Quest for the right Drug
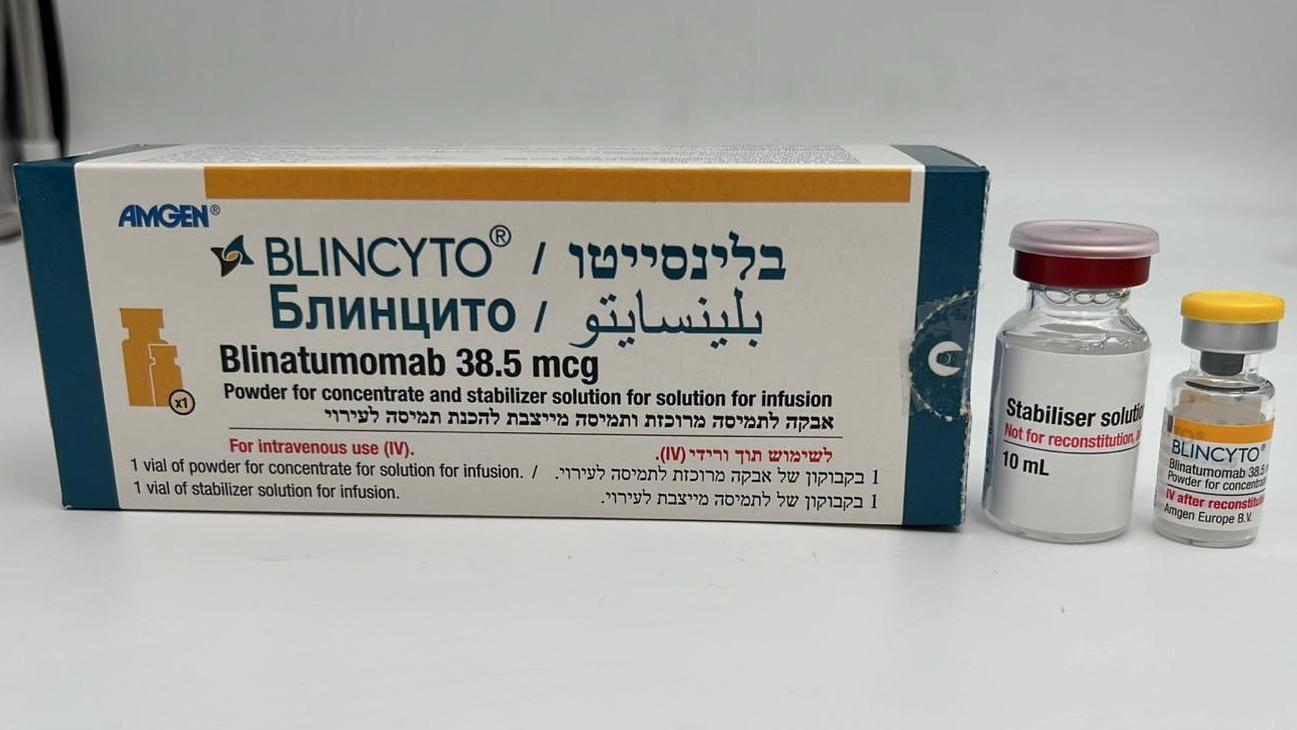
בלינסייטו BLINCYTO (BLINATUMOMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The adverse reactions described in this section were identified in clinical studies of patients with B-precursor ALL (N = 1,045). The most serious adverse reactions that may occur during blinatumomab treatment include: infections (22.6%), neurologic events (12.2%), neutropenia/febrile neutropenia (9.1%), cytokine release syndrome (2.7%), and tumor lysis syndrome (0.8%). The most common adverse reactions were: pyrexia (70.8%), infections - pathogen unspecified (41.4%), infusion-related reactions (33.4%), headache (32.7%), nausea (23.9%), anemia (23.3%), thrombocytopenia (21.6%), edema (21.4%), neutropenia (20.8%), febrile neutropenia (20.4%), diarrhea (19.7%), vomiting (19.0%), rash (18.0%), hepatic enzyme increased (17.2%), cough (15.0%), bacterial infectious disorders (14.1%), tremor (14.1%), cytokine release syndrome (13.8%), leukopenia (13.8%), constipation (13.5%), decreased immunoglobulins (13.4%), viral infectious disorders (13.3%), hypotension (13.0%), back pain (12.5%), chills (11.7%), abdominal pain (10.6%), tachycardia (10.6%), insomnia (10.4%), pain in extremity (10.1%), and fungal infectious disorders (9.6%). Tabulated list of adverse reactions Adverse reactions are presented below by system organ class and frequency category. Frequency categories were determined from the crude incidence rate reported for each adverse reaction in clinical studies of patients with B-precursor ALL (N = 1,045). Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness. MedDRA system Very common Common Uncommon organ class (≥ 1/10) (≥ 1/100 to < 1/10) (≥ 1/1,000 to < 1/100) Infections and Bacterial infectionsa, b Sepsis infestations Viral infectionsa, b Pneumonia Infections - pathogen Fungal infectionsa, b unspecifieda, b Blood and lymphatic Febrile neutropenia Leukocytosis5 Lymphadenopathy system disorders Anemia1 Lymphopenia6 Histiocytosis Neutropenia2 hematophagic Thrombocytopenia3 Leukopenia4 Immune system Cytokine release Hypersensitivity Cytokine storm disorders syndromea Metabolism and Tumor lysis syndrome nutrition disorders Psychiatric disordersa Insomnia Confusional state Disorientation Nervous system Headache Encephalopathy Speech disorder disordersa Tremor Aphasia Paresthesia Seizure Cognitive disorder Memory impairment Dizziness Somnolence Hypoesthesia Cranial nerve disorderb Ataxia Cardiac disorders Tachycardia7 Vascular disorders Hypotension8 Flushing Capillary leak Hypertension9 syndrome Respiratory, thoracic Cough Dyspnea Dyspnea exertional and mediastinal Productive cough Acute respiratory disorders Respiratory failure failure Wheezing Gastrointestinal Nausea Pancreatitisa disorders Diarrhea Vomiting Constipation Abdominal pain Hepatobiliary disorders Hyperbilirubinemiaa, 10 11 Skin and subcutaneous Rash tissue disorders Musculoskeletal and Back pain Bone pain connective tissue Pain in extremity disorders MedDRA system Very common Common Uncommon organ class (≥ 1/10) (≥ 1/100 to < 1/10) (≥ 1/1,000 to < 1/100) General disorders and Pyrexia12 Chest pain14 administration site Chills Pain conditions Edema13 Investigations Hepatic enzyme Weight increased increaseda, 15 Blood alkaline Decreased phosphatase increased immunoglobulins16 Injury, poisoning and Infusion-related procedural reactions17 complications a Additional information is provided in “Description of selected adverse reactions”. b MedDRA high level group terms (MedDRA version 23.0). Event terms that represent the same medical concept or condition were grouped together and reported as a single adverse reaction in the table above. The terms contributing to the relevant adverse reaction are indicated below: 1 Anemia includes anemia and hemoglobin decreased. 2 Neutropenia includes neutropenia and neutrophil count decreased. 3 Thrombocytopenia includes platelet count decreased and thrombocytopenia. 4 Leukopenia includes leukopenia and white blood cell count decreased. 5 Leukocytosis includes leukocytosis and white blood cell count increased. 6 Lymphopenia includes lymphocyte count decreased and lymphopenia. 7 Tachycardia includes sinus tachycardia, supraventricular tachycardia, tachycardia, atrial tachycardia and ventricular tachycardia. 8 Hypotension includes blood pressure decreased and hypotension. 9 Hypertension includes blood pressure increased and hypertension. 10 Hyperbilirubinemia includes blood bilirubin increased and hyperbilirubinemia. 11 Rash includes erythema, rash, rash erythematous, rash generalized, rash macular, rash maculo-papular, rash pruritic, catheter site rash, rash pustular, genital rash, rash papular and rash vesicular. 12 Pyrexia includes body temperature increased and pyrexia. 13 Edema includes bone marrow edema, periorbital edema, eyelid edema, eye edema, lip edema, face edema, localised edema, generalized edema, edema, edema peripheral, infusion site edema, edematous kidney, scrotal edema, edema genital, pulmonary edema, laryngeal edema, angioedema, circumoral edema and lymphedema. 14 Chest pain includes chest discomfort, chest pain, musculoskeletal chest pain and non-cardiac chest pain. 15 Hepatic enzyme increased includes alanine aminotransferase increased, aspartate aminotransferase increased, gamma-glutamyl transferase increased, hepatic enzyme increased, liver function test increased and transaminases increased. 16 Decreased immunoglobulins includes blood immunoglobulin G decreased, blood immunoglobulin A decreased, blood immunoglobulin M decreased, globulins decreased, hypogammaglobulinemia, hypoglobulinemia and immunoglobulins decreased. 17 Infusion-related reactions is a composite term that includes the term infusion-related reaction and the following events occurring with the first 48 hours of infusion and event lasted ≤ 2 days: pyrexia, cytokine release syndrome, hypotension, myalgia, acute kidney injury, hypertension, rash, tachypnea, swelling face, face edema and rash erythematous. Description of selected adverse reactions Neurologic events In the randomized phase III clinical study (N = 267) and the single-arm phase II clinical study (N = 189) in patients with Philadelphia chromosome negative relapsed or refractory B-precursor ALL treated with BLINCYTO, 66.0% of patients experienced one or more neurologic adverse reactions (including psychiatric disorders), primarily involving the CNS. Serious and grade ≥ 3 neurologic adverse reactions were observed in 11.6% and 12.1% of patients respectively, of which the most common serious adverse reactions were encephalopathy, tremor, aphasia, and confusional state. The majority of neurologic events (80.5%) were clinically reversible and resolved following interruption of BLINCYTO. The median time to the first event was within the first 2 weeks of treatment. One case of fatal encephalopathy has been reported in an earlier phase II clinical single-arm study. Neurologic events were reported for 62.2% of adult patients with Philadelphia chromosome positive relapsed or refractory B-precursor ALL (N = 45). Serious and grade ≥ 3 neurologic events were reported at 13.3% each in adult patients with Philadelphia chromosome positive relapsed or refractory B-precursor ALL. Neurologic events were reported for 71.5% of adult patients with MRD positive B-precursor ALL (N = 137), 22.6% of patients experienced serious events. Grade ≥ 3 and grade ≥ 4 events, respectively, were reported for 16.1% and 2.2% of adult patients with MRD positive B-precursor ALL. For clinical management of neurologic events, see section 4.4. Infections Life-threatening or fatal (grade ≥ 4) viral, bacterial and fungal infections have been reported in patients treated with BLINCYTO. In addition, reactivations of virus infection (e.g. Polyoma (BK)) have been observed in the phase II clinical study in adults with Philadelphia chromosome negative relapsed or refractory B-precursor ALL. Patients with Philadelphia chromosome negative relapsed or refractory B-precursor ALL with ECOG performance status at baseline of 2 experienced a higher incidence of serious infections compared to patients with ECOG performance status of < 2. For clinical management of infections, see section 4.4. Cytokine release syndrome (CRS) In the randomized phase III clinical study (N = 267) and the single-arm phase II clinical study (N = 189) in patients with Philadelphia chromosome negative relapsed or refractory B-precursor ALL treated with BLINCYTO, 14.7% of patients experienced CRS. Serious CRS reactions were reported in 2.4% of patients with a median time to onset of 2 days. Cytokine release syndrome was reported in 8.9% of adult patients with Philadelphia chromosome positive relapsed or refractory B-precursor ALL (N = 45), 2.2% of patients experienced serious events. No grade ≥ 3 or ≥ 4 events were reported. Cytokine release syndrome was reported in 2.9% of adult patients with MRD positive B-precursor ALL (N = 137). Grade 3 and serious events were reported for 1.5% each of adult patients with MRD positive B-precursor ALL; no grade ≥ 4 events were reported. Capillary leak syndrome was observed in 1 patient in the phase II clinical study in adult patients with Philadelphia chromosome negative relapsed or refractory B-precursor ALL and in 1 patient in the phase II clinical study in adult patients with MRD positive B-precursor ALL. Capillary leak syndrome was not observed in adult patients in the phase II clinical study in patients with Philadelphia chromosome positive relapsed or refractory B-precursor ALL. For clinical management of CRS, see section 4.4. Elevated liver enzymes In the randomized phase III clinical study (N = 267) and the single-arm phase II clinical study (N = 189) in patients with Philadelphia chromosome negative relapsed or refractory B-precursor ALL treated with BLINCYTO, 22.4% of patients reported elevated liver enzymes and associated signs/symptoms. Serious and grade ≥ 3 adverse reactions (such as ALT increased, AST increased, and blood bilirubin increased) were observed in 1.5% and 13.6% of patients respectively. The median time to onset to the first event was 4 days from the start of BLINCYTO treatment initiation. Elevated liver enzyme events were reported for 17.8% of adult patients with Philadelphia chromosome positive relapsed or refractory B-precursor ALL (N = 45), 2.2% of patients experienced serious events. Grade ≥ 3 and grade ≥ 4 events, respectively, were reported for 13.3% and 6.7% of adult patients with Philadelphia chromosome positive relapsed or refractory B-precursor ALL. Elevated liver enzyme events were reported for 12.4% of adult patients with MRD positive B-precursor ALL (N = 137). Grade ≥ 3 and grade ≥ 4 events, respectively, were reported for 8.0% and 4.4% of adult patients with MRD positive B-precursor ALL. The duration of hepatic adverse reactions has generally been brief and with rapid resolution, often when continuing uninterrupted treatment with BLINCYTO. For clinical management of elevated liver enzymes, see section 4.4. Pancreatitis Pancreatitis, life-threatening or fatal, has been reported in patients receiving BLINCYTO in the clinical studies and the post-marketing settings. The median time to onset was 7.5 days. For clinical management of pancreatitis, see section 4.4. Leukoencephalopathy including progressive multifocal leukoencephalopathy Leukoencephalopathy has been reported. Patients with brain MRI/CT findings consistent with leukoencephalopathy experienced concurrent serious adverse reactions including confusional state, tremor, cognitive disorder, encephalopathy, and convulsion. Although there is a potential for the development of progressive multifocal leukoencephalopathy (PML), no confirmed case of PML has been reported in the clinical studies. Pediatric population BLINCYTO has been evaluated in pediatric patients with relapsed or refractory B-precursor ALL in a phase I/II, single-arm dose escalation/evaluation study (MT103-205), in which 70 pediatric patients, aged 7 months to 17 years, were treated with the recommended dosage regimen. The most frequently reported serious adverse reactions were pyrexia (11.4%), febrile neutropenia (11.4%), cytokine release syndrome (5.7%), sepsis (4.3%), device-related infection (4.3%), overdose (4.3%), convulsion (2.9%), respiratory failure (2.9%), hypoxia (2.9%), pneumonia (2.9%), and multi-organ failure (2.9%). The adverse reactions in BLINCYTO-treated pediatric patients were similar in type to those seen in adult patients. Adverse reactions that were observed more frequently (≥ 10% difference) in the pediatric population compared to the adult population were anemia, thrombocytopenia, leukopenia, pyrexia, infusion-related reactions, weight increase, and hypertension. The type and frequency of adverse reactions were similar across different pediatric subgroups (gender, age and geographic region). At a dose higher than the recommended dose in study MT103-205, a case of fatal cardiac failure occurred in the setting of life-threatening cytokine release syndrome (CRS) and tumor lysis syndrome (TLS), see section 4.4. BLINCYTO has also been evaluated in pediatric patients with high-risk first relapsed B-precursor ALL in a randomized, controlled, open-label phase III study (20120215), in which 54 patients, aged 1 to 18 years, were treated with the recommended dosage regimen for high-risk first relapsed B-precursor ALL. The safety profile of BLINCYTO in study 20120215 is consistent with that of the studied pediatric relapsed or refractory B-precursor ALL population. Other special populations There is limited experience with BLINCYTO in patients ≥ 75 years of age. Generally, safety was similar between elderly patients (≥ 65 years of age) and patients less than 65 years of age treated with BLINCYTO. However, elderly patients may be more susceptible to serious neurologic events such as cognitive disorder, encephalopathy and confusion. Elderly patients with MRD positive ALL treated with BLINCYTO may have an increased risk of hypogammaglobulinemia compared to younger patients. It is recommended that immunoglobulin levels are monitored in elderly patients during treatment with BLINCYTO. The safety of BLINCYTO has not been studied in patients with severe renal impairment. Immunogenicity In clinical studies of adult ALL patients treated with BLINCYTO, less than 2% tested positive for anti-blinatumomab antibodies. Of patients who developed anti-blinatumomab antibodies, the majority had in vitro neutralizing activity. No anti-blinatumomab antibodies were detected in clinical studies of pediatric patients with relapsed or refractory ALL treated with blinatumomab. Anti-blinatumomab antibody formation may affect the pharmacokinetics of BLINCYTO. Overall, the totality of clinical evidence supports the finding that anti-blinatumomab antibodies are not suggestive of any clinical impact on the safety or effectiveness of BLINCYTO. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים אלה:1. חולים בגירים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL)) עמידה או חוזרת (Relapsed / Refractory).במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Blinatumomab, Inotuzumab ozogamicin, למעט בחולה אשר לא השיג תגובה מינימלית לאחר ניסיון טיפולי של מחזור טיפול אחד באחת מהתרופות האמורות.2. ילדים בני שנה ומעלה הלוקים בלוקמיה מסוג Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) עמידה או חוזרת (Relapsed / Refractory).לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה אלוגנאית של תאי גזע המטופואטיים.הטיפול לא יינתן כטיפול אחזקה.3. כמונותרפיה במבוגרים עם Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) בהפוגה ראשונה או שניה עם מחלה שארית מינימלית (MRD – minimal residual disease) בערך של 0.1% ומעלה. מחזור יחיד כחלק מטיפול קונסולידציה, בילדים חולי לוקמיה מסוג Philadelphia chromosome negative CD19 positive B-precursor ALL בסיכון גבוה, בחזרת מחלה ראשונה.לעניין זה הישנות בסיכון גבוה תוגדר כהישנות המתרחשת בתוך פחות מ-6 חודשים מסיום הטיפול הראשוני.4. מחזור יחיד כחלק מטיפול קונסולידציה, בילדים חולי לוקמיה מסוג Philadelphia chromosome negative CD19 positive B-precursor ALL בסיכון גבוה, בחזרת מחלה ראשונה.לעניין זה הישנות בסיכון גבוה תוגדר כהישנות המתרחשת בתוך פחות מ-6 חודשים מסיום הטיפול הראשוני.ב. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מונותרפיה במבוגרים עם Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) בהפוגה ראשונה או שניה עם מחלה שארית מינימלית (MRD – minimal residual disease) בערך של 0.1% ומעלה | 30/01/2020 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| חולים בגירים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL)) עמידה או חוזרת (Relapsed / Refractory). במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן - Blinatumomab, Inotuzumab ozogamicin, למעט בחולה אשר לא השיג תגובה מינימלית לאחר ניסיון טיפולי של מחזור טיפול אחד באחת מהתרופות האמורות. | 30/01/2020 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| ילדים בני שנה ומעלה הלוקים בלוקמיה מסוג Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) עמידה או חוזרת (Relapsed / Refractory). | 16/01/2019 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| התרופה תינתן לטיפול בחולים בגירים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL)) עמידה או חוזרת (Relapsed / Refractory). | 12/01/2017 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| התרופה תינתן לטיפול בחולים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL) בחולים בגירים, בהם מתקיימים כל התנאים הבאים: א. החולה חווה חזרת מחלה במהלך השנה הראשונה שלאחר טיפול כימותרפי והשתלת מח עצם (first relapse) (עד שנה מהשתלת מח העצם). ב. החולה מועמד להשתלת מח עצם אלוגנאית (השתלה שניה). ג. בדמו של החולה נספר מספר בלסטים הנמוך מ-50%. ד. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה. | 21/01/2016 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| מחזור יחיד כחלק מטיפול קונסולידציה, בילדים חולי לוקמיה מסוג Philadelphia chromosome negative CD19 positive B-precursor ALL בסיכון גבוה, בחזרת מחלה ראשונה. לעניין זה הישנות בסיכון גבוה תוגדר כהישנות המתרחשת בתוך פחות מ-6 חודשים מסיום הטיפול הראשוני. | 03/02/2022 | אונקולוגיה | Acute lymphoblastic leukemia, ALL |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
21/01/2016
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
17.05.18 - עלון לצרכן 07.03.19 - עלון לצרכן 16.09.19 - עלון לצרכן 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן עברית 01.02.22 - עלון לצרכן ערבית 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן אנגלית 14.03.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן עברית 01.02.22 - עלון לצרכן ערבית 13.03.22 - עלון לצרכן אנגלית 13.03.22 - עלון לצרכן עברית 13.03.22 - עלון לצרכן ערבית 04.09.23 - עלון לצרכן אנגלית 04.09.23 - עלון לצרכן עברית 04.09.23 - עלון לצרכן ערבית 09.06.20 - החמרה לעלון 27.04.21 - החמרה לעלון 13.03.22 - החמרה לעלון 04.09.23 - החמרה לעלון 16.11.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
בלינסייטו