Quest for the right Drug
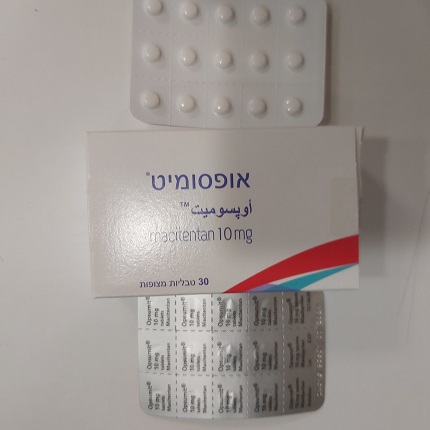
אופסומיט ® OPSUMIT ® (MACITENTAN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: anti-hypertensives, anti-hypertensives for pulmonary arterial hypertension, ATC code: C02KX04. Mechanism of action Endothelin (ET)-1 and its receptors (ET A and ET B ) mediate a variety of effects such as R R R R vasoconstriction, fibrosis, proliferation, hypertrophy, and inflammation. In disease conditions such as PAH, the local ET system is upregulated and is involved in vascular hypertrophy and in organ damage. Macitentan is an orally active potent endothelin receptor antagonist, active on both ET A and R R ET B receptors and approximately 100-fold more selective for ET A as compared to ET B in R R R R R R vitro. Macitentan displays high affinity and sustained occupancy of the ET receptors in human pulmonary arterial smooth muscle cells. This prevents endothelin-mediated activation of second messenger systems that result in vasoconstriction and smooth muscle cell proliferation. Opsumit_PI_EUPI update_January-2023 Clinical efficacy and safety Efficacy in patients with pulmonary arterial hypertension A multicenter, double-blind, placebo-controlled, parallel-group, event-driven, Phase 3 outcome study (AC-055-302/SERAPHIN) was conducted in 742 patients with symptomatic PAH, who were randomised to three treatment groups (placebo [N = 250], 3 mg [N = 250] or 10 mg [N = 242] of macitentan once daily), to assess the long-term effect on morbidity or mortality. At baseline, the majority of enrolled patients (64%) were treated with a stable dose of specific therapy for PAH, either oral phosphodiesterase inhibitors (61%) and/or inhaled/oral prostanoids (6%). The primary endpoint was the time to first occurrence of a morbidity or mortality event, up to the end of double-blind treatment, defined as death, or atrial septostomy, or lung transplantation, or initiation of intravenous (i.v.) or subcutaneous (s.c.) prostanoids, or other worsening of PAH. Other worsening of PAH was defined as the presence of all of the three following components: a sustained decrease in 6-minute walk distance (6MWD) of at least 15% from baseline; worsening of PAH symptoms (worsening of WHO FC or right heart failure); and need for new treatment for PAH. All events were confirmed by an independent adjudication committee, blinded to treatment allocation. All patients were followed up to end-of-study (EOS) for vital status. EOS was declared when the predefined number of primary endpoint events was reached. In the period between end- of-treatment (EOT) and EOS, patients could receive open-label macitentan 10 mg or alternative PAH therapy. The overall median double-blind treatment duration was 115 weeks (up to a maximum of 188 weeks on macitentan). The mean age of all patients was 46 years (range 12–85 years of age, including 20 patients below 18, 706 patients between 18–74 years, and 16 patients aged 75 and older) with the majority of subjects being Caucasian (55%) and female (77%). Approximately 52%, 46%, and 2% of patients were in WHO FC II, III, and IV, respectively. Idiopathic or heritable PAH was the most common aetiology in the study population (57%), followed by PAH due to connective tissue disorders (31%), PAH associated with corrected simple congenital heart disease (8%), and PAH associated with other aetiologies (medicinal products and toxins [3%] and HIV [1%]). Outcome endpoints Treatment with macitentan 10 mg resulted in a 45% risk reduction (hazard ratio [HR] 0.55; 97.5% CI: 0.39 to 0.76; logrank p < 0.0001) of the composite morbidity-mortality endpoint up to EOT when compared to placebo [Figure 1 and Table 1]. The treatment effect was established early and was sustained. Efficacy of macitentan 10 mg on the primary endpoint was consistent across subgroups of age, sex, ethnic origin, geographical region, aetiology, by monotherapy or in combination with another PAH therapy and by WHO FC (I/II and III/IV). Opsumit_PI_EUPI update_January-2023 Figure 1 Kaplan-Meier estimates of the first morbidity-mortality event in SERAPHIN Table 1 Summary of outcome events Patients with events Treatment comparison: macitentan 10 mg vs placebo Endpoints Placebo Relative & Macitentan Absolute (N = 250) risk HR a Logrank statistics 10 mg risk P reduction (97.5% CI) p-value (N = 242) reduction (97.5% CI) Morbidity- 45% 0.55 mortality 53% 37% 16% (24%; (0.39; < 0.0001 event b P 61%) 0.76) 36% 0.64 Death c 19 (7.6%) 14 (5.8%) 2% (−42%; (0.29; 0.20 P n (%) 71%) 1.42) Worsening of PAH 93 (37.2%) 59 (24.4%) 13% 49% 0.51 P n (%) (27%, i.v./s.c. (0.35; < 0.0001 65%) prostanoid 0.73) 6 (2.4%) 1 (0.4%) 2% initiation n (%) a P = based on Cox’s Proportional Hazards Model P b P = % of patients with an event at 36 months = 100 × (1 - KM estimate) P c P = all cause death up to EOT regardless of prior worsening P The number of deaths of all causes up to EOS on macitentan 10 mg was 35 versus 44 on placebo (HR 0.77; 97.5% CI: 0.46 to 1.28). The risk of PAH related death or hospitalisation for PAH up to EOT was reduced by 50% (HR 0.50; 97.5% CI: 0.34 to 0.75; logrank p < 0.0001) in patients receiving macitentan 10 mg (50 events) compared to placebo (84 events). At 36 months, 44.6% of patients on placebo and Opsumit_PI_EUPI update_January-2023 29.4% of patients on macitentan 10 mg (Absolute Risk Reduction = 15.2%) had been hospitalised for PAH or died from a PAH-related cause. Symptomatic endpoints Exercise capacity was evaluated as a secondary endpoint. Treatment with macitentan 10 mg at Month 6 resulted in a placebo-corrected mean increase in 6MWD of 22 meters (97.5% CI: 3 to 41; p = 0.0078). Evaluation of 6MWD by functional class resulted in a placebo-corrected mean increase from baseline to Month 6 in FC III/IV patients of 37 meters (97.5% CI: 5 to 69) and in FC I/II of 12 meters (97.5% CI: −8 to 33). The increase in 6MWD achieved with macitentan was maintained for the duration of the study. Treatment with macitentan 10 mg at Month 6 led to a 74% higher chance of WHO FC improvement relative to placebo (risk ratio 1.74; 97.5% CI: 1.10 to 2.74; p = 0.0063). Macitentan 10 mg improved quality of life assessed by the SF-36 questionnaire. Haemodynamic endpoints Haemodynamic parameters were assessed in a subset of patients (placebo [N = 67], macitentan 10 mg [N = 57]) after 6 months of treatment. Patients treated with macitentan 10 mg achieved a median reduction of 36.5% (97.5% CI: 21.7 to 49.2%) in pulmonary vascular resistance and an increase of 0.58 L/min/m2 (97.5% CI: 0.28 to 0.93 L/min/m2) in P P P P cardiac index compared to placebo. Long-term data in PAH In long-term follow-up of 242 patients who were treated with macitentan 10 mg in the double- blind (DB) phase of the SERAPHIN study, 182 of which continued with macitentan in the open-label (OL) extension study (SERAPHIN OL) (DB/OL cohort), Kaplan-Meier estimates of survival at 1, 2, 5, 7 and 9 years were 95%, 89%, 73%, 63% and 53%, respectively. The median follow-up time was 5.9 years.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of macitentan and its active metabolite have mainly been documented in healthy subjects. Exposure to macitentan in patients with PAH was approximately 1.2-fold greater than in healthy subjects. The exposure to the active metabolite in patients, which is approximately 5-fold less potent than macitentan, was approximately 1.3-fold higher than in healthy subjects. The pharmacokinetics of macitentan in PAH patients were not influenced by the severity of the disease. After repeated administration, the pharmacokinetics of macitentan are dose-proportional up to and including 30 mg. Absorption Maximum plasma concentrations of macitentan are achieved about 8 hours after administration. Thereafter, plasma concentrations of macitentan and its active metabolite decrease slowly, with an apparent elimination half-life of approximately 16 hours and 48 hours, respectively. In healthy subjects, the exposure to macitentan and its active metabolite is unchanged in the presence of food and, therefore, macitentan may be taken with or without food. Opsumit_PI_EUPI update_January-2023 Distribution Macitentan and its active metabolite are highly bound to plasma proteins (> 99%), primarily to albumin and to a lesser extent to alpha1-acid glycoprotein. Macitentan and its active metabolite ACT-132577 are well distributed into tissues as indicated by an apparent volume of distribution (Vss/F) of approximately 50 L and 40 L for macitentan and ACT-132577, respectively. Biotransformation Macitentan has four primary metabolic pathways. Oxidative depropylation of the sulfamide yields a pharmacologically active metabolite. This reaction is dependent on the cytochrome P450 system, mainly CYP3A4 (approximately 99%) with minor contributions of CYP2C8, CYP2C9 and CYP2C19. The active metabolite circulates in human plasma and may contribute to the pharmacological effect. Other metabolic pathways yield products without pharmacological activity. For these pathways, CYP2C9 plays a predominant role with minor contributions from CYP2C8, CYP2C19 and CYP3A4. Elimination Macitentan is only excreted after extensive metabolism. The major excretion route is via urine, accounting for about 50% of the dose. Special populations There is no clinically relevant effect of age, sex or ethnic origin on the pharmacokinetics of macitentan and its active metabolite. Renal impairment Exposure to macitentan and its active metabolite was increased by 1.3- and 1.6-fold, respectively, in patients with severe renal impairment. This increase is not considered clinically relevant (see sections 4.2 and 4.4). Hepatic impairment Exposure to macitentan was decreased by 21%, 34%, and 6% and, for the active metabolite by 20%, 25%, and 25% in subjects with mild, moderate or severe hepatic impairment, respectively. This decrease is not considered clinically relevant (see sections 4.2 and 4.4).

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול בחולה המוגדר ב-NYHA (New York Heart Association) כ-Class III ומעלה הסובל מיתר לחץ דם ריאתי עורקי. ב. התחלת הטיפול בתרופה האמורה תהיה על פי הוראתו של מנהל מחלקה בבית חולים שהוא מומחה למחלות ריאה או מומחה בקרדיולוגיה או מומחה בטיפול נמרץ כללי או מומחה בכירורגית כלי דם או מומחה בקרדיולוגית ילדים או מומחה במחלות ריאה ילדים או מומחה בטיפול נמרץ ילדים או מומחה בראומטולוגיה. ג. המשך הטיפול בתרופה האמורה ייעשה על פי מרשם של מומחה למחלות ריאה או מומחה בקרדיולוגיה או מומחה בטיפול נמרץ כללי או מומחה בכירורגית כלי דם או מומחה בקרדיולוגית ילדים או מומחה במחלות ריאה ילדים או מומחה בטיפול נמרץ ילדים או מומחה בראומטולוגיה. ד. ניתן להתחיל טיפול בתרופה האמורה במקרה בו התנגודת הריאתית המחושבת תישאר גבוהה אחרי טסט פרמקולוגי וזאת כאשר החולה סובל מ-NYHA Class III ומעלה ובעל מרחק הליכה ל-6 דקות הנמוך מ-400 מטרים ב-2 בדיקות עוקבות.ה. יש להימנע משילובי תרופות אלא לטפל בכל פעם בתרופה בודדת ורק עם כישלון בטיפול בה, לעבור לטיפול בתרופה אחרת, למעט המצבים הבאים: 1. בכישלון של טיפול ב-Sildenafil ניתן להוסיף במקרים נבחרים Iloprost באינהלציה או Selexipag או Bosentan או Ambrisentan או Macitentan.2. בכישלון של טיפול ב-Bosentan או Ambrisentan או Macitentan ניתן להוסיף במקרים נבחרים Iloprost באינהלציה או Selexipag או Sildenafil3. בכישלון של טיפול משולב ב- Bosentan או Ambrisentan או Macitentan עם Sildenafil או Tadalafil ניתן להוסיף במקרים נבחרים Selexipag. 4. השילוב של Epoprostenol או Treprostinil עם Ambrisentan או Macitentan או Bosentan או Sildenafil יעשה רק לאחר כישלון של אחד מהפרוסטציקלינים האמורים כטיפול בודד.5. השילוב של תרופה ממשפחת ה-Endothelin receptor antagonists (Ambrisentan או Macitentan או Bosentan) עם תרופה ממשפחת מעכבי PDE5 (Sildenafil או Tadalafil) יתאפשר כטיפול ראשוני (Upfront) עבור חולי יתר לחץ דם ריאתי עורקי, Group 1, שטרם קיבלו טיפול למחלתם.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| Pulmonary hypertension | AMBRISENTAN, BOSENTAN, MACITENTAN |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
28.02.19 - עלון לצרכן 13.09.20 - עלון לצרכן אנגלית 26.08.21 - עלון לצרכן עברית 13.09.20 - עלון לצרכן ערבית 21.12.22 - עלון לצרכן 03.01.23 - עלון לצרכן אנגלית 03.01.23 - עלון לצרכן עברית 03.01.23 - עלון לצרכן ערבית 11.05.23 - עלון לצרכן אנגלית 01.03.23 - עלון לצרכן עברית 11.05.23 - עלון לצרכן ערבית 01.02.16 - החמרה לעלון 26.08.21 - החמרה לעלון 03.01.23 - החמרה לעלון 01.03.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אופסומיט ®