Quest for the right Drug
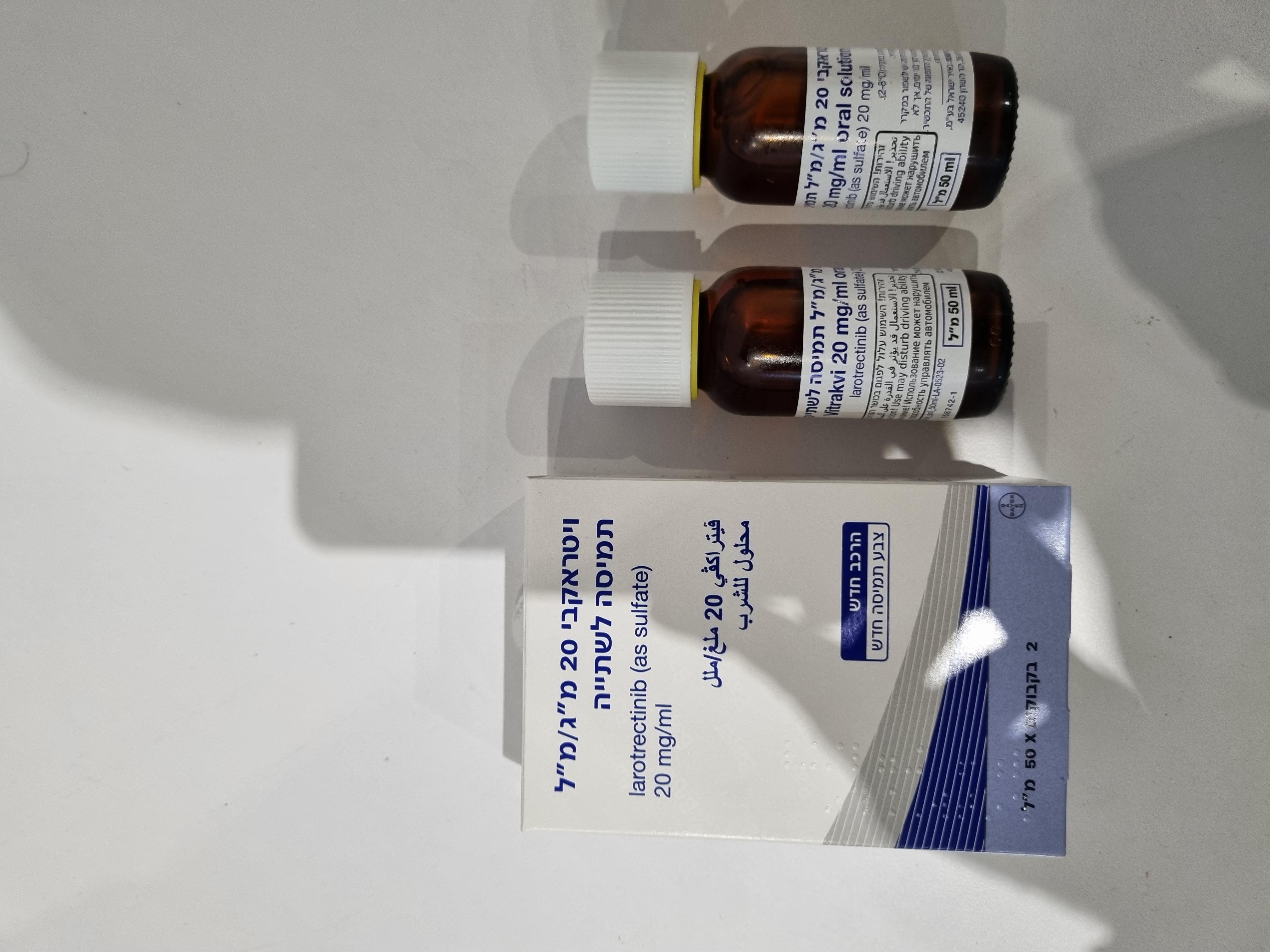
ויטראקבי 20 מ"ג/מ"ל תמיסה לשתיה VITRAKVI 20 MG/ML ORAL SOLUTION (LAROTRECTINIB AS SULFATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
תמיסה (פומי) : SOLUTION (ORAL)
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic and immunomodulating agents, antineoplastic agents, protein kinase inhibitors, ATC code: L01EX12. Mechanism of action Larotrectinib is an adenosine triphosphate (ATP)-competitive and selective tropomyosin receptor kinase (TRK) inhibitor that was rationally designed to avoid activity with off-target kinases. The target for larotrectinib is the TRK family of proteins inclusive of TRKA, TRKB, and TRKC that are encoded by NTRK1, NTRK2 and NTRK3 genes, respectively. In a broad panel of purified enzyme assays, larotrectinib inhibited TRKA, TRKB, and TRKC with IC50 values between 5-11 nM. The only other kinase activity occurred at 100-fold higher concentrations. In in vitro and in vivo tumour models, larotrectinib demonstrated anti-tumour activity in cells with constitutive activation of TRK proteins resulting from gene fusions, deletion of a protein regulatory domain, or in cells with TRK protein overexpression. In-frame gene fusion events resulting from chromosomal rearrangements of the human genes NTRK1, NTRK2, and NTRK3 lead to the formation of oncogenic TRK fusion proteins. These resultant novel chimeric oncogenic proteins are aberrantly expressed, driving constitutive kinase activity subsequently activating downstream cell signalling pathways involved in cell proliferation and survival leading to TRK fusion-positive cancer. Acquired resistance mutations after progression on TRK inhibitors have been observed. Larotrectinib had minimal activity in cell lines with point mutations in the TRKA kinase domain, including the clinically identified acquired resistance mutation, G595R. Point mutations in the TRKC kinase domain with clinically identified acquired resistance to larotrectinib include G623R, G696A, and F617L. The molecular causes for primary resistance to larotrectinib are not known. It is therefore not known if the presence of a concomitant oncogenic driver in addition to an NTRK gene fusion affects the efficacy of TRK inhibition. The measured impact of any concomitant genomic alterations on larotrectinib efficacy is provided below (see clinical efficacy). Pharmacodynamic effect Cardiac electrophysiology In 36 healthy adult subjects receiving single doses ranging from 100 mg to 900 mg, VITRAKVI did not prolong the QT interval to any clinically relevant extent. The 200 mg dose corresponds to a peak exposure (Cmax) similar to that observed with larotrectinib 100 mg BID at steady state. A shortening of QTcF was observed with VITRAKVI dosing, with a maximum mean effect observed between 3 and 24 hours after Cmax, with a geometric mean decrease in QTcF from baseline of -13.2 msec (range -10 to -15.6 msec). Clinical relevance of this finding has not been established. Clinical efficacy Overview of studies The efficacy and safety of VITRAKVI were studied in three multicentre, open-label, single-arm clinical studies in adult and paediatric cancer patients (Table 4). The studies are still ongoing Patients with and without documented NTRK gene fusion were allowed to participate in Study 1 and Study 3 (“SCOUT”). Patients enrolled to Study 2 (“NAVIGATE”) were required to have TRK fusion-positive cancer. The pooled primary analysis set of efficacy includes 272 patients with TRK fusion-positive cancer enrolled across the three studies that had measurable disease assessed by RECIST v1.1, a non-CNS primary tumour and received at least one dose of larotrectinib as of July 2022. These patients were required to have received prior standard therapy appropriate for their tumour type and stage of disease or who, in the opinion of the investigator, would have had to undergo radical surgery (such as limb amputation, facial resection, or paralysis causing procedure), or were unlikely to tolerate, or derive clinically meaningful benefit from available standard of care therapies in the advanced disease setting. The major efficacy outcome measures were overall response rate (ORR) and duration of response (DOR), as determined by a blinded independent review committee (BIRC). In addition, 41 patients with primary CNS tumours and measurable disease at baseline were treated in Study 2 (“NAVIGATE”) and in Study 3 (“SCOUT”). Forty of the 41 primary CNS tumour patients had received prior cancer treatment (surgery, radiotherapy and/or previous systemic therapy). Tumour responses were assessed by the investigator using RANO or RECIST v1.1 criteria. Identification of NTRK gene fusions relied on tissue samples for the molecular test methods: next generation sequencing (NGS) used in 276 patients, polymerase chain reaction (PCR) used in 14 patients, fluorescence in situ hybridization (FISH) used in 18 patients, and other testing methods (Sequencing, Nanostring, Sanger sequencing, or Chromosome Microarray) used in 5 patients. Table 4: Clinical studies contributing to the efficacy analyses in solid and primary CNS tumours Study name, design and patient Dose and Tumour types included in n population formulation efficacy analysis Study 1 Doses up to 200 mg Thyroid (n=4) 13 NCT02122913 once or twice daily Salivary gland (n=3) (25 mg, 100 mg GIST (n=2)a • Phase 1, open-label, dose escalation capsules or 20 mg/mL Soft tissue sarcoma (n=2) and expansion study; expansion phase oral solution) NSCLC (n=1)b,c required tumours with an NTRK gene fusion Unknown primary cancer • Adult patients (≥ 18 years) with (n=1) advanced solid tumours with an NTRK gene fusion Study 2 “NAVIGATE” 100 mg twice daily Soft tissue sarcoma NCT02576431 (25 mg, 100 mg (n=27) capsules or 20 mg/mL Thyroid (n=25)b 179 • Phase 2 multinational, open label, oral solution) NSCLC (n=24)b, c tumour “basket” study Salivary gland (n=22) • Adult and paediatric patients Colon (n=18) ≥ 12 years with advanced solid Primary CNS (n=15) tumours with an NTRK gene fusion Melanoma (n=8)b Pancreas (n=6) Breast, non-secretory (n=6)b Breast, secretory (n=4) Cholangiocarcinoma (n=4) GIST (n=3)a Prostate (n=2) Appendix, Atypical carcinoid lung cancer, Bone sarcoma , Cervix, Hepatice Duodenal, External auditory canalb, Gastric, Oesophageal, SCLCb, d, Rectal, Thymus, Unknown primary cancer, Urothelial, Uterus (n=1 each) Study 3 “SCOUT” Doses up to Infantile fibrosarcoma 121 NCT02637687 100 mg/m2 twice daily (n=49) (25 mg, 100 mg Soft tissue sarcoma (n=39)b • Phase 1/2 multinational, open-label, capsules or 20 mg/mL Primary CNS (n=26) dose escalation and expansion study; oral solution) Congenital mesoblastic Phase 2 expansion cohort required nephroma (n=2) advanced solid tumours with an NTRK Bone sarcoma (n=2) gene fusion, including locally Thyroid (n=1) Melanoma advanced infantile fibrosarcoma (n=1) • Paediatric patients ≥ 1 month to Breast, secretory 21 years with advanced cancer or with (n=1) primary CNS tumours Total number of patients (n)* 313 * consist of 272 patients with IRC tumour response assessment and 41 patients with primary CNS tumours (including astrocytoma, ganglioglioma, glioblastoma, glioma, glioneuronal tumours, neuronal and mixed neuronal-glial tumours, and primitive neuro-ectodermal tumour, not specified) with investigator tumour response assessment a GIST: gastrointestinal stromal tumour b brain metastases were observed in some patients in the following tumour types: lung ( NSCLC, SCLC), thyroid, melanoma, breast (non-secretory) , external auditory canal, and soft tissue sarcoma c NSCLC: non-small cell lung cancer d SCLC: small cell lung cancer e hepatocellular carcinoma Baseline characteristics for the pooled 272 patients with solid tumours with an NTRK gene fusion were as follows: median age 41 years (range 0-90 years); 35% < 18 years of age, and 65% ≥ 18 years; 57% white and 49% male; and ECOG PS 0-1 (89%), 2 (9%), or 3 (2%). Ninety-two percent of patients had received prior treatment for their cancer, defined as surgery, radiotherapy, or systemic therapy. Of these, 72% had received prior systemic therapy with a median of 1 prior systemic treatment regimen. Twenty-six percent of all patients had received no prior systemic therapy. Of those 272 patients the most common tumour types represented were soft tissue sarcoma (25%), infantile fibrosarcoma (18%), thyroid cancer (11%), lung cancer (10%), and salivary gland tumour (9%). Baseline characteristics for the 41 patients with primary CNS tumours with an NTRK gene fusion assessed by investigator were as follows: median age 11 years (range 1-79 years); 28 patients < 18 years of age, and 13 patients ≥ 18 years, and 28 patients white and 20 patients male; and ECOG PS 0-1 (36 patients), or 2 (4 patients). Forty (98%) patients had received prior treatment for their cancer, defined as surgery, radiotherapy, or systemic therapy. There was a median of 1 prior systemic treatment regimen received. Efficacy results The pooled efficacy results for overall response rate, duration of response and time to first response, in the primary analysis population (n=272) and with post-hoc addition of primary CNS tumours (n=41) resulting in the pooled population (n=313), are presented in Table 5 and Table 6. Table 5: Pooled efficacy results in solid tumours including and excluding primary CNS tumours Efficacy parameter Analysis in solid Analysis in solid tumours excluding tumours including primary CNS tumours primary CNS tumours (n=272)a (n=313)a, b Overall response rate (ORR) % (n) 67% (182) 61% (191) [95% CI] [61, 72] [55, 66] Complete response (CR) 23% (62) 20% (63) c Pathological complete response 5% (13) 4% (13) Partial response (PR) 39% (107) 37% (115) Time to first response (median, months) 1.84 1.84 [range] [0.89, 22.90] [0.89, 22.90] Duration of response (median, months) 43.3 41.5 [range] [0.0+, 65.4+] [0.0+, 65.4+] % with duration ≥ 12 months 80% 79% % with duration ≥ 24 months 66% 64% % with duration ≥ 36 months 54% 52% + denotes ongoing a Independent review committee analysis by RECIST v1.1 for solid tumours except primary CNS tumours (272 patients). b Investigator assessment using either RANO or RECIST v1.1 criteria for primary CNS tumours (41 patients). c A pathological CR was a CR achieved by patients who were treated with larotrectinib and subsequently underwent surgical resection with no viable tumour cells and negative margins on post-surgical pathology evaluation. The pre-surgical best response for these patients was reclassified pathological CR after surgery following RECIST v.1.1 Table 6: Overall response rate and duration of response by tumour type* Patients ORRa DO Tumour type (n=313 R months Range % 95% CI ≥ 12 ≥ 24 ≥ 36 (months) 55%, 49% 0.03+, Soft tissue sarcoma 68 68% 78% 84% 70% 65.5 Infantile 53% 49 92% 80%, 98% 80% 60% 1.6+, 64.2+ fibrosarcoma 50% Primary CNS 41 22% 11%, 38% 60% 50% 3.5, 39.4+ Thyroid 30 63% 44%, 80% 89% 65% 54% 3.7+, 64.3+ Lung 27 74% 54% 72% 56% 42% 1.9+, 45.1+ 89% Salivary gland 25 84% 64%, 95% 90% 86% 74 7.4, 59.1+ % Colon 18 50% 26%, 74% 86% 43% 5.2, 39.4 86% Breast 11 Non-secretoryc 12% 67% 7.4 6 50% 67% 67% 88% 45.3+ NR 11.1+, Secretoryb 5 80% 28%, 99% 75% 75% 31.5 Melanoma NR 1.9+, 23.2+ 9 44% 14% 50% NR 79% Pancreas 0% 5.8, 5.8 6 17 0%, 64% 0% 0% Gastrointestinal 38% 9.5, 5 80% 28%, 99% 75% 38% stromal tumour 50.4+ Bone sarcoma 3 33% 1%, 91% 0% 0% 0% 9.5, 9.5 Congenital 100% 100 mesoblastic 2 100% 16%, 100% 100% 29.4+, 44.5 % nephroma DOR: duration of response NR: not reached * no data are available for the following tumour types: cholangiocarcinoma (n=4); prostate, unknown primary cancer (n=2 each); appendix, cervix, hepatic, duodenal, external auditory canal, gastric, oesophageal, rectal, thymus, urothelial, uterus (n=1 each) + denotes ongoing response a evaluated per independent review committee analysis by RECIST v1.1 for all tumour types except patients with a primary CNS tumour who were evaluated per investigator assessment using either RANO or RECIST v1.1 criteria b with 3 complete, 1 partial response c with 1 complete, 2 partial response Due to the rarity of TRK fusion-positive cancer, patients were studied across multiple tumour types with a limited number of patients in some tumour types, causing uncertainty in the ORR estimate per tumour type. The ORR in the total population may not reflect the expected response in a specific tumour type. In the adult sub-population (n=178), the ORR was 58%. In the paediatric sub-population (n=94), the ORR was 84%. In 238 patients with wide molecular characterisation before larotrectinib treatment, the ORR in 218 patients who had other genomic alterations in addition to NTRK gene fusion was 52%, and in 110 patients without other genomic alterations ORR was 76%. Pooled primary analysis set The pooled primary analysis set consisted of 272 patients and did not include primary CNS tumours. Median time on treatment before disease progression was 19.6 months (range: 0.10 to 75.2 months) based on July 2022 cut-off. Fifty seven percent of patients had received VITRAKVI for 12 months or more, 34% had received VITRAKVI 24 months or more, and 21% had received VITRAKVI 36 months or more, with follow-up ongoing at the time of the analysis. At the time of analysis, the median duration of response is 43.3 months (range: 0.0+ to 65.4+), an estimated 80% [95% CI: 74, 86] of responses lasted 12 months or longer, 66% [95% CI: 58, 74] of responses lasted 24 months or longer, and 51% [95% CI:42, 60] of responses lasted 36 months or longer. Eighty-six percent (86%) [95% CI: 82, 90] of patients treated were alive one year after the start of therapy 77% [95% CI: 72, 82] after two years after the start of therapy, and 72% [95% CI: 66, 78] after three years with the median for overall survival not yet being reached. Median progression free survival was 30.8 months at the time of the analysis, with a progression free survival rate of 65% [95% CI: 59, 71] after 1 year 56% [95% CI: 49, 62] after 2 years, and 43% [95% CI: 36, 50] after 3 years. The median change in tumour size in the pooled primary analysis set was a decrease of 79%. Patients with primary CNS tumours At the time of data cut-off, of the 41 patients with primary CNS tumours confirmed response was observed in 9 patients (22%) with 1 of the 41 patients (2%) being complete responders and 8 patients (20%) being partial responders. Further 20 patients (49%) had stable disease. Twelve patients (29%) had progressive disease. At the time of data cut-off, time on treatment ranged from 1.7 to 50.9 months and was ongoing in 13 out of 41 patients with one of these patients receiving post-progression treatment.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties In cancer patients given VITRAKVI capsules, peak plasma levels (Cmax) of larotrectinib were achieved at approximately 1 hour after dosing. Half-life (t½) is approximately 3 hours and steady state is reached within 8 days with a systemic accumulation of 1.6 fold. At the recommended dose of 100 mg taken twice daily, steady-state arithmetic mean (± standard deviation) Cmax and daily AUC in adults were 914 ± 445 ng/mL and 5410 ± 3813 ng*h/mL, respectively. In vitro studies indicate that larotrectinib is not a substrate for either OATP1B1 or OATP1B3. In vitro studies indicate that larotrectinib does not inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP2D6 at clinically relevant concentrations and is unlikely to affect clearance of substrates of these CYPs. In vitro studies indicate that larotrectinib does not inhibit the transporters BCRP, P-gp, OAT1, OAT3, OCT1, OCT2, OATP1B3, BSEP, MATE1 and MATE2-K at clinically relevant concentrations and is unlikely to affect clearance of substrates of these transporters. Absorption VITRAKVI is available as a capsule and oral solution formulation. The mean absolute bioavailability of larotrectinib was 34% (range: 32% to 37%) following a single 100 mg oral dose. In healthy adult subjects, the AUC of larotrectinib in the oral solution formulation was similar to the capsule, with Cmax 36% higher with the oral solution formulation. Larotrectinib Cmax was reduced by approximately 35% and there was no effect on AUC in healthy subjects administered VITRAKVI after a high-fat and high-calorie meal compared to the Cmax and AUC after overnight fasting. Effect of gastric pH-elevating agents on larotrectinib Larotrectinib has pH-dependent solubility. In vitro studies show that in liquid volumes relevant to the gastrointestinal (GI) tract larotrectinib is fully soluble over entire pH range of the GI tract. Therefore, larotrectinib is unlikely to be affected by pH-modifying agents. Distribution The mean volume of distribution of larotrectinib in healthy adult subjects was 48 L following intravenous administration of an IV microtracer in conjunction with a 100 mg oral dose. Binding of larotrectinib to human plasma proteins in vitro was approximately 70% and was independent of drug concentration. The blood-to-plasma concentration ratio was approximately 0.9. Biotransformation Larotrectinib was metabolised predominantly by CYP3A4/5 in vitro. Following oral administration of a single 100 mg dose of radiolabeled larotrectinib to healthy adult subjects, unchanged larotrectinib (19%) and an O-glucuronide that is formed following loss of the hydroxypyrrolidine-urea moiety (26%) were the major circulating radioactive drug components. Elimination The half-life of larotrectinib in plasma of cancer patients given 100 mg twice daily of VITRAKVI was approximately 3 hours. Mean clearance (CL) of larotrectinib was approximately 34 L/h following intravenous administration of an IV microtracer in conjunction with a 100 mg oral dose of VITRAKVI. Excretion Following oral administration of 100 mg radiolabeled larotrectinib to healthy adult subjects, 58% of the administered radioactivity was recovered in faeces and 39% was recovered in urine and when an IV microtracer dose was given in conjunction with a 100 mg oral dose of larotrectinib, 35% of the administered radioactivity was recovered in faeces and 53% was recovered in urine. The fraction excreted as unchanged drug in urine was 29% following IV microtracer dose, indicating that direct renal excretion accounted for 29% of total clearance. Linearity / non-linearity The area under the plasma concentration-time curve (AUC) and maximum plasma concentration (Cmax) of larotrectinib after a single dose in healthy adult subjects were dose proportional up to 400 mg and slightly greater than proportional at doses of 600 to 900 mg. Special populations Paediatric patients Based on population pharmacokinetic analyses exposure (Cmax and AUC) in paediatric patients at the recommended dose of 100 mg/m2 with a maximum of 100 mg BID was higher than in adults (≥18 years of age) given the dose of 100 mg BID (see Table 7). Data defining exposure in small children (1 month to <2 years of age) at the recommended dose is limited (n=40). Table 7: Exposure (Cmax and AUC on day 1a) in patients grouped by age group at the recommended dose of 100 mg/m2 with a maximum of 100 mg BID Fold difference compared to patients ≥ 18 years of agec Age group n=348b Cmax AUCa 1 to < 3 months 9 4.2 4.5 3 to < 6 months 4 2.6 2.5 6 to < 12 months 18 2.5 1.9 1 to < 2 years 9 2.0 1.4 2 to < 6 years 31 2.0 1.4 6 to < 12 years 26 1.5 1.2 12 to < 18 years 27 1.2 1.0 ≥ 18 years 224 1.0 1.0 a area under the plasma concentration-time curve for 24 hours on day 1 b number of patients from 26 November 2020 data cut-off c fold difference is the ratio of stated age group to ≥18 years group. A fold-difference of 1 equates to no difference. Elderly There are limited data in elderly. PK data is available only in 2 patients over 65 years. Patients with hepatic impairment A pharmacokinetic study was conducted in subjects with mild (Child-Pugh A), moderate (Child-Pugh B) and severe (Child-Pugh C) hepatic impairment, and in healthy adult control subjects with normal hepatic function matched for age, body mass index and sex. All subjects received a single 100 mg dose of larotrectinib. An increase in larotrectinib AUC0-inf was observed in subjects with mild, moderate and severe hepatic impairment of 1.3, 2 and 3.2-fold respectively versus those with normal hepatic function. Cmax was observed to increase slightly by 1.1, 1.1 and 1.5-fold respectively. Patients with renal impairment A pharmacokinetic study was conducted in subjects with end stage renal disease requiring dialysis, and in healthy adult control subjects with normal renal function matched for age, body mass index and sex. All subjects received a single 100 mg dose of larotrectinib. An increase in larotrectinib Cmax and AUC0-inf, of 1.25 and 1.46-fold respectively was observed in renally impaired subjects versus those with normal renal function. Other special populations Gender did not appear to influence larotrectinib pharmacokinetics to a clinically significant extent. There was not enough data to investigate the potential influence of race on the systemic exposure of larotrectinib.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. חולים עם ממאירות סולידית עם איחוי גני מסוג NTRK, שמחלתם מתקדמת מקומית או גרורתית והם מיצו את אופציות הטיפול האפשריות למחלתם.2. טיפול קו ראשון עבור חולים עם ממאירות סולידית עם איחוי גני מסוג NTRK במקרים האלה:א. Infantile fibrosarcoma;ב. Congenital mesoblastic nephroma, לא נתיחה או גרורתית;ג. Infant high grade glioma (HGG).ב. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת מעכבי NTRK.ג. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או באונקולוגיה ילדים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התרופה תינתן לטיפול בילדים עם ממאירות סולידית עם איחוי גני מסוג NTRK, שמחלתם מתקדמת מקומית או גרורתית והם מיצו את אופציות הטיפול האפשריות למחלתם. ב. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת מעכבי NTRK. ג. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או באונקולוגיה ילדים. | 01/03/2021 | אונקולוגיה | ||
| א. התרופה תינתן לטיפול בילדים עם ממאירות סולידית עם איחוי גני מסוג NTRK, שמחלתם מתקדמת מקומית או גרורתית והם מיצו את אופציות הטיפול האפשריות למחלתם. ב. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה ילדים. | 30/01/2020 | אונקולוגיה | ||
| א. התרופה תינתן לטיפול במקרים האלה: 1. חולים עם ממאירות סולידית עם איחוי גני מסוג NTRK, שמחלתם מתקדמת מקומית או גרורתית והם מיצו את אופציות הטיפול האפשריות למחלתם. 2. טיפול קו ראשון עבור חולים עם ממאירות סולידית עם איחוי גני מסוג NTRK במקרים האלה: א. Infantile fibrosarcoma; ב. Congenital mesoblastic nephroma, לא נתיחה או גרורתית; ג. Infant high grade glioma (HGG). ב. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת מעכבי NTRK. ג. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או באונקולוגיה ילדים. | 03/02/2022 | אונקולוגיה | ||
| א. התרופה תינתן לטיפול בילדים עם ממאירות סולידית עם איחוי גני מסוג NTRK, שמחלתם מתקדמת מקומית או גרורתית והם מיצו את אופציות הטיפול האפשריות למחלתם. ב. במהלך מחלתו יהיה החולה זכאי לתרופה אחת בלבד מתרופות המשתייכות למשפחת מעכבי NTRK. ג. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה או באונקולוגיה ילדים. | 01/03/2021 | אונקולוגיה | ||
| א. התרופה תינתן לטיפול בילדים עם ממאירות סולידית עם איחוי גני מסוג NTRK, שמחלתם מתקדמת מקומית או גרורתית והם מיצו את אופציות הטיפול האפשריות למחלתם. ב. מתן התרופה ייעשה לפי מרשם של מומחה באונקולוגיה ילדים. | 30/01/2020 | אונקולוגיה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
30/01/2020
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
