Quest for the right Drug
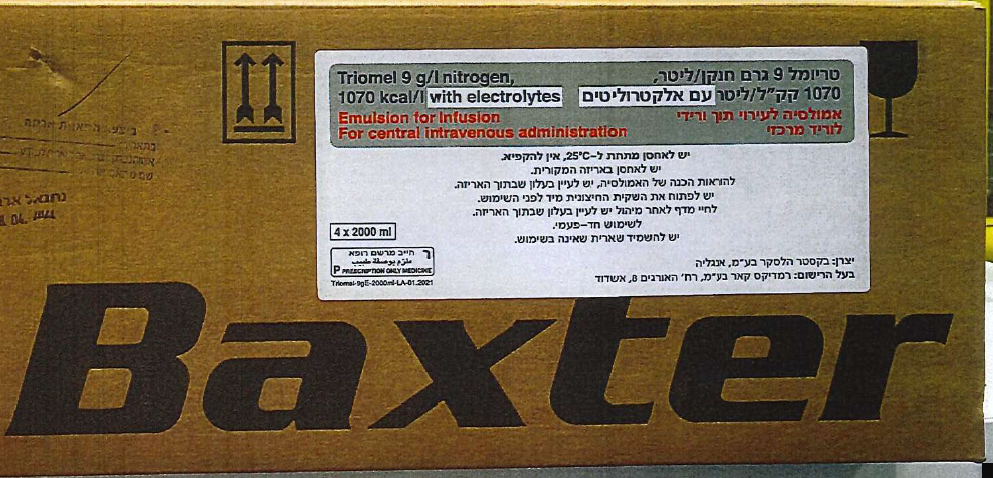
טריומל 9 גרם חנקן/ליטר, 1070 קק"ל/ליטר עם אלקטרוליטים TRIOMEL 9 G/L NITROGEN 1070 Kcal/L WITH ELECTROLYTES (ALANINE, ARGININE, ASPARTIC ACID, CALCIUM CHLORIDE DIHYDRATE, GLUCOSE MONOHYDRATE, GLUTAMIC ACID, GLYCINE, HISTIDINE, ISOLEUCINE, LEUCINE, LYSINE, MAGNESIUM CHLORIDE, METHIONINE, PHENYLALANINE, POTASSIUM CHLORIDE, PROLINE, SERINE, SODIUM ACETATE TRIHYDRATE, SODIUM GLYCEROPHOSPHATE HYDRATE, SOYA BEAN OIL REFINED + OLIVE OIL REFINED, THREONINE, TRYPTOPHAN, TYROSINE, VALINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תחליב לאינפוזיה : EMULSION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use An excessively fast administration of total parenteral nutrition (TPN) solutions may result in severe or fatal consequences. The infusion must be stopped immediately if any signs or symptoms of an allergic reaction (such as sweating, fever, chills, headache, skin rashes, or dyspnea) develop. This medicinal product contains soya-bean oil, and egg phospholipids. Soya-bean and egg proteins may cause hypersensitivity reactions. Cross-allergic reactions between soya-bean and peanut proteins have been observed. TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, contains glucose derived from corn which may cause hypersensitivity reactions in patients with allergy to corn or corn products (see section 4.3). Ceftriaxone must not be mixed or administered simultaneously with any calcium-containing IV solutions even via different infusion lines or different infusion sites. Ceftriaxone and calcium- containing solutions may be administered sequentially one after another if infusion lines at different sites are used or if the infusion lines are replaced or thoroughly flushed between infusions with physiological salt solution to avoid precipitation. In patients requiring continuous infusion with calcium-containing TPN solutions, healthcare professionals may wish to consider the use of alternative antibacterial treatments which do not carry a similar risk of precipitation. If use of ceftriaxone is considered necessary in patients requiring continuous nutrition, TPN solutions and ceftriaxone can be administered simultaneously, albeit via different infusion lines at different sites. Alternatively, infusion of TPN solution could be stopped for the period of ceftriaxone infusion, considering the advice to flush infusion lines between solutions (see sections 4.5 and 6.2). Pulmonary vascular precipitates causing pulmonary vascular embolism and respiratory distress have been reported in patients receiving parenteral nutrition. In some cases, fatal outcomes have occurred. Excessive addition of calcium and phosphate increases the risk of formation of calcium phosphate precipitates (see section 6.2). Suspected precipitate formation in the blood stream has also been reported. In addition to inspection of the solution, the infusion set and catheter should also periodically be checked for precipitates. If signs of respiratory distress occur, the infusion should be stopped and medical evaluation initiated. Do not add other medicinal products or substances to any components of the bag or to the reconstituted emulsion without first confirming their compatibility and the stability of the resulting preparation (in particular, the stability of the lipid emulsion). Formation of precipitates or destabilization of the lipid emulsion could result in vascular occlusion (see sections 6.2 and 6.6). Severe water and electrolyte equilibration disorders, severe fluid overload states, and severe metabolic disorders must be corrected before starting the infusion. Specific clinical monitoring is required when an intravenous infusion is started. Vascular-access infection and sepsis are complications that may occur in patients receiving parenteral nutrition, particularly in case of poor maintenance of catheters, immunosuppressive effects of illness or drugs. Careful monitoring of signs, symptoms, and laboratory test results for fever/chills, leukocytosis, technical complications with the access device, and hyperglycemia can help recognize early infections. Patients who require parenteral nutrition are often predisposed to infectious complications due to malnutrition and/or their underlying disease state. The occurrence of septic complications can be decreased with heightened emphasis on aseptic techniques in catheter placement and maintenance, as well as aseptic techniques in the preparation of the nutritional formula. Monitor water and electrolyte balance, serum osmolarity, serum triglycerides, acid/base balance, blood glucose, liver and kidney function tests, coagulation tests, and blood count, including platelets, throughout treatment. Elevated liver enzymes and cholestasis have been reported with similar products. Monitoring of serum ammonia should be considered if hepatic insufficiency is suspected. Metabolic complications may occur if the nutrient intake is not adapted to the patient's requirements, or the metabolic capacity of any given dietary component is not accurately assessed. Adverse metabolic effects may arise from administration of inadequate or excessive nutrients or from inappropriate composition of an admixture for a particular patient's needs. Administration of amino acid solutions may precipitate acute folate deficiency; folic acid is, therefore, recommended to be given daily. Extravasation Catheter site should be monitored regularly to identify signs of extravasation. If extravasation occurs the administration should be stopped immediately, keeping the inserted catheter or cannula in place for immediate management of the patient. If possible, aspiration should be performed through the inserted catheter/cannula in order to reduce the amount of fluid present in the tissues before removing the catheter/cannula. Depending on the extravasated product (including the product(s) being mixed with TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, if applicable) and the stage/extent of any injury, appropriate specific measures should be taken. Options for management may include non- pharmacologic, pharmacologic and/or surgical intervention. In case of large extravasation, plastic surgeon advice should be sought within the first 72 hours. The extravasation site should be monitored at least every 4 hours during the first 24 hours, then once daily. The infusion should not be restarted in the same central vein. Hepatic Insufficiency Use with caution in patients with hepatic insufficiency because of the risk of developing or worsening neurological disorders associated with hyperammonaemia. Regular clinical and laboratory tests are required, particularly liver function parameters, blood glucose, electrolytes and triglycerides. Renal Insufficiency Use with caution in patients with renal insufficiency, particularly if hyperkalaemia is present, because of the risk of developing or worsening metabolic acidosis and hyperazotemia if extra-renal waste removal is not being performed. Fluid, triglycerides and electrolyte status should be closely monitored in these patients. Hematologic Use with caution in patients with coagulation disorders and anaemia. Blood count and coagulation parameters should be closely monitored. Endocrine and Metabolism Use with caution in patients with: - Metabolic acidosis. Administration of carbohydrates is not recommended in the presence of lactic acidosis. Regular clinical and laboratory tests are required. - Diabetes mellitus. Monitor glucose concentrations, glucosuria, ketonuria and, where applicable adjust insulin dosages. - Hyperlipidaemia due to the presence of lipids in the emulsion for infusion. Regular clinical and laboratory tests are required. - Amino acid metabolism disorders. Hepatobiliary disorders Hepatobiliary disorders including cholestasis, hepatic steatosis, fibrosis and cirrhosis, possibly leading to hepatic failure, as well as cholecystitis and cholelithiasis are known to develop in some patients on parenteral nutrition. The etiology of these disorders is thought to be multifactorial and may differ between patients. Patients developing abnormal laboratory parameters or other signs of hepatobiliary disorders should be assessed early by a clinician knowledgeable in liver diseases in order to identify possible causative and contributory factors, and possible therapeutic and prophylactic interventions. Serum triglyceride concentrations and the ability of the body to remove lipids must be checked regularly. Serum triglyceride concentrations must not exceed 3 mmol/l during the infusion. If a lipid metabolism abnormality is suspected, it is recommended to measure daily serum triglyceride levels after a period of 5 to 6 hours without administering lipids. In adults, the serum must be clear in less than 6 hours after stopping the infusion containing the lipid emulsion. The next infusion must only be administered when the serum triglyceride concentrations have returned to baseline values. Fat overload syndrome has been reported with similar products. The reduced or limited ability to metabolise the lipids contained in TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, may result in a "fat overload syndrome", which may be caused by overdose; however, the signs and symptoms of this syndrome may also occur when the product is administered according to instructions (see also section 4.8). In the event of hyperglycaemia, the infusion rate of TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, must be adjusted and/or insulin administered. DO NOT ADMINISTER THROUGH A PERIPHERAL VEIN. Although there is a natural content of trace elements and vitamins in the product, the levels are insufficient to meet body requirements. Trace elements and vitamins should be added in sufficient quantities to meet individual patient requirements and to prevent deficiencies from developing. See instructions for making additions to this product. Caution should be exercised in administering TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, to patients with increased osmolarity, adrenal insufficiency, heart failure or pulmonary dysfunction. In malnourished patients, initiation of parenteral nutrition can precipitate fluid shifts resulting in pulmonary oedema and congestive heart failure, as well as a decrease in the serum concentration of potassium, phosphorus, magnesium, or water-soluble vitamins. These changes can occur within 24 to 48 hours; therefore, careful and slow initiation of parenteral nutrition is recommended together with close monitoring and appropriate adjustments of fluid, electrolytes, trace elements, and vitamins. Do not connect bags in series in order to avoid the possibility of air embolism due to residual gas contained in the primary bag. To avoid risks associated with excessively rapid infusion rates, it is recommended to use a continuous and controlled infusion. TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, must be administered with caution to patients with a tendency towards electrolyte retention. Intravenous infusion of amino acids is accompanied by increased urinary excretion of trace elements, in particular copper and zinc. This should be taken into account in the dosing of trace elements, especially during long-term intravenous nutrition. Interference with laboratory tests The lipids contained in this emulsion may interfere with the results of certain laboratory tests (see section 4.5). Special precautions in paediatrics When administered to children greater than 2 years of age, it is essential to use a bag that has a volume corresponding to the daily dosage. TRIOMEL 9 g/l nitrogen 1070 kcal/l with electrolytes, emulsion for infusion, is not suitable for use in children less than 2 years of age because: - The glucose intake is too low, leading to a low glucose/lipid ratio, - The absence of cysteine makes the amino acid profile inadequate, - Calcium is too low, - The bag volumes are not appropriate. In children greater than 2 years of age, the amount of phosphate limits the daily intakes; therefore, all macronutrients and calcium should be supplemented. Maximal infusion rate is 3.3 ml/kg/hour in children 2 to 11 years of age and 2.1 ml/kg/hour in children 12 to 18 years of age. Vitamin and trace elements supplementation is always required. Paediatric formulations must be used. Geriatric population In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Effects on Driving
4.7 Effects on ability to drive and use machines Not relevant.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
