Quest for the right Drug
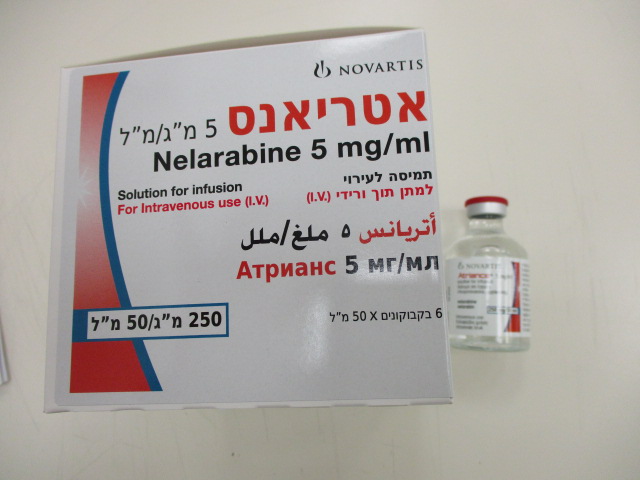
אטריאנס 5 מ"ג/מ"ל ATRIANCE 5 MG/ML (NELARABINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה לאינפוזיה : SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, antimetabolites, purine analogues, ATC code: L01B B 07 Nelarabine is a pro-drug of the deoxyguanosine analogue ara-G. Nelarabine is rapidly demethylated by adenosine deaminase (ADA) to ara-G and then phosphorylated intracellularly by deoxyguanosine kinase and deoxycytidine kinase to its 5’-monophosphate metabolite. The monophosphate metabolite is subsequently converted to the active 5’- triphosphate form, ara-GTP. Accumulation of ara-GTP in leukaemic blasts allows for preferential incorporation of ara-GTP into deoxyribonucleic acid (DNA) leading to inhibition of DNA synthesis. This results in cell death. Other mechanisms may contribute to the cytotoxic effects of nelarabine. In vitro, T-cells are more sensitive than B-cells to the cytotoxic effects of nelarabine. Clinical efficacy and data Adult clinical study in relapsed or refractory T-ALL and T-LBL In an open-label study carried out by the Cancer and Leukaemia Group B and the Southwest Oncology Group, the safety and efficacy of nelarabine were evaluated in 39 adults with T-cell acute lymphoblastic leukaemia (T-ALL) or lymphoblastic lymphoma (T-LBL). Twenty–eight of the 39 adults had relapsed or were refractory to at least two prior induction regimens and aged between 16 to 65 years of age (mean 34 years). Nelarabine at a dose of 1500 mg/m2/day was administered intravenously over two hours on days 1, 3 and 5 of a 21 day cycle. Five of the 28 patients (18%) [95% CI: 6%—37%] treated with nelarabine achieved a complete response (bone marrow blast counts ≤ 5%, no other evidence of disease, and full recovery of peripheral blood counts). A total of 6 patients (21%) [95% CI: 8%–41%] achieved a complete response with or without haematological recovery. Time to complete response in both classifications of response ranged from 2.9 to 11.7 weeks. Duration of response (in both classifications of response (n=5) ranged between 15 and 195+ weeks. Median overall survival was 20.6 weeks [95% CI: 10.4–36.4]. Survival at one year was 29% [95% CI: 12%–45%]. Paediatric clinical study in relapsed or refractory T-ALL and T-LBL In an open-label, multicenter study carried out by Childrens Oncology Group, nelarabine was administered intravenously over 1 hour for 5 days to 151 patients ≤ 21 years of age, 149 of whom had relapsed or refractory T-cell acute lymphoblastic leukaemia (T-ALL) or T-cell lymphoblastic lymphoma (T-LBL). Eighty-four (84) patients, 39 of whom had received two or more prior induction regimens and 31 whom had received one prior induction regimen, were treated with 650 mg/m2/day of nelarabine administered intravenously over 1 hour daily for 5 consecutive days repeated every 21 days. Of the 39 patients who had received two or more prior induction regimens, 5 (13%) [95% CI: 4%–27%] achieved a complete response (bone marrow blast counts ≤ 5%, no other evidence of disease, and full recovery of peripheral blood counts) and 9 (23%) [95% CI: 11%–39%] achieved complete responses with or without full haematological recovery. Duration of response in both classifications of response ranged between 4.7 and 36.4 weeks and median ATR API AUG21 V1 EU SmPC 11.20 overall survival was 13.1 weeks [95% CI: 8.7–17.4] and survival at one year was 14% [95% CI: 3%–26%]. Thirteen (42%) of the 31 patients treated with one prior induction regimen achieved a complete response overall. Nine of these 31 patients failed to respond to prior induction (refractory patients). Four (44%) of the nine refractory patients experienced a complete response to nelarabine. This medicinal product has been authorised under “exceptional circumstances”. This means that due to the rarity of the disease it has not been possible to obtain complete information on this medicinal product.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Nelarabine is a pro-drug of the deoxyguanosine analogue ara-G. Nelarabine is rapidly demethylated by adenosine deaminase (ADA) to ara-G and then phosphorylated intracellularly by deoxyguanosine kinase and deoxycytidine kinase to its 5’-monophosphate metabolite. The monophosphate metabolite is subsequently converted to the active 5’- triphosphate form, ara-GTP. Accumulation of ara-GTP in leukaemic blasts allows for preferential incorporation of ara-GTP into deoxyribonucleic acid (DNA) leading to inhibition of DNA synthesis. This results in cell death. Other mechanisms may contribute to the cytotoxic effects of nelarabine. In vitro, T-cells are more sensitive than B-cells to the cytotoxic effects of nelarabine. In a cross-study analysis using data from four Phase I studies, the pharmacokinetics of nelarabine and ara-G were characterized in patients aged less than 18 years and adult patients with refractory leukaemia or lymphoma. Absorption Adults Plasma ara-G Cmax values generally occurred at the end of the nelarabine infusion and were generally higher than nelarabine Cmax values, suggesting rapid and extensive conversion of nelarabine to ara-G. After infusion of 1,500 mg/m2 nelarabine over two hours in adult patients, mean (%CV) plasma nelarabine Cmax and AUCinf values were 13.9 µM (81%) and 13.5 µM.h (56%) respectively. Mean plasma ara-G Cmax and AUCinf values were 115 µM (16%) and 571 µM.h (30%), respectively. Intracellular Cmax for ara-GTP appeared within 3 to 25 hours on day 1. Mean (%CV) intracellular ara-GTP Cmax and AUC values were 95.6 µM (139%) and 2214 µM.h (263%) at this dose. Paediatric patients After infusion of 400 or 650 mg/m2 nelarabine over one hour in 6 paediatric patients, mean (%CV) plasma nelarabine Cmax and AUCinf values, adjusted to a 650 mg/m2 dose, were 45.0 µM (40%) and 38.0 µM.h (39%), respectively. Mean plasma ara-G Cmax and AUCinf values were 60.1 µM (17%) and 212 µM.h (18%), respectively. Distribution Nelarabine and ara-G are extensively distributed throughout the body based on combined Phase I pharmacokinetic data at nelarabine doses of 104 to 2,900 mg/m2. Specifically, for nelarabine, mean (%CV) VSS values were 115 l/m2 (159%) and 89.4 l/m2 (278%) in adult and ATR API AUG21 V1 EU SmPC 11.20 paediatric patients, respectively. For ara-G, mean VSS/F values were 44.8 l/m2 (32%) and 32.1 l/m2 (25%) in adult and paediatric patients, respectively. Nelarabine and ara-G are not substantially bound to human plasma proteins (less than 25%) in vitro, and binding is independent of nelarabine or ara-G concentrations up to 600 µM. No accumulation of nelarabine or ara-G was observed in plasma after nelarabine administration on either a daily or a day 1, 3, 5 schedule. Intracellular ara-GTP concentrations in leukaemic blasts were quantifiable for a prolonged period after nelarabine administration. Intracellular ara-GTP accumulated with repeated administration of nelarabine. On the day 1, 3, and 5 schedule, Cmax and AUC(0-t) values on day 3 were approximately 50% and 30%, respectively, greater than Cmax and AUC(0-t) values on day 1. Biotransformation The principal route of metabolism for nelarabine is O-demethylation by adenosine deaminase to form ara-G, which undergoes hydrolysis to form guanine. In addition, some nelarabine is hydrolysed to form methylguanine, which is O-demethylated to form guanine. Guanine is N- deaminated to form xanthine, which is further oxidized to yield uric acid. Elimination Nelarabine and ara-G are rapidly eliminated from plasma with a half-life of approximately 30 minutes and 3 hours, respectively. These findings were demonstrated in patients with refractory leukaemia or lymphoma given a dose of 1,500 mg/m2 nelarabine (adults) or a 650 mg/m2 (paediatrics). Combined Phase 1 pharmacokinetic data at nelarabine doses of 104 to 2,900 mg/m2 indicate that mean (%CV) clearance (Cl) values for nelarabine are 138 l/h/m2 (104%) and 125 l/h/m2 (214%) in adult and paediatric patients, respectively, on day 1 (n = 65 adults, n = 21 paediatric patients). The apparent clearance of ara-G (Cl/F) is comparable between the two groups [9.5 l/h/m2 (35%) in adult patients and 10.8 l/h/m2 (36%) in paediatric patients] on day 1. Nelarabine and ara-G are partially eliminated by the kidneys. In 28 adult patients, 24 hours after nelarabine infusion on day 1, mean urinary excretion of nelarabine and ara-G was 5.3% and 23.2% of the administered dose, respectively. Renal clearance averaged 9.0 l/h/m2 (151%) for nelarabine and 2.6 l/h/m2 (83%) for ara-G in 21 adult patients. Because the timecourse of intracellular ara-GTP was prolonged, its elimination half-life could not be accurately estimated. Paediatric population Limited clinical pharmacology data are available for patients below the age of 4 years. Combined Phase 1 pharmacokinetic data at nelarabine doses of 104 to 2,900 mg/m2 indicate that the clearance (Cl) and Vss values for nelarabine and ara-G are comparable between the two groups. Further data with respect to nelarabine and ara-G pharmacokinetics in the paediatric population are provided in other subsections. Gender ATR API AUG21 V1 EU SmPC 11.20 Gender has no effect on nelarabine or ara-G plasma pharmacokinetics. Intracellular ara-GTP Cmax and AUC(0–t) values at the same dose level were 2– to 3–fold greater on average in adult female than in adult male patients. Race The effect of race on nelarabine and ara-G pharmacokinetics has not been specifically studied. In a pharmacokinetic/pharmacodynamic cross study analysis, race had no apparent effect on nelarabine, ara-G, or intracellular ara-GTP pharmacokinetics. Renal impairment The pharmacokinetics of nelarabine and ara-G have not been specifically studied in renally impaired or haemodialysed patients. Nelarabine is excreted by the kidney to a small extent (5 to 10% of the administered dose). Ara-G is excreted by the kidney to a greater extent (20 to 30% of the administered nelarabine dose). Adults and children in clinical studies were categorized into the three groups according to renal impairment: normal with Clcr greater than 80 ml/min (n = 56), mild with Clcr equalling 50 to 80 ml/min (n = 12), and moderate with Clcr less than 50 ml/min (n = 2). The mean apparent clearance (Cl/F) of ara-G was about 7% lower in patients with mild renal impairment than in patients with normal renal function (see section 4.2). No data are available to provide a dose advice for patients with Clcr less than 50 ml/min. Elderly Age has no effect on the pharmacokinetics of nelarabine or ara-G. Decreased renal function, which is more common in the elderly, may reduce ara-G clearance (see section 4.2).

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בלוקמיה מסוג T cell Acute Lymphocytic Leukemia (T-ALL) או לימפומה מסוג T cell Lymphoblastic Lymphoma (T-LBL) העונים על כל אלה: 1. מחלתם חזרה או שהינם רפרקטורים לאחר שני משטרי טיפול קודמים. 2. מועמדים להשתלת מח עצם אלוגנאית. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בלוקמיה מסוג T cell Acute Lymphocytic Leukemia (T-ALL) או לימפומה מסוג T cell Lymphoblastic Lymphoma (T-LBL) | 01/01/2009 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
