Quest for the right Drug
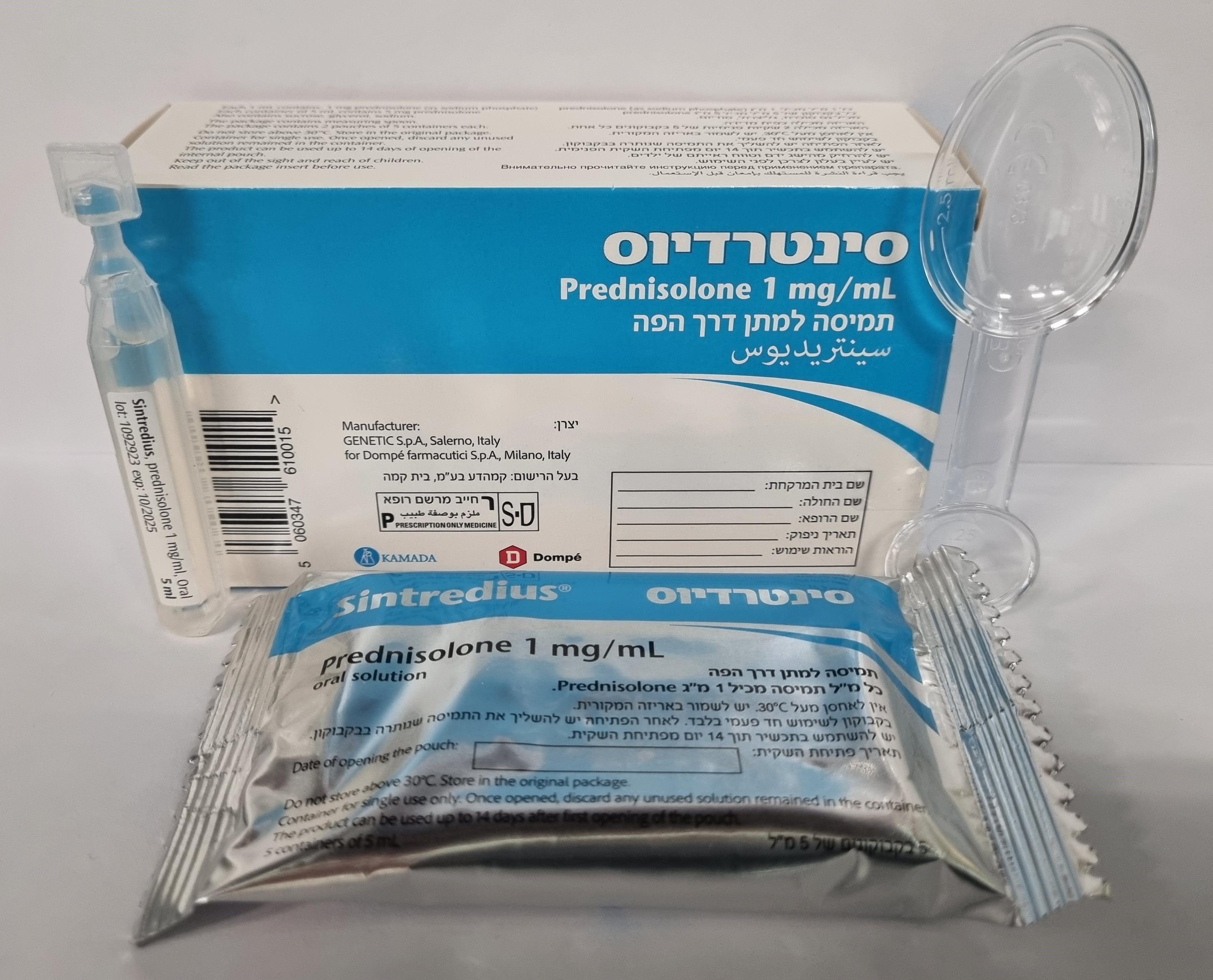
סינטרדיוס SINTREDIUS (PREDNISOLONE AS SODIUM PHOSPHATE, PREDNISOLONE SODIUM PHOSPHATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : ORAL
צורת מינון:
תמיסה : SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Adrenal cortical atrophy develops during prolonged therapy and may persist for years after stopping treatment. Withdrawal of corticosteroids after prolonged therapy must therefore always be gradual to avoid acute adrenal insufficiency, being tapered off over weeks or months according to the dose and duration of treatment. Suppression of the HPA axis and other undesirable effects may be minimized by using the lowest effective dose for the minimum period, and by administering the daily requirement as a single morning dose or whenever possible as a single morning dose on alternate days. Frequent patient review is required to appropriately titrate the dose against disease activity. (See dosage section). Suppression of the inflammatory response and immune function increases the susceptibility to infections and their severity. The clinical presentation may often be atypical and serious infections such as septicaemia and tuberculosis may be masked and may reach an advanced stage before being recognized. Chickenpox is of particular concern since this normally minor illness may be fatal in immunosuppressed patients. Patients without a definite history of chickenpox should be advised to avoid close personal contact with chickenpox or herpes zoster and if exposed they should seek urgent medical attention. If the patient is a child parents must be given the above advice. Passive immunization with varicella zoster immunoglobulin (VZIG) is needed by exposed non-immune patients who are receiving systemic corticosteroids or who have used them within the previous 3 months; this should be given within 10 days of exposure to chickenpox. If a diagnosis of chickenpox is confirmed, the illness warrants specialist care and urgent treatment. Corticosteroids should not be stopped and the dose may need to be increased. Patients should be advised to take particular care to avoid exposure to measles and to seek immediate advice if exposure occurs. Prophylaxis with intramuscular normal immunoglobulin may be needed. Live vaccines should not be given to individuals with impaired immune responsiveness caused by high doses of corticosteroids. The antibody response to other vaccines may be diminished. Kaposi's sarcoma has been reported to occur in patients receiving corticosteroid therapy. Discontinuation of corticosteroids may result in clinical remission. Because of the possibility of fluid retention, care must be taken when corticosteroids are administered to patients with renal insufficiency or hypertension or congestive heart failure. Corticosteroids may worsen diabetes mellitus, osteoporosis, hypertension, glaucoma and epilepsy and therefore patients with these conditions or a family history of them should be monitored frequently. Care is required and frequent patient monitoring necessary where there is a history of severe affective disorders (especially a previous history of steroid psychosis), previous steroid myopathy, peptic ulceration, hypothyroidism, recent myocardial infarction or patients with a history of tuberculosis. In patients with liver failure, blood levels of corticosteroid may be increased, as with other drugs which are metabolized in the liver. Frequent patient monitoring is therefore necessary. Physicians should be aware that corticoids have been reported to precipitate porphyria. As well, one case of a reversible Steven-Johnson-Syndrome (SJS) was reported in connection with prednisolone treatment. Visual disturbance Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision, or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids. Chorioretinopathy may result in impaired vision, including loss of vision. Regular checkups with doctors (including vision checkups in three month-intervals) are advised during long term treatment. At high doses, sufficient calcium intake and sodium restriction, as well as potassium levels should be monitored. Scleroderma renal crisis Caution is required in patients with systemic sclerosis because of an increased incidence of (possibly fatal) scleroderma renal crisis with hypertension and decreased urinary output observed with a daily dose of 15 mg or more prednisolone. Blood pressure and renal function (s-creatinine) should therefore be routinely checked. When renal crisis is suspected, blood pressure should be carefully controlled. Use in Children: Corticosteroids cause dose-related growth retardation in infancy, childhood and adolescence, which may be irreversible. Use in the Elderly: The common adverse effects of systemic corticosteroids may be associated with more serious consequences in old age, especially osteoporosis, hypertension, hypokalaemia, diabetes, susceptibility to infection and thinning of the skin. Close clinical supervision is required to avoid life-threatening reactions. Patients/and or carers should be warned that potentially severe psychiatric adverse reactions may occur with systemic steroids (see Section 4.8 Undesirable effects). Symptoms typically emerge within a few days or weeks of starting the treatment. Risks may be higher with high doses/systemic exposure (see also Section 4.5 Interaction with other medicinal products and other forms of interaction), although dose levels do not allow prediction of the onset, type, severity or duration of reactions. Most adverse reactions resolve after either dose reduction or withdrawal of the medicine, although specific treatment may be necessary. Patients/carers should be encouraged to seek medical advice if worrying psychological symptoms develop, especially if depressed mood or suicidal ideation is suspected. Patients/carers should also be alert to possible psychiatric disturbances that may occur either during or immediately after dose tapering/withdrawal of systemic steroids, although such reactions have been reported infrequently. Particular care is required when considering the use of systemic corticosteroids in patients with existing or a previous history of severe affective disorders in themselves or in their first degree relatives. These would include depressive or manic-depressive illness and previous steroid psychosis. Patients with rare hereditary problems of fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase insufficiency should not take this medicine. "Patients should carry 'Steroid treatment' cards which give clear guidance on the precautions to be taken to minimize risk and which provide details of prescriber, drug, dosage and the duration of treatment." Withdrawal In patients who have received more than physiological doses of systemic corticosteroids (approximately 7.5 mg prednisolone or equivalent) for greater than 3 weeks, withdrawal should not be abrupt. How dose reduction should be carried out depends largely on whether the disease is likely to relapse as the dose of systemic corticosteroids is reduced. Clinical assessment of disease activity may be needed during withdrawal. If the disease is unlikely to relapse on withdrawal of systemic corticosteroids but there is uncertainty about HPA suppression, the dose of systemic corticosteroid may be reduced rapidly to physiological doses. Once a daily dose equivalent to 7.5mg of prednisolone is reached, dose reduction should be slower to allow the HPA-axis to recover. Abrupt withdrawal of systemic corticosteroid treatment, which has continued up to 3 weeks is appropriate if it is considered that the disease is unlikely to relapse. Abrupt withdrawal of doses of up to 40mg daily of prednisolone, or equivalent for 3 weeks is unlikely to lead to clinically relevant HPA-axis suppression, in the majority of patients. In the following patient groups, gradual withdrawal of systemic corticosteroid therapy should be considered even after courses lasting 3 weeks or less: • Patients who have had repeated courses of systemic corticosteroids, particularly if taken for greater than 3 weeks, • When a short course has been prescribed within one year of cessation of long-term therapy (months or years), • Patients who may have reasons for adrenocortical insufficiency other than exogenous corticosteroid therapy, • Patients receiving doses of systemic corticosteroid greater than 40mg daily of prednisolone, • Patients repeatedly taking doses in the evening. During prolonged therapy any intercurrent illness, trauma or surgical procedure will require a temporary increase in dosage; if corticosteroids have been stopped following prolonged therapy they may need to be temporarily reintroduced.
Effects on Driving
4.7 Effects on ability to drive and use machines None known.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
