Quest for the right Drug
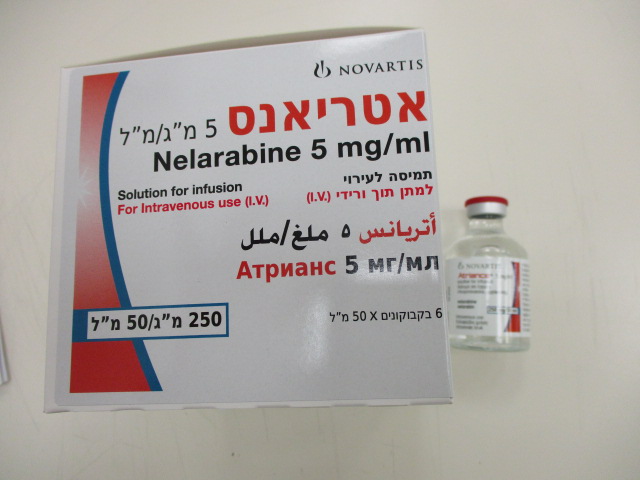
אטריאנס 5 מ"ג/מ"ל ATRIANCE 5 MG/ML (NELARABINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה לאינפוזיה : SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The safety profile from pivotal clinical studies at the recommended doses of nelarabine in adults (1,500 mg/m2) and children (650 mg/m2) is based on data from 103 adults and 84 paediatric patients respectively. The most frequently occurring adverse events were fatigue; gastrointestinal disorders; haematological disorders; respiratory disorders; nervous system disorders (somnolence, peripheral neurological disorders [sensory and motor], dizziness, hypoaesthesia, paraesthesia, headache); and pyrexia. Neurotoxicity is the dose-limiting toxicity associated with nelarabine therapy (see section 4.4). Tabulated list of adverse reactions ATR API AUG21 V1 EU SmPC 11.20 The following convention has been utilised for the classification of frequency: very common (≥1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000) and not known (cannot be estimated from the available data) Adverse reactions Adults (1,500 mg/m2) Children (650 mg/m2) N=103 N=84 Infections and infestations Infection (including but not Very common: 40 (39%) Very common: 13 (15%) limited to; sepsis, bacteraemia, pneumonia, fungal infection) Neoplasms benign, malignant and unspecified (including cysts and polyps) Tumour lysis syndrome (see Common: 1 (1%) N/A also data from compassionate use programme and non-pivotal studies) Blood and lymphatic system disorders Febrile neutropenia Very common: 12 (12%) Common: 1 (1%) Neutropenia Very common: 83 (81%) Very common: 79 (94%) Leukopenia Common: 3 (3%) Very common: 32 (38%) Thrombocytopenia Very common: 89 (86%) Very common: 74 (88%) Anaemia Very common: 102 (99%) Very common: 80 (95%) Metabolism and nutrition disorders Hypoglycaemia N/A Common: 5 (6%) Hypocalcaemia Common: 3 (3%) Common: 7 (8%) Hypomagnesaemia Common: 4 (4%) Common: 5 (6%) Hypokalaemia Common: 4 (4%) Very common: 9 (11%) Anorexia Common: 9 (9%) N/A Psychiatric disorders Confusional state Common: 8 (8%) Common: 2 (2%) Nervous system disorders Seizures (including Common: 1 (1%) Common: 5 (6%) convulsions, grand mal convulsions, status epilepticus) Amnesia Common: 3 (3%) N/A Somnolence Very common: 24 (23%) Common: 6 (7%) Peripheral neurological Very common: 22 (21%) Very common: 10 (12%) disorders (sensory and motor) Hypoesthesia Very common: 18 (17%) Common: 5 (6%) Paraesthesia Very common: 15 (15%) Common: 3 (4%) Ataxia Common: 9 (9%) Common: 2 (2%) Balance disorder Common: 2 (2%) N/A Tremor Common: 5 (5%) Common: 3 (4%) Dizziness Very common: 22 (21%) N/A ATR API AUG21 V1 EU SmPC 11.20 Adverse reactions Adults (1,500 mg/m2) Children (650 mg/m2) N=103 N=84 Headache Very common: 15 (15%) Very common: 14 (17%) Dysgeusia Common: 3 (3%) N/A Eye disorders Blurred vision Common: 4 (4%) N/A Vascular disorders Hypotension Common: 8 (8%) N/A Respiratory, thoracic and mediastinal disorders Pleural effusion Common: 10 (10%) N/A Wheezing Common: 5 (5%) N/A Dyspnoea Very common: 21 (20%) N/A Cough Very common: 26 (25%) N/A Gastrointestinal disorders Diarrhoea Very common: 23 (22%) Common: 2 (2%) Stomatitis Common: 8 (8%) Common: 1 (1%) Vomiting Very common: 23 (22%) Common: 8 (10%) Abdominal pain Common: 9 (9%) N/A Constipation Very common: 22 (21%) Common: 1 (1%) Nausea Very common: 42 (41%) Common: 2 (2%) Hepatobiliary disorders Hyperbilirubinaemia Common: 3 (3%) Common: 8 (10%) Transaminases increased N/A Very common: 10 (12%) Aspartate aminotransferase Common: 6 (6%) N/A increased Musculoskeletal and connective tissue disorders Muscle weakness Common: 8 (8%) N/A Myalgia Very common: 13 (13%) N/A Arthralgia Common: 9 (9%) Common: 1 (1%) Back pain Common: 8 (8%) N/A Pain in extremity Common: 7 (7%) Common: 2 (2%) Rhabdomyolysis, blood Rare: N/A Rare: N/A creatine phosphokinase increased (see “Post– marketing data”) Renal and urinary disorders Blood creatinine increased Common: 2 (2%) Common: 5 (6%) General disorders and administration site conditions Oedema Very common: 11 (11%) N/A Gait abnormal Common: 6 (6%) N/A Oedema peripheral Very common: 15 (15%) N/A Pyrexia Very common: 24 (23%) Common: 2 (2%) Pain Very common: 11 (11%) N/A Fatigue Very common: 51 (50%) Common: 1 (1%) Asthenia Very common: 18 (17%) Common: 5 (6%) ATR API AUG21 V1 EU SmPC 11.20 Description of selected adverse reactions Infection and infestations There was a single additional report of biopsy confirmed progressive multifocal leukoencephalopathy in the adult population. There have been reports of sometimes fatal opportunistic infections in patients receiving nelarabine therapy. Nervous system disorders There have been reports of events associated with demyelination and ascending peripheral neuropathies similar in appearance to Guillain-Barré syndrome. Two paediatric patients had fatal neurological events. Data from NCI studies/compassionate use programme and phase I studies In addition to the adverse reactions seen in the pivotal clinical studies, there are also data from 875 patients from NCI studies/compassionate use programme (694 patients) and Phase I (181 patients) studies of nelarabine. The following additional adverse reactions were seen: Neoplasms benign and malignant (including cysts and polyps) Tumour lysis syndrome – 7 cases (see sections 4.2 and 4.4) Post-marketing data Rhabdomyolysis and increased blood creatine phosphokinase have been identified during post-approval use of nelarabine. This includes spontaneous case reports as well as serious adverse events from ongoing studies. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form (https://sideeffects.health.gov.il/).

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בלוקמיה מסוג T cell Acute Lymphocytic Leukemia (T-ALL) או לימפומה מסוג T cell Lymphoblastic Lymphoma (T-LBL) העונים על כל אלה: 1. מחלתם חזרה או שהינם רפרקטורים לאחר שני משטרי טיפול קודמים. 2. מועמדים להשתלת מח עצם אלוגנאית. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בלוקמיה מסוג T cell Acute Lymphocytic Leukemia (T-ALL) או לימפומה מסוג T cell Lymphoblastic Lymphoma (T-LBL) | 01/01/2009 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
