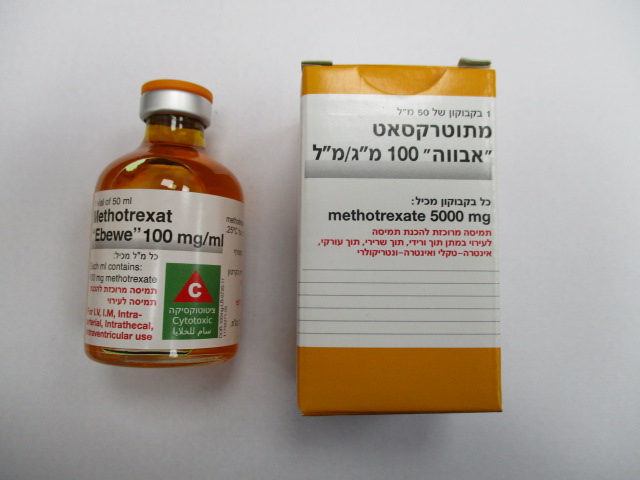
מתוטרקסאט " אבווה " 100 מ"ג/מ"ל METHOTREXAT "EBEWE" 100 MG/ML (METHOTREXATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-עורקי, תוך-ורידי, תוך חדרי, תוך-שדרתי : I.M, INTRA-ARTERIAL, I.V, INTRA VENTRICULAR, INTRATHECAL
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Methotrexate must be used only by doctors experienced in tumour therapy with sufficient experience in methotrexate treatment. Incorrect use of methotrexate can cause severe undesirable effects, which may be fatal. Medical personnel and patients must be given clear instructions. Toxicity During the treatment with methotrexate, the patients must be closely monitored due to the possible severe toxic reactions (which may be fatal) so that any signs of toxicity can be quickly recognised. The patients must be informed of the possible risks and benefits of methotrexate therapy (including the early signs and symptoms of toxicity). Furthermore, they must be instructed to see a doctor immediately if signs of toxicity become apparent and regarding the required monitoring of signs of toxicity, including regular lab tests. Discontinuation of methotrexate does not always lead to a full regression of the undesirable effects that have occurred. A prerequisite for treatment with methotrexate is that methotrexate serum levels can be determined. The discharge of methotrexate from pathological accumulations in body cavities such as ascites or intrapleural effusions (called "third space") will be slow, which leads to a prolonged plasma elimination half-life period and unexpected toxicity. If at all possible, the fluid accumulations must be removed by puncture prior to methotrexate therapy. Blood and lymphatic system Methotrexate can suppress haematopoiesis, causing anaemia, aplastic anaemia, pancytopenia, leukopenia, neutropenia and/or thrombocytopenia. First signs of these life-threatening complications may be: fever, sore throat, ulcerations of the oral mucosa, flu-like complaints, severe feeling of exhaustion, nosebleeds and skin haemorrhage. Methotrexate therapy should only be continued in the treatment of neoplastic diseases if the potential benefits outweigh the risk of severe myelosuppression. There are reports about megaloblastic anaemias, mainly during long-term therapy in older patients. Methotrexate must not be used if a peptic ulcer or ulcerative colitis is present (see section 4.3). With respect to the condition after the treatment with medicinal products with cumulative myelotoxicity and radiotherapy involving the bone marrow, attention must be paid to a limited bone-marrow reserve. This can lead to increased bone marrow susceptibility towards methotrexate therapy with increased suppression of the haematopoietic system. In longer-lasting methotrexate therapies, it may be necessary to carry out bone marrow biopsies. In acute lymphoblastic leukaemia, methotrexate may cause pain in the upper left quadrant (perisplenitis due to the destruction of the leukaemia cells). Hepatic function Due to its potentially hepatotoxic effects it is recommended that no additional hepatotoxic or potentially hepatotoxic medicinal products are used during methotrexate therapy. Furthermore, alcohol should be avoided, or alcohol consumption decreased significantly. Methotrexate can cause acute hepatitis and chronic, possibly fatal, hepatotoxicity (fibrosis, cirrhosis), but generally only after extended use. Acute increases of liver enzymes are observed frequently. These are usually temporary and asymptomatic and not preliminary signs of subsequent hepatic disease. Methotrexate caused a reactivation of hepatitis B or an exacerbation of hepatitis C infections, which were fatal in some cases. Some cases of hepatitis B reactivation appeared after discontinuation of methotrexate. Clinical and laboratory investigations should be performed to be able to evaluate an existing liver disease in patients who have a history of hepatitis B or C infection. This may result in methotrexate treatment being incompatible with some patients. If other inactive, chronic infections are present, such as herpes zoster, or tuberculosis, special caution is advised due to a possible activation. Increased caution is generally required in patients with insulin-dependent diabetes mellitus as liver cirrhosis without an intermittent increase in transaminases may develop in individual cases during methotrexate therapy. Renal function Because of the delayed methotrexate elimination, the methotrexate therapy should be performed with increased caution and at a low dosage in patients with impaired renal function. During methotrexate therapy, renal function may deteriorate, with an increase in certain lab values (creatinine, urea, and uric acid in serum), which may lead to acute kidney failure with oliguria/anuria. This is likely to be caused by precipitation of methotrexate and its metabolites in the renal tubules. Conditions leading to dehydration, such as vomiting, diarrhoea, stomatitis, may increase the toxicity of methotrexate due to increased levels of the active substance. In these cases, supportive treatment should be introduced, and the suspension of methotrexate should be considered until the symptoms have disappeared. Gastrointestinal disorders If ulcerative stomatitis or diarrhoea, haematemesis, black stool or blood in the stool (melaena) occur, the therapy must be suspended as haemorrhagic enteritis and fatalities due to perforation of the intestine may occur otherwise. Nervous system In case of patients with previous cranial radiotherapy, there have been reports of leukoencephalopathy after intravenous administration of methotrexate. Chronic leukoencephalopathy was also observed in patients who had received a repeated high- dose methotrexate therapy with calcium folinate rescue without previous cranial radiotherapy. There is evidence that the combined use of cranial irradiation together with intrathecal administration of methotrexate increases the incidence of leukoencephalopathy (see also section 4.8). Progressive multifocal leukoencephalopathy (PML) Cases of progressive multifocal leukoencephalopathy (PML) have been reported in patients receiving methotrexate, usually in combination with other immunosuppressants. PML can be fatal and should be considered in the differential diagnosis in immunosuppressed patients with newly occurring or worsening neurological symptoms. After intrathecal administration of methotrexate, patients should be monitored for signs of neurotoxicity (damage to the nervous system, such as meningitis, transient or permanent paralysis, or encephalopathy). Cases of severe neurological undesirable effects, ranging from headache to paralysis, coma and stroke-like episodes, have been reported predominantly in children and adolescents who received intrathecal methotrexate in combination with IV cytarabine. A temporary acute neurological syndrome was also observed during high dose methotrexate therapy, which can manifest e.g. through behavioural anomalies, focal sensory motor symptoms (including temporary blindness) and abnormal reflexes. The exact cause is unknown. Lung function Particular caution is required in case of patients with impaired pulmonary function. Pulmonary complications, pleural effusion, alveolitis or pneumonitis, with symptoms such as dry tickly cough, fever, general malaise, cough, thoracic pain, dyspnoea, hypoxaemia and infiltrates in the chest X-rays or a non-specific pneumonia occurring during the methotrexate therapy, may indicate potentially dangerous and possibly fatal injury. Lung biopsies revealed different findings (e.g. interstitial oedema, mononuclear infiltrates or non-necrotising granuloma). If these complications are suspected, treatment with methotrexate must be suspended at once and a careful examination to rule out infections, tumours etc. is required. Methotrexate-induced lung diseases may occur acutely at any time during the therapy; they were not always fully reversible and have been reported with doses as low as 7.5 mg/week. Pulmonary alveolar bleeding may also be linked to vasculitis and other comorbidities. An immediate examination should be considered to confirm the diagnosis if pulmonary alveolar bleeding is suspected. Skin and subcutaneous tissue disorders There are reports about the onset of severe, sometimes fatal, skin reactions, such as the Stevens-Johnson syndrome and toxic epidermal necrolysis (Lyell syndrome) after single or continuous administration of methotrexate. Psoriatic lesions may deteriorate through ultraviolet irradiation during concomitant methotrexate therapy. Radiation-induced dermatitis and sunburns can re-appear during methotrexate administration (recall reactions). Immune system Opportunistic infections, including pneumocystis jirovecii pneumonia, may occur during methotrexate therapy and may be fatal. If a patient should present with pulmonary symptoms, the possibility of pneumocystis jirovecii pneumonia should be considered. Because of its potential effects on the immune system, methotrexate may distort vaccination and test results (immunological test methods used to collect data on immune reaction). Vaccinations carried out during methotrexate therapy may be ineffective. Due to the higher risk of infection no vaccinations with live vaccines must be performed during methotrexate treatment. Methotrexate should be used with particular caution in patients with florid infections. Methotrexate is contraindicated for patients with immunodeficiency syndromes that are obvious or confirmed by laboratory tests. Furthermore, care should be taken when administering methotrexate if the patients are exposed to the viruses that cause chickenpox and herpes zoster. Neoplasms In patients with fast-growing tumours, methotrexate may, like other cytostatic medicinal products, induce tumour lysis syndrome. Suitable supportive and pharmacological measures may prevent or mitigate this complication. There are occasional reports of the occurrence of malignant lymphoma during the administration of low doses of methotrexate, which regressed in some cases after discontinuation of methotrexate therapy. In the event of lymphoma, the first step should therefore be to suspend the methotrexate therapy and to only initiate a suitable therapy if the lymphoma does not regress. In a more recent study, no increased incidence of the occurrence of lymphoma during methotrexate treatment could be determined. The use of high-dose regimens in the therapy of neoplastic diseases outside of the approved indications is investigative; a therapeutic benefit has not been proven for this. Musculoskeletal and connective tissue disorders In radiotherapy during the administration of methotrexate, the risk of soft tissue or bone necrosis may be increased. Folic acid supplementation Folate deficiency conditions may increase methotrexate toxicity (see section 4.5). The administration of folic or folinic acid may reduce the toxicity of methotrexate (gastrointestinal symptoms, stomatitis, alopecia, and increase in liver enzymes). Before taking folic acid preparations, vitamin B12 levels should be checked, as folate administration may mask vitamin B12 deficiency, especially in adults over 50 years of age. Recommended medical check-ups and safety measures Patients receiving methotrexate treatment must be closely monitored in order to immediately determine the toxic effects. The following tests should be carried out prior to initiating therapy: − complete blood count with differential blood count, − liver enzymes (ALAT [GPT], ASAT [GOT], AP), bilirubin, − serum albumin, − kidney retention parameters (if necessary with creatinine clearance) − hepatitis serology (A, B, C) − rule out the possibility of tuberculosis, if required − chest X-ray, if required. Pulmonary function tests may be beneficial if lung disease (e.g. interstitial pneumonia) is suspected, especially if corresponding reference values from the initial examination are available. Depending on the dosage or the applied therapy protocol, frequent checks of methotrexate serum levels are necessary, in particular during and after high-dose therapy with methotrexate (see also section 4.9). The adjustment of methotrexate dose and implementing suitable rescue measures can significantly reduce the toxicity and potential mortality of methotrexate treatment. Patients suffering from pleural effusions, ascites, obstruction in the gastrointestinal tract, previous cisplatin therapy, dehydration, decreased urine pH or impaired renal function, are particularly at risk of developing increased or only slowly decreasing methotrexate levels and must be monitored particularly closely. Some patients may also have delayed methotrexate elimination without the recognisable causes listed above. It is important to identify these patients within 48 hours of therapy as the methotrexate toxicity may be irreversible otherwise. After methotrexate therapy with a dose of 100 mg/m2 BSA or more, calcium folinate rescue therapy must be carried out. Depending on the methotrexate dose and the infusion duration, different calcium folinate doses are required to protect the normal tissue from serious toxic undesirable effects. Adequate calcium folinate rescue therapy must be initiated within 42 to 48 hours of methotrexate therapy. Monitoring of methotrexate levels should therefore take place at least after 24, 48 and 72 hours and should, if necessary, be continued in order to determine how long the calcium folinate rescue therapy must be continued. During the therapy with methotrexate, complete blood count monitoring with differential blood count, including platelet and leukocyte counts, must take place (daily to weekly). Prior to initiating combination therapy including high-dose methotrexate, the leukocyte and platelet counts should be above the minimum values stated in the respective protocol (leukocytes 1,000 to 1,500/µl, platelets 50,000 to 100,000/µl). The nadir for circulating leukocytes, neutrophil granulocytes, and platelets usually appears 5‒13 days after intravenous application of methotrexate (with a rebound after 14‒28 days). Leukocytes and neutrophil granulocytes sometimes show two nadirs, with the first at 4‒7 days, and the second after 12‒21 days, followed by a rebound. Hepatic and renal function tests as well as urine tests should be carried out in regular intervals. In 13–20% of patients undergoing methotrexate therapy, a temporary 2 to 3 fold increase in transaminases can be observed. This is usually no reason to change the dose regimen. Prolonged anomalies in liver enzymes and/or decreased serum albumin levels may, however, be signs of severe hepatotoxicity. In the event of a prolonged increase in liver enzymes, a dose reduction or suspension of the therapy must be considered. In patients with prolonged hepatic impairment, methotrexate must be discontinued in any case. Enzyme determination does not allow for a reliable prognosis of the development of liver injury that would be identifiable by morphological means, i.e. even with normal transaminase levels, hepatic fibrosis and less frequently hepatic cirrhosis, that can only be identified by histological examination. Renal function may deteriorate due to use of methotrexate. Creatinine, urea and electrolyte monitoring, especially in high-dose therapy with methotrexate, are recommended on Days 2 and 3 to detect any impending methotrexate elimination disorder at an early stage. Therapy with methotrexate may lead to acute renal failure with oliguria/anuria and an increase in creatinine levels. This is likely to be caused by precipitation of methotrexate and its metabolites in the renal tubules. It is recommended that renal function is monitored, including adequate hydration and alkalisation of the urine, as well as measuring the methotrexate levels in serum and monitoring urine elimination. If there are signs of renal impairment (e.g. pronounced undesirable effects of previous methotrexate therapy or urinary obstruction), the creatinine clearance must be determined. High-dose methotrexate therapy (methotrexate doses >100 mg/m2) should only be administered if creatinine values are within the normal range (creatinine clearance > 80 ml/min) (see section 4.3). As methotrexate is predominantly eliminated through the kidneys, increased concentrations are expected in impaired renal function, which may lead to severe undesirable effects.The dose should be reduced in case of a serum creatinine increase.During the conventional dose of methotrexate a dose reduction of 50% is recommended if the serum creatinine values are 1.2-2 mg/dl.If creatinine clearance is below 30 ml/min, methotrexate must not be administered. If serum creatinine values are over 2 mg/dl and the creatinine clearance is below 60 ml/min, the therapy is contraindicated for methotrexate doses of over 100 mg/m2 (see section 4.3). A treatment with methotrexate exceeding 100 mg/m2 should not be introduced if the urine pH value is below 7.0. Alkalisation of urine must be tested at least 24 hours before the start of methotrexate use by repeated pH monitoring (values of 6.8 or more). Within the scope of a high dose methotrexate treatment, sufficient intravenous fluid supply is absolutely required. If renal dysfunction is possible, or in borderline renal function (e.g. old age), monitoring should be performed in short intervals. This applies particularly, if additional medicinal products are administered, which adversely affect the elimination of methotrexate, cause renal damage (for example non-steroidal anti-inflammatory drugs), or may lead to dyshaematopoiesis. If risk factors, such as renal impairment including mild renal impairment, are present, concomitant administration with NSAIDs is not recommended. Concomitant administration of proton pump inhibitors and high-dose methotrexate should therefore be avoided, particularly in patients with impaired renal function. Conditions leading to dehydration, such as vomiting, diarrhoea, stomatitis, may increase the toxicity of methotrexate due to increased levels of the active substance. In these cases, administration of methotrexate should be suspended until the symptoms have stopped. An examination of the oral cavity and the throat for mucosal alterations must be performed daily. Particularly close monitoring of the patient is mandatory in cases of previous intensive radiotherapy, reduced general condition, juvenile or elderly patients. More frequent monitoring may be necessary at the beginning of treatment, at dose adjustment or during a period of higher risk of increased methotrexate levels (e.g. dehydration, impaired renal function, additional or increased administration of concomitant medicinal products such as non- steroidal anti-inflammatory drugs). Use in paediatric patients Particular caution is required if methotrexate is used in the treatment of children and adolescents. Treatment should comply with the therapy protocols that were specifically developed for children. In paediatric patients with acute lymphoblastic leukaemia (ALL), severe neurotoxicity can occur after treatment with moderately high doses (1 g/m2 BSA) of methotrexate. This is often seen as a generalised or focal epileptic seizure. In symptomatic patients, diagnostic imaging usually shows leukoencephalopathy and/or microangiopathic calcification. Use in elderly patients Particular caution is also required in elderly patients. The patients should be examined in short intervals for early signs of toxicity. The clinical pharmacology of methotrexate in the elderly has not yet been fully researched. The methotrexate dose should be adjusted to the hepatic and renal performance, which is reduced due to old age. Partially modified therapy protocols, for example for the treatment of ALL, have been developed for elderly patients (aged 55 and over). Fertility Methotrexate has been reported to cause oligospermia, dysmenorrhoea, fertility issues, and amenorrhoea in humans, during and for a short period after cessation of therapy, and to cause impaired fertility, affecting spermatogenesis and oogenesis during the period of its administration – effects that appear to be reversible on discontinuing therapy. Teratogenicity – reproductive risk Methotrexate causes embryotoxicity, abortion and foetal defects in humans. Therefore, the possible effects on reproduction, miscarriages and congenital malformations should be discussed with female patients of child-bearing age (see section 4.6). If women of child-bearing age are treated, effective contraception must be used during treatment and for at least six months after discontinuing treatment. Use in men Methotrexate may have genotoxic effects. It is therefore recommended that men treated with methotrexate do not father a child during and up to 6 months after treatment. Since treatment with methotrexate can lead to serious and possibly irreversible spermatogenesis disorders, men should seek advice about the possibility of sperm preservation before starting therapy (see section 4.6 for advice on birth control in men). This medicinal product contains 10.13 mg sodium per ml.
Effects on Driving
4.7 Effects on ability to drive and use machines Methotrexate has minor or moderate influence on the ability to drive and use machines. Since central nervous system effects, such as fatigue and vertigo may occur during treatment, the ability to drive and use machines may be impaired in individual cases. This is especially true in combination with alcohol.

שימוש לפי פנקס קופ''ח כללית 1994
Leukemias, non-hodgkin's lymphomas, breast, head and lung carcinoma, choriocarcinoma, osteogenic sarcoma. Severe psoriasis, rheumatoid arthritis unresponsive to conventional therapy, mycosis fungoides
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
