Quest for the right Drug
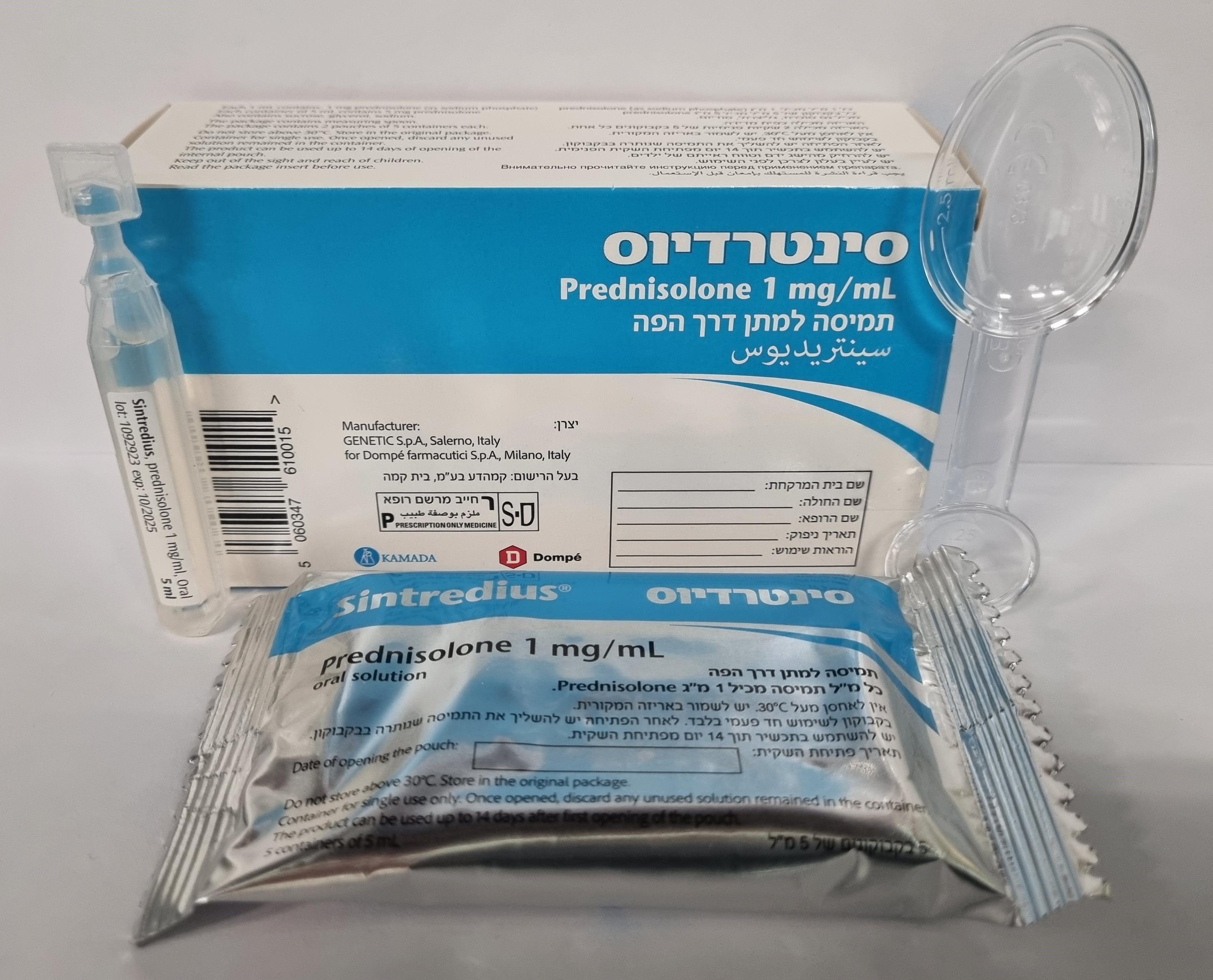
סינטרדיוס SINTREDIUS (PREDNISOLONE AS SODIUM PHOSPHATE, PREDNISOLONE SODIUM PHOSPHATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : ORAL
צורת מינון:
תמיסה : SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Data reported under this section originate from post authorization and spontaneous reporting, therefore estimation of frequency of adverse reaction could not be established. The incidence of predictable undesirable effects, including hypothalamo-pituitary- adrenal (HPA) suppression, correlates with the relative potency of the drug, dosage, timing of administration and the duration of treatment (see Section 4.4). The following side effects may be associated with the long-term systemic use of corticosteroids. Infections and Infestations Infection susceptibility increased, opportunistic infection, latent tuberculosis (see section 4.4). Neoplasms benign, malignant and unspecified (incl cysts and polyps) Kaposi's sarcoma (see section 4.4). Blood and lymphatic system disorders Leukocytosis. Immune system disorders Hypersensitivity, anaphylactic reaction. Endocrine disorders Suppression of the HPA axis. Cushingoid. Carbohydrate intolerance, diabetes mellitus exacerbated. Metabolism and nutrition disorders Sodium retention, fluid retention, hypokalaemia, hypokalaemic alkalosis, increased appetite, electrolyte imbalance, protein total abnormal Psychiatric disorders Dependence. Affective disorder: irritability, euphoric mood, depressed mood, affect lability, suicidal ideation. Psychotic disorder: mania, delusions, hallucinations, schizophrenia aggravated. Abnormal behavior, anxiety, sleep disorder. Cognitive disorder: confusion, amnesia. A wide range of psychiatric reactions including the above mentioned reactions, are common and may occur in both adults and children. In adults, the frequency of severe reactions has been estimated to be 5-6%. Psychological effects have been reported on withdrawal of corticosteroids; the frequency is unknown. Nervous system disorders Dizziness, headache, epilepsy aggravated. Intracranial pressure increased, papilloedema, epilepsy. Eye disorders Glaucoma, papilloedema, posterior subcapsular cataract, chorioretinopathy, vision, blurred (see also section 4.4), exophthalmos, corneal thinning, scleral thinning, eye infection viral, eye infection fungal. Ear and labyrinth disorders Vertigo Cardiac disorders Myocardial rupture (post infarct), cardiac failure congestive. Frequency “not known”: Bradycardia* Vascular disorders Hypertension, embolism. Respiratory, thoracic and mediastinal disorders Hiccups. Gastrointestinal disorders Dyspepsia, nausea, vomiting, abdominal distension, abdominal pain, diarrhoea, oesophageal ulcer, candidiasis, pancreatitis acute. Peptic ulcer haemorrhage, peptic ulcer perforation. Skin and subcutaneous tissue disorders Skin atrophy, skin striae, acne, telangiectasia, hyperhidrosis, rash, pruritus, urticaria, hirsutism, Stevens-Johnson syndrome. Musculoskeletal and connective tissue disorders Myopathy, osteoporosis, multiple spinal fractures, osteonecrosis, myalgia. Renal and urinary disorders Scleroderma renal crisis. Amongst the different subpopulations the occurrence of scleroderma renal crisis varies. The highest risk has been reported in patients with diffuse systemic sclerosis. The lowest risk has been reported in patients with limited systemic sclerosis (2%) and juvenile onset systemic sclerosis (1%). Reproductive system and breast disorders Menstruation irregular, amenorrhoea. Congenital, familial and genetic disorders Porphyria General disorders and administration site conditions Impaired healing, malaise. Investigations Weight increased, intraocular pressure increased. Injury, poisoning and procedural complications Tendon rupture, contusion. Withdrawal Symptoms Too rapid a reduction of corticosteroid dosage following prolonged treatment can lead to acute adrenal insufficiency, hypotension and death (See Section 4.4). A 'withdrawal syndrome' may also occur including fever, myalgia, arthralgia, rhinitis, conjunctivitis, painful itchy skin nodules and loss of weight. In some instances, withdrawal symptoms may involve or resemble a clinical relapse of the disease for which the patient has been undergoing treatment. Other effects that may occur during withdrawal or change of corticosteroid therapy include benign intracranial hypertension with headache and vomiting and papilloedema caused by cerebral oedema. Latent rhinitis or eczema may be unmasked. Pediatric population The following side effects have been reported in the pediatric population. Growth retardation in infancy, childhood and adolescence. Intracranial pressure increased with papilloedema (pseudo tumour cerebri) after treatment withdrawal. For psychiatric reactions in children, refer to the paragraph “Psychiatric disorders”. *Following high doses Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form : https://sideeffects.health.gov.il Additionally, you should also report to Kamada Ltd. to email address: pharmacovigilance@kamada.com

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
