Quest for the right Drug
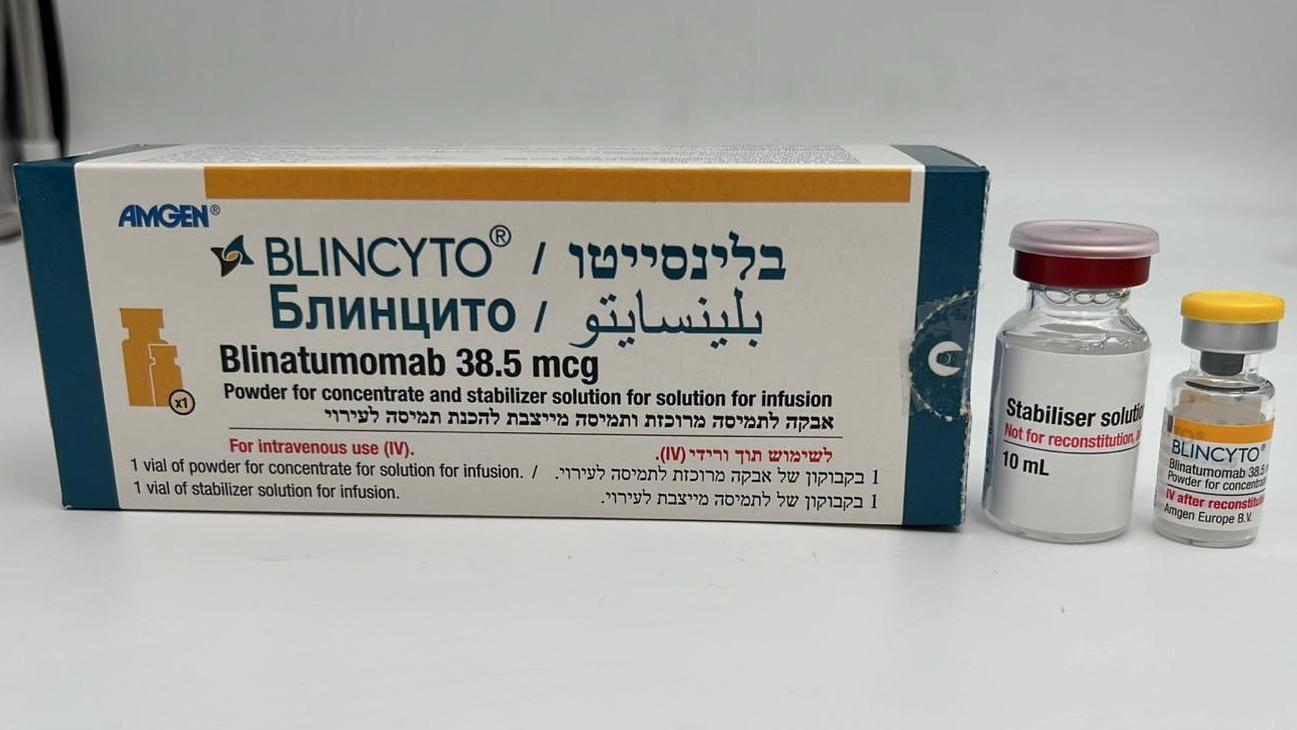
בלינסייטו BLINCYTO (BLINATUMOMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, other antineoplastic agents, ATC code: L01FX07. Mechanism of action Blinatumomab is a bispecific T-cell engager molecule that binds specifically to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T-cells. It activates endogenous T-cells by connecting CD3 in the T-cell receptor (TCR) complex with CD19 on benign and malignant B-cells. The anti-tumor activity of blinatumomab immunotherapy is not dependent on T-cells bearing a specific TCR or on peptide antigens presented by cancer cells, but is polyclonal in nature and independent of human leukocyte antigen (HLA) molecules on target cells. Blinatumomab mediates the formation of a cytolytic synapse between the T-cell and the tumor cell, releasing proteolytic enzymes to kill both proliferating and resting target cells. Blinatumomab is associated with transient upregulation of cell adhesion molecules, production of cytolytic proteins, release of inflammatory cytokines, and proliferation of T-cells, and results in elimination of CD19+ cells. Pharmacodynamic effects Consistent immune-pharmacodynamic responses were observed in patients studied. During the continuous intravenous infusion over 4 weeks, the pharmacodynamic response was characterized by T-cell activation and initial redistribution, rapid peripheral B-cell depletion, and transient cytokine elevation. Peripheral T-cell redistribution (i.e. T-cell adhesion to blood vessel endothelium and/or transmigration into tissue) occurred after start of blinatumomab infusion or dose escalation. T-cell counts initially declined within 1 to 2 days and then returned to baseline levels within 7 to 14 days in the majority of patients. Increase of T-cell counts above baseline (T-cell expansion) was observed in few patients. Peripheral B-cell counts decreased rapidly to an undetectable level during treatment at doses ≥ 5 mcg/m2/day or ≥ 9 mcg/day in the majority of patients. No recovery of peripheral B-cell counts was observed during the 2-week treatment-free period between treatment cycles. Incomplete depletion of B-cells occurred at doses of 0.5 mcg/m2/day and 1.5 mcg/m2/day and in a few non-responders at higher doses. Peripheral lymphocytes were not measured in pediatric subjects. Cytokines including IL-2, IL-4, IL-6, IL-8, IL-10, IL-12, TNF-α and IFN-γ were measured and, IL-6, IL-10 and IFN-γ were most elevated. Transient elevation of cytokines was observed in the first 2 days following start of blinatumomab infusion. The elevated cytokine levels returned to baseline within 24 to 48 hours during the infusion. In subsequent treatment cycles, cytokine elevation occurred in fewer patients with lesser intensity compared to the initial 48 hours of the first treatment cycle. Clinical efficacy and safety Philadelphia chromosome negative relapsed or refractory B-precursor ALL A total of 456 patients aged ≥ 18 years of age with relapsed or refractory B-precursor ALL were exposed to BLINCYTO during the phase II and phase III clinical studies described below. The safety and efficacy of BLINCYTO compared to standard of care (SOC) chemotherapy were evaluated in a randomized, open-label, multicenter, phase III study (TOWER). Eligible patients were ≥ 18 years of age and ECOG status ≤ 2 with relapsed or refractory B-precursor ALL (had > 5% blasts in the bone marrow and either relapse at any time after allogeneic HSCT, untreated first relapse with first remission duration < 12 months, or refractory to last therapy). Patients were randomized 2:1 to receive BLINCYTO or 1 of 4 prespecified, investigator-selected, SOC backbone chemotherapy regimens. Randomization was stratified by age (< 35 years versus ≥ 35 years of age), prior salvage therapy (yes versus no), and prior allogeneic HSCT (yes versus no) as assessed at the time of consent. The demographics and baseline characteristics were well-balanced between the two arms (see table 3). Table 3. Demographics and baseline characteristics in phase III study (TOWER) BLINCYTO SOC chemotherapy Characteristic (N = 271) (N = 134) Age Median, years (min, max) 37 (18, 80) 37 (18, 78) Mean, years (SD) 40.8 (17.1) 41.1 (17.3) ≥ 65 Years, n (%) 33 (12.2) 15 (11.2) Prior salvage therapy 164 (60.5) 80 (59.7) 0 114 (42.1) 65 (48.5) 1 91 (33.6) 43 (32.1) ≥2 66 (24.3) 26 (19.4) Prior alloHSCT 94 (34.7) 46 (34.3) ECOG status - n (%) 0 96 (35.4) 52 (38.8) 1 134 (49.4) 61 (45.5) 2 41 (15.1) 20 (14.9) Refractory status - n (%) Primary refractory 46 (17.0) 27 (20.1) Refractory to salvage therapy 87 (32.1) 34 (25.4) Maximum of central/local bone marrow blasts - n (%) ≥ 50% 201 (74.2) 104 (77.6) AlloHSCT = allogeneic hematopoietic stem cell transplantation SOC = standard of care BLINCYTO was administered as a continuous intravenous infusion. In the first cycle, the initial dose was 9 mcg/day for week 1, then 28 mcg/day for the remaining 3 weeks. The target dose of 28 mcg/day was administered in cycle 2 and subsequent cycles starting on day 1 of each cycle. Dose adjustment was possible in case of adverse reactions. Of the 267 patients who received BLINCYTO, the mean number of completed treatment cycles was 2.0; of the 109 patients who received SOC chemotherapy, the mean number of treatment cycles was 1.3. The primary endpoint was overall survival (OS). The median OS was 4.0 months (95% CI: 2.9, 5.3) in the SOC chemotherapy arm compared with 7.7 months (95% CI: 5.6, 9.6) in the BLINCYTO arm. The hazard ratio (95% CI) was 0.71 (0.55, 0.93) between treatment arms favoring BLINCYTO, indicated a 29% reduction in hazard rate in the BLINCYTO arm (p-value = 0.012 (stratified log-rank test)), see figure 1. Consistency in OS results was shown in subgroups by stratification factors. Consistent results were observed after censoring at the time of HSCT; median OS, censored at the time of HSCT, was 6.9 months (95% CI: 5.3, 8.8) in the BLINCYTO group and 3.9 months (95% CI: 2.8, 4.9) in the SOC group (HR, 0.66; 95% CI: 0.50, 0.88; p-value = 0.004). The mortality rate following alloHSCT among all responders who did not receive anti-leukemic therapy was 10/38 (26.3%; 95% CI: 13.4, 43.1) in the BLINCYTO group and 3/12 (25%; 95% CI: 5.5, 57.2) in the SOC group; such mortality rate at 100 days post alloHSCT was 4/38 (12.4%; 95% CI: 4.8%, 29.9%) in the BLINCYTO group and 0/12 (0%; 95% CI: not estimable) in the SOC group. Efficacy results from other key endpoints in the study are summarized in table 4. Figure 1. Kaplan-Meier curve of overall survival Table 4. Efficacy results in patients ≥ 18 years of age with Philadelphia chromosome negative relapsed or refractory B-precursor ALL (TOWER) BLINCYTO SOC chemotherapy (N = 271) (N = 134) Complete remission (CR) 119 (43.9) (37.9, 50.0) 33 (24.6) (17.6, 32.8) CRa/CRh*b/CRic, n (%) [95% CI] Treatment difference [95% CI] 19.3 (9.9, 28.7) p-value < 0.001 CR, n (%) [95% CI] 91 (33.6) (28.0, 39.5) 21 (15.7) (10.0, 23.0) Treatment difference [95% CI] 17.9 (9.6, 26.2) p-value < 0.001 Event-free survivald 6-month estimate % [95% CI] 30.7 (25.0, 36.5) 12.5 (7.2, 19.2) 18-months estimate % [95% CI] 9.5 (5.1, 15.6) 7.9 (3.7, 14.2) HR [95% CI] 0.55 (0.43, 0.71) Duration of hematological response- Median time to event [95% CI] CR 8.3 (5.7, 10.7) 7.8 (2.2, 19.0) CR/CRh*/CRi 7.3 (5.8, 9.9) 4.6 (1.8, 19.0) e MRD response for CR/CRh*/CRi MRD evaluable patients (%) 16/33 (48.5) (30.8, 74/97 (76.3) (66.6, 84.3) [95% CI]f 66.5) Duration of MRD response- 4.5 months (3.6, 9.0) 3.8 months (1.9, 19.0) Median time to event [95% CI] Postbaseline alloHSCT - n (%) Overall subjects 65 (24) 32 (23.9) Hematological responders 50 (42.0) 18 (54.5) (CR/CRh*/CRi) Time to alloHSCT among all transplanted patients 3.7 months (3.0, 5.3) 3.1 months (2.6, 4.3) Median time to event (N = 65) (N = 32) (Interquartile range) BLINCYTO SOC chemotherapy (N = 271) (N = 134) Time to alloHSCT among CR/CRh*/CRi responders 11.3 months (5.2, NE) 3.6 months (2.3, 7.2) Median time to event [95% CI] (N = 119) (N = 33) (KM estimate) 100 day mortality after alloHSCT n/N (%), [95% CI] 4/38, 12.4% (4.8, 29.9) 0/12, 0.0% (0.0, NE) a CR was defined as ≤ 5% blasts in the bone marrow, no evidence of disease, and full recovery of peripheral blood counts (platelets > 100,000/microliter and absolute neutrophil counts [ANC] > 1,000/microliter). b CRh* (complete remission with partial hematologic recovery) was defined as ≤ 5% blasts in the bone marrow, no evidence of disease, and partial recovery of peripheral blood counts (platelets > 50,000/microliter and ANC > 500/microliter). c CRi (complete remission with incomplete hematologic recovery) was defined as ≤ 5% blasts in the bone marrow, no evidence of disease, and incomplete recovery of peripheral blood counts (platelets > 100,000/microliter or ANC > 1,000/microliter). d EFS time was calculated from the time of randomization until the date of disease assessment indicating a relapse after achieving a CR/CRh*/CRi or death, whichever is earlier. Subjects who fail to achieve a CR/CRh*/CRi within 12 weeks of treatment initiation are considered treatment failures and assigned an EFS duration of 1 day. e MRD (minimum residual disease) response was defined as MRD by PCR or flow cytometry < 1 × 10-4. f Patients who achieved CR/CRh*/CRi and had an evaluable post baseline MRD assessment. Health related quality of life In this open-label study, Health related quality of life (HRQoL) reported by patients were measured using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire – Core 30 (EORTC QLQ-C30). In a post-hoc sensitivity analysis, compared to SOC, BLINCYTO consistently delayed the time to clinically meaningful deterioration of HRQoL (≥ 10-point worsening from baseline) for global health status [median BLINCYTO versus SOC: 8.1 months versus 1.0 month; HR = 0.60 (95% CI: 0.42, 0.85)], functional scales, symptom scales and individual items. Because the health related quality of life results are based on a post-hoc sensitivity analysis, the results should be interpreted with caution. BLINCYTO was also evaluated in an open-label, multicenter, single-arm phase II study of 189 patients (MT103-211). Eligible patients were ≥ 18 years of age with Philadelphia chromosome negative relapsed or refractory B-precursor ALL (relapsed with first remission duration of ≤ 12 months in first salvage, or relapsed or refractory after first salvage therapy, or relapsed within 12 months of allogeneic HSCT, and had ≥ 10% blasts in bone marrow). Pre-medication, BLINCYTO dose per treatment cycle and route of administration were identical to those in the phase III study. Patients were premedicated with a mandatory cerebrospinal fluid prophylaxis consisting of an intrathecal regimen according to institutional or national guidelines within 1 week prior to start of BLINCYTO treatment. BLINCYTO was administered as a continuous intravenous infusion. In the first cycle, the initial dose was 9 mcg/day for week 1, then 28 mcg/day for the remaining 3 weeks. The target dose of 28 mcg/day was administered in cycle 2 and subsequent cycles starting on day 1 of each cycle. Dose adjustment was possible in the case of adverse reactions. The treated population included 189 patients who received at least 1 infusion of BLINCYTO; the mean number of cycles per patient was 1.6. Patients who responded to BLINCYTO but later relapsed had the option to be retreated with BLINCYTO. Among treated patients, the median age was 39 years (range: 18 to 79 years, including 25 patients ≥ 65 years of age), 64 of 189 (33.9%) had undergone HSCT prior to receiving BLINCYTO and 32 of 189 (16.9%) had received more than 2 prior salvage therapies. The primary endpoint was the complete remission/complete remission with partial hematological recovery (CR/CRh*) rate within 2 cycles of treatment with BLINCYTO. Eighty-one of 189 (42.9%) patients achieved CR/CRh* within the first 2 treatment cycles with the majority of responses (64 of 81) occurring within 1 cycle of treatment. In the elderly population (≥ 65 years of age) 11 of 25 patients (44.0%) achieved CR/CRh* within the first 2 treatment cycles (see section 4.8 for safety in elderly). Four patients achieved CR during consolidation cycles, resulting in a cumulative CR rate of 35.4% (67/189; 95% CI: 28.6% - 42.7%). Thirty-two of 189 (17%) patients underwent allogeneic HSCT in CR/CRh* induced with BLINCYTO (see table 5). Table 5. Efficacy results in patients ≥ 18 years of age with Philadelphia chromosome negative relapsed or refractory B-precursor ALL (MT103-211) n (%) 95% CI n = 189 Complete remission (CR)1/Complete remission 81 (42.9%) [35.7% – 50.2%] with partial hematological recovery (CRh*)2 CR 63 (33.3%) [26.7% – 40.5%] CRh* 18 (9.5%) [5.7% – 14.6%] Blast free hypoplastic or aplastic bone marrow3 17 (9.0%) [5.3% – 14.0%] Partial remission4 5 (2.6%) [0.9% – 6.1%] Relapse5-free survival (RFS) for CR/CRh* 5.9 months [4.8 to 8.3 months] Overall survival 6.1 months [4.2 to 7.5 months] 1 CR was defined as ≤ 5% of blasts in the bone marrow, no evidence of disease, and full recovery of peripheral blood counts (platelets > 100,000/microliter and absolute neutrophil counts [ANC] > 1,000/microliter). 2 CRh* was defined as ≤ 5% of blasts in the bone marrow, no evidence of disease, and partial recovery of peripheral blood counts (platelets > 50,000/microliter and ANC > 500/microliter). 3 Blast free hypoplastic or aplastic bone marrow was defined as bone marrow blasts ≤ 5%, no evidence of disease, insufficient recovery of peripheral blood counts: platelets ≤ 50,000/microliter and/or ANC ≤ 500/microliter. 4 Partial remission was defined as bone marrow blasts 6% to 25% with at least a 50% reduction from baseline. 5 Relapse was defined as hematological relapse (blasts in bone marrow greater than 5% following CR) or an extramedullary relapse. In a prespecified exploratory analysis, 60 of 73 MRD evaluable patients with CR/CRh* (82.2%) also had a MRD response (defined as MRD by PCR < 1 × 10-4). Patients with prior allogeneic HSCT had similar response rates to those without prior HSCT, older patients had similar response rates to younger patients, and no substantial difference was observed in remission rates based on the number of lines of prior salvage treatment. In patients with non-CNS/non-testes extramedullary disease (defined as at least 1 lesion ≥ 1.5 cm) at screening (N = 8/189) clinical response rates (25% [95% CI: 3.2 - 65.1]) were lower compared with patients with no evidence of extramedullary disease (N = 181, 43.6% [95% CI: 36.3 - 51.2]) (see figure 2). Patients with the highest tumor burden as measured by the percentage of bone marrow blast cells at baseline (≥ 90%) still had a clinically meaningful response with a CR/CRh* rate of 21.6% (95% CI: 12.9 - 32.7) (see figure 2). Patients with low tumor burden (< 50%) responded best to BLINCYTO treatment with CR/CRh* rate of 72.9% (95% CI: 59.7 – 83.6). Figure 2. Forest plot of CR/CRh* rate during the first 2 cycles for study MT103-211 (primary analysis set) n = number of patients who achieved CR or CRh* in the first 2 cycles of treatment in the specified subgroup. N = total number of patients in the specified subgroup. There is limited data in patients with late first relapse of B-precursor ALL defined as a relapse occurring more than 12 months after first remission or more than 12 months after HSCT in the first remission. In clinical phase II studies, 88.9% (8/9) of patients with late first relapse as defined in the individual studies achieved CR/CRh* within the first 2 treatment cycles with 62.5% (6/9) achieving MRD response and 37.5% (3/9) undergoing allogeneic HSCT after treatment with BLINCYTO. The median overall survival (OS) was 17.7 months (95% CI: 3.1 – not estimable). In the randomized, open-label, multicenter, phase III study (TOWER), 70% (7/10) of post-transplant patients in late first relapse treated with BLINCYTO compared to 20% (1/5) treated with SOC chemotherapy achieved CR/CRh* within the first 2 treatment cycles. Fifty percent (5/10) compared to 0% (0/5) achieved MRD response and 20% (2/10) compared to 40% (2/5) underwent allogeneic HSCT after treatment. The median OS was 15.6 months (95% CI: 5.5 – not estimable) for the BLINCYTO group and 5.3 months (95% CI: 1.1 – not estimable) for the SOC chemotherapy group. Philadelphia chromosome positive relapsed or refractory B-precursor ALL in adult patients The safety and efficacy of BLINCYTO were evaluated in an open-label, multicenter, single-arm phase II study (ALCANTARA). Eligible patients were ≥ 18 years of age with Philadelphia chromosome positive B-precursor ALL: relapsed or refractory to at least 1 second generation or later tyrosine kinase inhibitor (TKI); OR intolerant to second generation TKI, and intolerant or refractory to imatinib mesylate. BLINCYTO was administered as a continuous intravenous infusion. In the first cycle, the initial dose was 9 mcg/day for week 1, then 28 mcg/day for the remaining 3 weeks. The dose of 28 mcg/day was administered in cycle 2 and subsequent cycles starting on day 1 of each cycle. Dose adjustment was possible in case of adverse reactions. The treated population included 45 patients who received at least one infusion of BLINCYTO; the mean number of treatment cycles was 2.2 (see table 6 for patient demographics and baseline characteristics). Table 6. Demographics and baseline characteristics in phase II study (ALCANTARA) BLINCYTO Characteristic (N = 45) Age Median, years (min, max) 55 (23, 78) Mean, years (SD) 52.8 (15) ≥ 65 Years and < 75 years, n (%) 10 (22.2) ≥ 75 Years, n (%) 2 (4.4) Males, n (%) 24 (53.3) Race, n (%) Asian 1 (2.2) Black (or African American) 3 (6.7) Other 2 (4.4) White 39 (86.7) Disease History, n (%) Prior TKI treatmenta 1 7 (15.6) 2 21 (46.7) ≥3 17 (37.8) Prior salvage therapy 31 (61.9) Prior alloHSCTb 20 (44.4) Bone marrow blastsc, n (%) ≥ 50% to < 75% 6 (13.3) ≥ 75% 28 (62.2) a number of patients that failed ponatinib = 23 (51.1%) b alloHSCT = allogeneic hematopoietic stem cell transplantation c centrally assessed The primary endpoint was the CR/CRh* rate within 2 cycles of treatment with BLINCYTO. Sixteen out of 45 (35.6%) patients achieved CR/CRh* within the first 2 treatment cycles. Of the 16 patients with CR/CRh* in the first 2 cycles, 12 of 14 (85.7%) patients with a CR and 2 of 2 (100%) patients with a CRh* also achieved an MRD complete response (see table 7). Two patients achieved CR during subsequent cycles, resulting in a cumulative CR rate of 35.6% (16 out of 45; 95% CI: 21.9 – 51.2). Five out of 16 (31.3%) patients underwent allogeneic HSCT in CR/CRh* induced with BLINCYTO. Table 7. Efficacy results in patients ≥ 18 years of age with Philadelphia chromosome positive relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL) (ALCANTARA) N = 45 a Complete remission (CR) /Complete remission with partial 16 (35.6) [21.9, 51.2] hematological recovery (CRh*)b, n (%) [95% CI] CR 14 (31.1) [18.2, 46.6] CRh* 2 (4.4) [0.5, 15.1] CRic (without CRh*), n (%) [95% CI] 2 (4.4) [0.5, 15.1] Blast free hypoplastic or aplastic bone marrow (without CRi)d, n (%) 3 (6.7) [1.4, 18.3] [95% CI] Partial remissione, n (%) [95% CI] 2 (4.4) [0.5, 15.1] Complete MRD responsef, n (%) [95% CI] 18 (40.0) [25.7, 55.7] Median Relapseg-free survival (RFS) for CR/CRh* [95% CI] 6.7 months [4.4 to NEh] Median Overall survival [95% CI] 7.1 months [5.6 to NEh] a CR was defined as ≤ 5% of blasts in the bone marrow, no evidence of disease, and full recovery of peripheral blood counts (platelets > 100,000/microliter and absolute neutrophil counts [ANC] > 1,000/microliter). b CRh* was defined as ≤ 5% of blasts in the bone marrow, no evidence of disease, and partial recovery of peripheral blood counts (platelets > 50,000/microliter and ANC > 500/microliter). c CRi (complete remission with incomplete hematologic recovery) was defined as ≤ 5% blasts in the bone marrow, no evidence of disease, and incomplete recovery of peripheral blood counts (platelets > 100,000/microliter or ANC > 1,000/microliter). d Blast free hypoplastic or aplastic bone marrow was defined as bone marrow blasts ≤ 5%, no evidence of disease, insufficient recovery of peripheral counts: platelets ≤ 50,000/microliter and/or ANC ≤ 500/microliter. e Partial remission was defined as bone marrow blasts 6% to 25% with at least a 50% reduction from baseline. f Complete MRD response was defined as the absence of detectable MRD confirmed in an assay with minimum sensitivity of 10-4. g Relapse was defined as hematological relapse (blasts in bone marrow greater than 5% following CR) or an extramedullary relapse. h NE = not estimable. Patients with the higher tumor burden as measured by the percentage of bone marrow blast cells at baseline (≥ 50%) still had a clinically meaningful response with a CR/CRh* rate of 26.5% (95% CI: 12.9 – 44.4). Patients with low tumor burden (< 50%) responded best to BLINCYTO treatment with CR/CRh* rate of 63.6% (95% CI: 30.8 – 89.1). For patients with high peripheral white blood cell counts (≥ 3.0 × 109/L), response rate was 27.3% (95% CI: 10.7 – 50.2) while percentage of response for those with a lower white blood cell count (< 3.0 × 109/L) was 43.5% (95% CI: 23.2 – 65.5). Treatment effects in evaluable subgroups (e.g. mutation status, number of prior TKIs, prior HSCT status, and relapse without prior HSCT) were in general consistent with the results in the overall population. Patients with T315I mutation, other mutations, or additional cytogenetic abnormalities responded with a similar rate as compared to those that did not have these mutations or abnormalities. MRD positive B-precursor ALL The safety and efficacy of BLINCYTO in adult patients with MRD positive B-precursor ALL were evaluated in an open-label, multicenter, single-arm phase II study (BLAST). Eligible patients were ≥ 18 years of age with no prior HSCT, had received at least 3 blocks of standard ALL induction therapy, were in complete hematologic remission (defined as < 5% blasts in bone marrow, absolute neutrophil count ≥ 1,000/microliters, platelets ≥ 50,000/microliters, and hemoglobin level ≥ 9 g/dL) and had molecular failure or molecular relapse (defined as MRD ≥ 10-3), see table 8. MRD status at screening was determined from bone marrow aspirations using flow cytometry or polymerase chain reaction (PCR) at a minimum sensitivity of 10-4 based on local site evaluations. A central laboratory subsequently confirmed MRD levels by PCR. Final interpretation of MRD results followed EuroMRD Consortium guidelines. Table 8. Demographics and baseline characteristics in MRD study (BLAST) BLINCYTO Characteristic (N = 116) Age Median, years (min, max) 45 (18, 76) Mean, years (SD) 44.6 (16.4) ≥ 65 years, n (%) 15 (12.9) Males, n (%) 68 (58.6) Race, n (%) Asian 1 (0.9) Other (mixed) 1 (0.9) White 102 (87.9) Unknown 12 (10.3) Relapse history n (%) Patients in 1st CR 75 (64.7) Patients in 2nd CR 39 (33.6) Patients in 3rd CR 2 (1.7) BLINCYTO Characteristic (N = 116) MRD level at baseline*, n (%) ≥ 10-1 and < 1 9 (7.8) ≥ 10-2 and < 10-1 45 (38.8) ≥ 10-3 and < 10-2 52 (44.8) < 10-3 3 (2.6) Below lower limit of quantification 5 (4.3) Unknown 2 (1.7) * Centrally assessed in an assay with minimum sensitivity of 10-4 BLINCYTO was administered as a continuous intravenous infusion. Patients received BLINCYTO at a constant dose of 15 mcg/m2/day (equivalent to the recommended dosage of 28 mcg/day) for all treatment cycles. Patients received up to 4 cycles of treatment. Dose adjustment was possible in case of adverse reactions. The treated population included 116 patients who received at least one infusion of BLINCYTO; the mean number of completed treatment cycles was 1.8 (range: 1 to 4). The primary endpoint was the proportion of patients who achieved a complete MRD response within one cycle of BLINCYTO treatment. Eighty-eight out of 113 (77.9%) evaluable patients achieved a complete MRD response after one cycle of treatment; see table 9. Two subjects achieved a complete MRD response with 1 additional cycle of BLINCYTO. MRD response rates by age and MRD level at baseline subgroups were consistent with the results in the overall population. RFS in patients with Philadelphia chromosome negative B-precursor ALL at 18 months censored at HSCT or post-BLINCYTO chemotherapy was 54% (33%, 70%). RFS at 18 months not censored at HSCT or post-BLINCYTO chemotherapy was 53% (44%, 62%). Table 9. Efficacy results in patients ≥ 18 years of age with MRD positive B-precursor ALL (BLAST) Complete MRD responsea, n/N (%), [95% CI] 88/113b (77.9) [69.1 - 85.1] ≥ 65 years old 12/15 (80.0) [51.9 - 95.7] Patients in 1st CR 60/73 (82.2) [71.5 - 90.2] Patients in 2nd CR 27/38 (71.1) [54.1 - 84.6] Patients in 3rd CR 1/2 (50.0) [1.3 - 98.7] Duration of complete MRD response [95% CI] 17.3 months [12.6 - 23.3] a Complete MRD response was defined as the absence of detectable MRD confirmed in an assay with minimum sensitivity of 10-4. b One hundred thirteen patients (97.4%; 113/116) were included in the primary endpoint full analysis set. Pediatric population The safety and efficacy of BLINCYTO compared to standard of care (SOC) consolidation chemotherapy were evaluated in a randomized, controlled, open-label, multicenter study (20120215). Eligible patients were between 28 days and 18 years of age with high-risk first relapsed Philadelphia chromosome negative B-precursor ALL and had < 25% blasts in the bone marrow. High-risk patients were defined as per IntReALL criteria. Patients with clinically relevant CNS pathology requiring treatment (e.g. unstable epilepsy) or evidence of current CNS involvement by ALL were excluded from the study. Patients were enrolled and randomized after induction and 2 blocks of consolidation chemotherapy. Patients were randomized 1:1 to receive BLINCYTO or a third block of SOC consolidation chemotherapy. Patients in the BLINCYTO arm received one cycle of BLINCYTO as a continuous intravenous infusion at 15 mcg/m2/day over 4 weeks (maximum daily dose was not to exceed 28 mcg/day). Dose adjustment was possible in case of adverse reactions. Randomization was stratified by age (< 1 year, 1 to 9 years, and > 9 years), bone marrow status determined at the end of the second block of consolidation chemotherapy and MRD status determined at the end of induction (blasts < 5% with MRD level < 10-3, blasts < 5% with MRD level ≥ 10-3, and blasts ≥ 5% and < 25%). The demographics and baseline characteristics were well-balanced between the two arms (see table 10). No subject had prior HSCT. Table 10. Demographics and baseline characteristics in study 20120215 BLINCYTO SOC Chemotherapy Characteristics (N = 54) (N = 54) Age, n (%) < 1 year 0 (0.0) 0 (0.0) 1 to 9 years 39 (72.2) 38 (70.4) ≥ 10 to 18 years 15 (27.8) 16 (29.6) Males, n (%) 30 (55.6) 22 (40.7) Race, n (%) American Indian or Alaska Native 0 (0.0) 0 (0.0) Asian 1 (1.9) 3 (5.6) Black (or African American) 0 (0.0) 3 (5.6) Native Hawaiian or Other Pacific 0 (0.0) 0 (0.0) Islander Other 3 (5.6) 5 (9.3) White 50 (92.6) 43 (79.6) Occurrence and type of any genetic abnormality, n (%) No 34 (63.0) 29 (53.7) Yes 20 (37.0) 25 (46.3) Hyperdiploidy 6 (11.1) 6 (11.1) Hypodiploidy 1 (1.9) 0 (0.0) t(v;11q23)/MLL rearranged 0 (0.0) 4 (7.4) t(12;21)(p13;q22)/TEL-AML1 2 (3.7) 3 (5.6) t(1;19)(q23;p13.3)/E2A-PBX1 2 (3.7) 2 (3.7) t(5;14)(q31;32)/IL3-IGH 0 (0.0) 0 (0.0) Other 9 (16.7) 10 (18.5) Extramedullary disease at relapse, n (%) No 44 (81.5) 40 (74.1) Yes 10 (18.5) 14 (25.9) Cytomorphology, n (%) Blasts < 5% 54 (100.0) 51 (94.4) Blasts ≥ 5% and < 25% 0 (0.0) 2 (3.7) Blasts ≥ 25% 0 (0.0) 0 (0.0) Not evaluable 0 (0.0) 1 (1.9) MRD PCR value, n (%) ≥ 10-4 10 (18.5) 13 (24.1) < 10-4 20 (37.0) 22 (40.7) Time from first diagnosis to relapse (month), n (%) < 18 months 19 (35.2) 22 (40.7) ≥ 18 months and ≤ 30 months 32 (59.3) 28 (51.9) > 30 months 3 (5.6) 4 (7.4) The primary endpoint was event-free survival (EFS). The study demonstrated statistically significant improvement in EFS for patients treated with BLINCYTO as compared to SOC consolidation chemotherapy. In patients who received the SOC consolidation chemotherapy, the 36-month Kaplan-Meier estimate of EFS, with a hazard ratio (95% CI) of 0.36 (0.19, 0.66) was 26.9% (95% CI: 13.2%, 42.8%) compared to 55.7% (95% CI: 37.8%, 70.4%) in patients who received BLINCYTO. Treatment effects in subgroups (e.g. age, tumor burden/MRD status, time from first diagnosis to relapse) were in general consistent with the results in the overall population. See figure 3 and table 11 for efficacy results from study 20120215. Figure 3. Kaplan-Meier curve of event-free survival 1.0 0.9 Stratified Log Rank: p = <0.001 Hazard ratio (95% CI) from stratified Cox regression: 0.36 (0.19, 0.66) 0.8 0.7 Survival Probability 0.6 0.5 0.4 0.3 0.2 0.1 0.0 Number of Subjects at Risk: 1: 54 35 22 17 13 11 9 8 5 5 5 5 4 2 0 GRH2386 v1 2: 54 49 37 28 24 22 21 19 15 12 10 7 4 1 0 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 Months Treatment (N), Median (95% CI) 1: HC3 (N = 54), 7.4 (4.5, 12.7) 2: Blinatumomab (N = 54), NE (12.0, NE) Table 11. Efficacy results in pediatric patients with high-risk first relapsed B-precursor ALL (20120215) BLINCYTO SOC Chemotherapy (N = 54) (N = 54) Event-free survivala Events (%) 18 (33.3) 31 (57.4) Median, months [95% CI] NEb [12.0, NEb] 7.4 [4.5, 12.7] Hazard ratio [95% CI]c 0.36 [0.19, 0.66] p-valued < 0.001 Overall survival Number of deaths (%) 8 (14.8) 16 (29.6) 36-month estimate (%) [95% CI] 81.1 [65.5, 90.2] 55.8 [36.9, 71.0] Hazard ratio [95% CI]c,d 0.43 [0.18, 1.01] p-valuee,f 0.047 MRD responseg Number of MRD response, n1/n2h (%) 44/49 (89.8) 26/48 (54.2) [95% CI] [77.8, 96.6] [39.2, 68.6] p-valuef,i < 0.001 Note: Efficacy results from primary analysis (data cut-off of 17 July 2019). a EFS time was calculated from the time of randomization until the date of relapse or tumor burden of ≥ 5% and < 25% blasts after having achieved a complete remission (CR), failure to achieve a CR at the end of treatment, secondary malignancy, or death due to any cause, whichever occurs first. b NE = not estimable. c Based on stratified Cox’s model. d The updated hazard ratio for OS (data cut-off of 14 September 2020) was 0.33 (95% CI: 0.15 to 0.72). e The p-value was derived using a stratified log-rank test. f Endpoint not formally tested. The p-value was not adjusted for multiplicity. g MRD (minimum residual disease) response was defined as MRD by PCR < 1 × 10-4. h n1: number of patients who achieved a MRD response after having a baseline MRD ≥ 10-4 or < 10-4; n2: number of patients assessed. i The p-value was derived using Cochran Mantel Haenszel test. The safety and efficacy of BLINCYTO were also evaluated in an open-label, multicenter, single-arm study in 93 pediatric patients with relapsed or refractory B-precursor ALL (second or later bone marrow relapse, in any marrow relapse after allogeneic HSCT, or refractory to other treatments, and also with > 25% blasts in bone marrow) (MT103-205). This was a two-part study, a dose-finding part to determine the appropriate dosing regimen, followed by a single-arm efficacy part using this regimen. BLINCYTO was administered as a continuous intravenous infusion. In the dose-finding part of the study, doses of up to 30 mcg/m2/day were evaluated. The recommended dose for the pharmacokinetics (PK) expansion and efficacy parts of the study was determined to be 5 mcg/m2/day on days 1-7 and 15 mcg/m2/day on days 8-28 for cycle 1, and 15 mcg/m2/day on days 1-28 for subsequent cycles. Dose adjustment was possible in case of adverse reactions. Patients who responded to BLINCYTO but later relapsed had the option to be retreated with BLINCYTO. The treated population (in the dose-finding, PK expansion, and efficacy parts) included 70 patients who received at least 1 infusion of BLINCYTO at the recommended dose; the mean number of treatment cycles was 1.5. Among treated patients, the median age was 8 years (range: 7 months to 17 years), 40 out of 70 (57.1%) had undergone allogeneic HSCT prior to receiving BLINCYTO, and 39 out of 70 (55.7%) had refractory disease. Most patients had a high tumor burden (≥ 50% leukemic blasts in bone marrow) at baseline with a median of 75.5% bone marrow blasts. Twenty out of 70 (28.6%) patients achieved CR/CRh* within the first 2 treatment cycles with 17 out of 20 (85%) occurring within cycle 1 of treatment. Four patients achieved M1 bone marrow but did not meet the peripheral blood count recovery criteria for CR or CRh*. Eleven of the 20 patients (55%) who achieved CR/CRh* received an allogeneic HSCT. The CR/CRh* for patients less than 2 years of age was 40.0% (4/10), for patients 2 to 6 years was 30.0% (6/20); and for patients aged 7 to 17 years was 25.0% (10/40). Three patients < 1 year of age refractory to prior treatment and without prior alloHSCT received one cycle of BLINCYTO at a dose of 5-15 mcg/m2/day. None of the 3 subjects < 1 year old achieved a CR/CRh*, 1 patient had progressive disease (OS 2.3 months) and 2 were non-responders (OS 1.1 months and 8.7 months, respectively). The type of adverse reactions observed in infants were similar to those observed in the overall pediatric population. See table 12 for the efficacy results. Table 12. Efficacy results in patients < 18 years of age with relapsed or refractory B-precursor ALL (MT103-205) N = 70 CRa/CRh*b, n (%) [95% CI] 20 (28.6%) [18.4% – 40.6%] CR, n (%) [95% CI] 11 (15.7%) [8.1% – 26.4%] CRh*, n (%) [95% CI] 9 (12.9%) [6.1% – 23.0%] Complete MRD response for CR/CRh*c, n1/n2d (%) [95% CI] 11/20 (55.0%) [31.5 – 76.9] CR, n1/n2d (%) [95% CI] 6/11 (54.5%) [23.4 – 83.3] CRh*, n1/n2d (%) [95% CI] 5/9 (55.6%) [21.2 – 86.3] Median relapsee-free survival (RFS)e for CR/CRh* [95% CI] 6.8 months [2.2 to 12.0 months] Median overall survival [95% CI] 7.5 months [4.0 to 11.8 months] 100-day mortality after alloHSCTf n/N (%), [95% CI] 1/6 (16.7%) [2.5% – 72.7%] a CR was defined as M1 marrow (≤ 5% of blasts in the bone marrow), no evidence of circulating blasts or extramedullary disease, and full recovery of peripheral blood counts (platelets > 100,000/microliter and absolute neutrophil counts [ANC] > 1,000/microliter) and no relapse within 28 days. b CRh* was defined as M1 marrow (≤ 5% of blasts in the bone marrow), no evidence of circulating blasts or extramedullary disease, and partial recovery of peripheral blood counts (platelets > 50,000/microliter and ANC > 500/microliter) and no relapse within 28 days. c Complete MRD response No detectable signal for leukemic cells either by PCR or flow cytometry. d n1: number of patients who achieved MRD response and the respective remission status; n2: number of patients who achieved the respective remission status. One CR/CRh* responder with missing MRD data was considered as a MRD-non-responder. e Relapse was defined as hematological relapse (blasts in bone marrow greater than 25% following CR) or an extramedullary relapse. f Only patients with HSCT in CR/CRh* remission (with no anti-leukemia agents used prior to HSCT) are included.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of blinatumomab appear linear over a dose range from 5 to 90 mcg/m2/day (approximately equivalent to 9-162 mcg/day) in adult patients. Following continuous intravenous infusion, the steady state serum concentration (Css) was achieved within a day and remained stable over time. The increase in mean Css values was approximately proportional to the dose in the range tested. At the clinical doses of 9 mcg/day and 28 mcg/day for the treatment of relapsed or refractory ALL, the mean (SD) Css was 228 (356) pg/mL and 616 (537) pg/mL, respectively. The pharmacokinetics of blinatumomab in patients with MRD positive B-precursor ALL was similar to patients with relapsed or refractory ALL. Distribution The estimated mean (SD) volume of distribution based on terminal phase (Vz) was 4.35 (2.45) L with the continuous intravenous infusion of blinatumomab. Biotransformation The metabolic pathway of blinatumomab has not been characterized. Like other protein therapeutics, blinatumomab is expected to be degraded into small peptides and amino acids via catabolic pathways. Elimination The estimated mean (SD) systemic clearance with continuous intravenous infusion in patients receiving blinatumomab in clinical studies was 3.11 (2.98) L/hour. The mean (SD) half-life was 2.10 (1.41) hours. Negligible amounts of blinatumomab were excreted in the urine at the tested clinical doses. Body surface area, gender and age A population pharmacokinetic analysis was performed to evaluate the effects of demographic characteristics on blinatumomab pharmacokinetics. Results suggest that age (7 months to 80 years) and gender do not influence the pharmacokinetics of blinatumomab. Body surface area (0.37 to 2.70 m2) influences the pharmacokinetics of blinatumomab. However, the influence is negligible in adults and body surface area based dosing is recommended in the pediatric population. Renal impairment No formal pharmacokinetic studies of blinatumomab have been conducted in patients with renal impairment. Pharmacokinetic analyzes showed an approximately 2-fold difference in mean blinatumomab clearance values between patients with moderate renal dysfunction and normal renal function. However high inter-patient variability was discerned (CV% up to 96.8%), and clearance values in renal impaired patients were essentially within the range observed in patients with normal renal function, no clinically meaningful impact of renal function on clinical outcomes is expected. Hepatic impairment No formal pharmacokinetic studies of blinatumomab have been conducted in patients with hepatic impairment. Baseline ALT and AST levels were used to assess the effect of hepatic impairment on the clearance of blinatumomab. Population pharmacokinetic analysis suggested that there was no association between ALT or AST levels and the clearance of blinatumomab. Pediatric population The pharmacokinetics of blinatumomab appear linear over a dose range from 5 to 30 mcg/m2/day in pediatric patients with relapsed or refractory B-precursor ALL. At the recommended doses of 5 and 15 mcg/m2/day, the mean (SD) steady state concentration (Css) values were 162 (179) and 533 (392) pg/mL, respectively. The estimated mean (SD) volume of distribution (Vz), clearance (CL) and terminal half-life (t1/2,z) were 3.91 (3.36) L/m2, 1.88 (1.90) L/hr/m2 and 2.19 (1.53) hours, respectively. The pharmacokinetics of blinatumomab in patients with high-risk first relapsed B-precursor ALL was characterized with an estimated mean (SD) Css at 15 mcg/m2/day and CL were 921 (1,010) pg/mL and 0.988 (0.450) L/hr/m2, respectively; the observed values are not considered to be clinically different from those in patients with relapsed or refractory B-precursor ALL. Volume of distribution and half- life could not be estimated.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים אלה:1. חולים בגירים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL)) עמידה או חוזרת (Relapsed / Refractory).במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Blinatumomab, Inotuzumab ozogamicin, למעט בחולה אשר לא השיג תגובה מינימלית לאחר ניסיון טיפולי של מחזור טיפול אחד באחת מהתרופות האמורות.2. ילדים בני שנה ומעלה הלוקים בלוקמיה מסוג Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) עמידה או חוזרת (Relapsed / Refractory).לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה אלוגנאית של תאי גזע המטופואטיים.הטיפול לא יינתן כטיפול אחזקה.3. כמונותרפיה במבוגרים עם Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) בהפוגה ראשונה או שניה עם מחלה שארית מינימלית (MRD – minimal residual disease) בערך של 0.1% ומעלה. מחזור יחיד כחלק מטיפול קונסולידציה, בילדים חולי לוקמיה מסוג Philadelphia chromosome negative CD19 positive B-precursor ALL בסיכון גבוה, בחזרת מחלה ראשונה.לעניין זה הישנות בסיכון גבוה תוגדר כהישנות המתרחשת בתוך פחות מ-6 חודשים מסיום הטיפול הראשוני.4. מחזור יחיד כחלק מטיפול קונסולידציה, בילדים חולי לוקמיה מסוג Philadelphia chromosome negative CD19 positive B-precursor ALL בסיכון גבוה, בחזרת מחלה ראשונה.לעניין זה הישנות בסיכון גבוה תוגדר כהישנות המתרחשת בתוך פחות מ-6 חודשים מסיום הטיפול הראשוני.ב. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מונותרפיה במבוגרים עם Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) בהפוגה ראשונה או שניה עם מחלה שארית מינימלית (MRD – minimal residual disease) בערך של 0.1% ומעלה | 30/01/2020 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| חולים בגירים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL)) עמידה או חוזרת (Relapsed / Refractory). במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן - Blinatumomab, Inotuzumab ozogamicin, למעט בחולה אשר לא השיג תגובה מינימלית לאחר ניסיון טיפולי של מחזור טיפול אחד באחת מהתרופות האמורות. | 30/01/2020 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| ילדים בני שנה ומעלה הלוקים בלוקמיה מסוג Philadelphia chromosome-negative CD19+ B cell precursor acute lymphoblastic leukemia (ALL) עמידה או חוזרת (Relapsed / Refractory). | 16/01/2019 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| התרופה תינתן לטיפול בחולים בגירים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL)) עמידה או חוזרת (Relapsed / Refractory). | 12/01/2017 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| התרופה תינתן לטיפול בחולים הלוקים בלוקמיה מסוג Philadelphia chromosome-negative B cell precursor acute lymphoblastic leukemia (ALL) בחולים בגירים, בהם מתקיימים כל התנאים הבאים: א. החולה חווה חזרת מחלה במהלך השנה הראשונה שלאחר טיפול כימותרפי והשתלת מח עצם (first relapse) (עד שנה מהשתלת מח העצם). ב. החולה מועמד להשתלת מח עצם אלוגנאית (השתלה שניה). ג. בדמו של החולה נספר מספר בלסטים הנמוך מ-50%. ד. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה. | 21/01/2016 | אונקולוגיה | Acute lymphoblastic leukemia, ALL | |
| מחזור יחיד כחלק מטיפול קונסולידציה, בילדים חולי לוקמיה מסוג Philadelphia chromosome negative CD19 positive B-precursor ALL בסיכון גבוה, בחזרת מחלה ראשונה. לעניין זה הישנות בסיכון גבוה תוגדר כהישנות המתרחשת בתוך פחות מ-6 חודשים מסיום הטיפול הראשוני. | 03/02/2022 | אונקולוגיה | Acute lymphoblastic leukemia, ALL |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
21/01/2016
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
17.05.18 - עלון לצרכן 07.03.19 - עלון לצרכן 16.09.19 - עלון לצרכן 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן עברית 01.02.22 - עלון לצרכן ערבית 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן אנגלית 14.03.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן אנגלית 01.02.22 - עלון לצרכן עברית 01.02.22 - עלון לצרכן ערבית 13.03.22 - עלון לצרכן אנגלית 13.03.22 - עלון לצרכן עברית 13.03.22 - עלון לצרכן ערבית 04.09.23 - עלון לצרכן אנגלית 04.09.23 - עלון לצרכן עברית 04.09.23 - עלון לצרכן ערבית 09.06.20 - החמרה לעלון 27.04.21 - החמרה לעלון 13.03.22 - החמרה לעלון 04.09.23 - החמרה לעלון 16.11.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
בלינסייטו