Quest for the right Drug
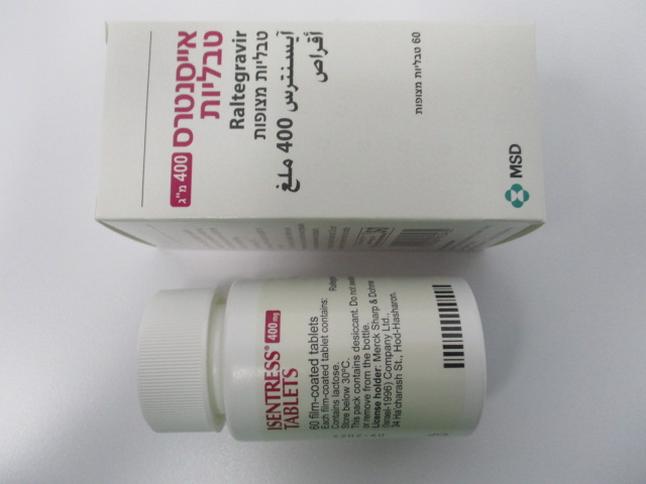
אייסנטרס 400 מ"ג טבליות ISENTRESS 400 MG TABLETS (RALTEGRAVIR AS POTASSIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: antivirals for systemic use, integrase inhibitors, ATC code: J05AJ01. Mechanism of action Raltegravir is an integrase strand transfer inhibitor active against the Human Immunodeficiency Virus (HIV-1). Raltegravir inhibits the catalytic activity of integrase, an HIV-encoded enzyme that is required for viral replication. Inhibition of integrase prevents the covalent insertion, or integration, of the HIV genome into the host cell genome. HIV genomes that fail to integrate cannot direct the production of new infectious viral particles, so inhibiting integration prevents propagation of the viral infection. Antiviral activity in vitro Raltegravir at concentrations of 31 ± 20 nM resulted in 95 % inhibition (IC95) of HIV-1 replication (relative to an untreated virus-infected culture) in human T-lymphoid cell cultures infected with the cell-line adapted HIV-1 variant H9IIIB. In addition, raltegravir inhibited viral replication in cultures of mitogen-activated human peripheral blood mononuclear cells infected with diverse, primary clinical isolates of HIV-1, including isolates from 5 non-B subtypes, and isolates resistant to reverse transcriptase inhibitors and protease inhibitors. In a single-cycle infection assay, raltegravir inhibited infection of 23 HIV isolates representing 5 non-B subtypes and 5 circulating recombinant forms with IC50 values ranging from 5 to 12 nM. Resistance Most viruses isolated from patients failing raltegravir had high-level raltegravir resistance resulting from the appearance of two or more mutations in integrase. Most had a signature mutation at amino acid 155 (N155 changed to H), amino acid 148 (Q148 changed to H, K, or R), or amino acid 143 (Y143 changed to H, C, or R), along with one or more additional integrase mutations (e.g., L74M, E92Q, T97A, E138A/K, G140A/S, V151I, G163R, S230R). The signature mutations decrease viral susceptibility to raltegravir and addition of other mutations results in a further decrease in raltegravir susceptibility. Factors that reduced the likelihood of developing resistance included lower baseline viral load and use of other active anti-retroviral agents. Mutations conferring resistance to raltegravir generally also confer resistance to the integrase strand transfer inhibitor elvitegravir. Mutations at amino acid 143 confer greater resistance to raltegravir than to elvitegravir, and the E92Q mutation confers greater resistance to elvitegravir than to raltegravir. Viruses harbouring a mutation at amino acid 148, along with one or more other raltegravir resistance mutations, may also have clinically significant resistance to dolutegravir. Clinical experience The evidence of efficacy of raltegravir was based on the analyses of 96-week data from two randomised, double-blind, placebo-controlled trials (BENCHMRK 1 and BENCHMRK 2, Protocols 018 and 019) in antiretroviral treatment-experienced HIV-1 infected adult patients and the analysis of 240-week data from randomised, double-blind, active-control trial (STARTMRK, Protocol 021) in antiretroviral treatment-naïve HIV-1 infected adult patients. Efficacy Treatment-experienced adult patients BENCHMRK 1 and BENCHMRK 2 (multi-centre, randomised, double-blind, placebo-controlled trials) evaluated the safety and anti-retroviral activity of raltegravir 400 mg twice daily vs. placebo in a combination with optimised background therapy (OBT), in HIV-infected patients, 16 years or older, with documented resistance to at least 1 drug in each of 3 classes (NRTIs, NNRTIs, PIs) of anti- retroviral therapies. Prior to randomisation, OBT were selected by the investigator based on the patient's prior treatment history, as well as baseline genotypic and phenotypic viral resistance testing. Patient demographics (gender, age and race) and baseline characteristics were comparable between the groups receiving raltegravir 400 mg twice daily and placebo. Patients had prior exposure to a median of 12 anti-retrovirals for a median of 10 years. A median of 4 ARTs was used in OBT. Results 48 week and 96 week analyses Durable outcomes (Week 48 and Week 96) for patients on the recommended dose raltegravir 400 mg twice daily from the pooled studies BENCHMRK 1 and BENCHMRK 2 are shown in Table 2. Table 2 Efficacy Outcome at Weeks 48 and 96 BENCHMRK 1 and 2 Pooled 48 Weeks 96 Weeks Raltegravir Placebo + OBT Raltegravir Placebo + Parameter 400 mg twice (N = 237) 400 mg twice OBT daily + OBT daily + OBT (N = 237) (N = 462) (N = 462) Percent HIV-RNA < 400 copies/mL (95 % CI) All patients† 72 (68, 76) 37 (31, 44) 62 (57, 66) 28 (23, 34) Baseline Characteristic‡ HIV-RNA > 100,000 copies/mL 62 (53, 69) 17 (9, 27) 53 (45, 61) 15 (8, 25) ≤ 100,000 copies/mL 82 (77, 86) 49 (41, 58) 74 (69, 79) 39 (31, 47) CD4-count ≤ 50 cells/mm3 61 (53, 69) 21 (13, 32) 51 (42, 60) 14 (7, 24) > 50 and ≤ 200 cells/mm3 80 (73, 85) 44 (33, 55) 70 (62, 77) 36 (25, 48) > 200 cells/mm3 83 (76, 89) 51 (39, 63) 78 (70, 85) 42 (30, 55) § Sensitivity score (GSS) 0 52 (42, 61) 8 (3, 17) 46 (36, 56) 5 (1, 13) 1 81 (75, 87) 40 (30, 51) 76 (69, 83) 31 (22, 42) 2 and above 84 (77, 89) 65 (52, 76) 71 (63, 78) 56 (43, 69) Percent HIV-RNA < 50 copies/ml (95 % CI) All patients† 62 (57, 67) 33 (27, 39) 57 (52, 62) 26 (21, 32) Baseline Characteristic‡ HIV-RNA > 100,000 copies/mL 48 (40, 56) 16 (8, 26) 47 (39, 55) 13 (7, 23) ≤ 100,000 copies/mL 73 (68, 78) 43 (35, 52) 70 (64, 75) 36 (28, 45) CD4-count ≤ 50 cells/mm3 50 (41, 58) 20 (12, 31) 50 (41, 58) 13 (6, 22) > 50 and ≤ 200 cells/mm3 67 (59, 74) 39 (28, 50) 65 (57, 72) 32 (22, 44) > 200 cells/mm3 76 (68, 83) 44 (32, 56) 71 (62, 78) 41 (29, 53) Sensitivity score (GSS) § 0 45 (35, 54) 3 (0, 11) 41 (32, 51) 5 (1, 13) 1 67 (59, 74) 37 (27, 48) 72 (64, 79) 28 (19, 39) 2 and above 75 (68, 82) 59 (46, 71) 65 (56, 72) 53 (40, 66) Mean CD4 Cell Change (95 % CI), cells/mm3 All patients‡ 109 (98, 121) 45 (32, 57) 123 (110, 137) 49 (35, 63) Baseline Characteristic‡ HIV-RNA > 100,000 copies/mL 126 (107, 144) 36 (17, 55) 140 (115, 165) 40 (16, 65) ≤ 100,000 copies/mL 100 (86, 115) 49 (33, 65) 114 (98, 131) 53 (36, 70) CD4-count ≤ 50 cells/mm3 121 (100, 142) 33 (18, 48) 130 (104, 156) 42 (17, 67) > 50 and ≤ 200 cells/mm3 104 (88, 119) 47 (28, 66) 123 (103, 144) 56 (34, 79) 3 > 200 cells/mm 104 (80, 129) 54 (24, 84) 117 (90, 143) 48 (23, 73) § Sensitivity score (GSS) 0 81 (55, 106) 11 (4, 26) 97 (70, 124) 15 (-0, 31) 1 113 (96, 130) 44 (24, 63) 132 (111, 154) 45 (24, 66) 2 and above 125 (105, 144) 76 (48, 103) 134 (108, 159) 90 (57, 123) † Non-completer is failure imputation: patients who discontinued prematurely are imputed as failure thereafter. Percent of patients with response and associated 95 % confidence interval (CI) are reported. ‡ For analysis by prognostic factors, virologic failures were carried forward for percent < 400 and 50 copies/mL. For mean CD4 changes, baseline- carry-forward was used for virologic failures. § The Genotypic Sensitivity Score (GSS) was defined as the total oral ARTs in the optimised background therapy (OBT) to which a patient's viral isolate showed genotypic sensitivity based upon genotypic resistance test. Enfuvirtide use in OBT in enfuvirtide-naïve patients was counted as one active drug in OBT. Similarly, darunavir use in OBT in darunavir-naïve patients was counted as one active drug in OBT. Raltegravir achieved virologic responses (using Not Completer=Failure approach) of HIV RNA < 50 copies/mL in 61.7 % of patients at Week 16, in 62.1 % at Week 48 and in 57.0% at Week 96. Some patients experienced viral rebound between Week 16 and Week 96. Factors associated with failure include high baseline viral load and OBT that did not include at least one potent active agent. Switch to raltegravir The SWITCHMRK 1 & 2 (Protocols 032 & 033) studies evaluated HIV-infected patients receiving suppressive (screening HIV RNA < 50 copies/mL; stable regimen > 3 months) therapy with lopinavir 200 mg (+) ritonavir 50 mg 2 tablets twice daily plus at least 2 nucleoside reverse transcriptase inhibitors and randomised them 1:1 to continue lopinavir (+) ritonavir 2 tablets twice daily (n=174 and n=178, respectively) or replace lopinavir (+) ritonavir with raltegravir 400 mg twice daily (n=174 and n=176, respectively). Patients with a prior history of virological failure were not excluded and the number of previous antiretroviral therapies was not limited. These studies were terminated after the primary efficacy analysis at Week 24 because they failed to demonstrate non-inferiority of raltegravir versus lopinavir (+) ritonavir. In both studies at Week 24, suppression of HIV RNA to less than 50 copies/mL was maintained in 84.4 % of the raltegravir group versus 90.6 % of the lopinavir (+) ritonavir group, (Non-completers = Failure). See section 4.4 regarding the need to administer raltegravir with two other active agents. Treatment-naïve adult patients STARTMRK (multi-centre, randomised, double-blind, active-control trial) evaluated the safety and anti-retroviral activity of raltegravir 400 mg twice daily vs. efavirenz 600 mg at bedtime, in a combination with emtricitabine (+) tenofovir disoproxil fumarate, in treatment-naïve HIV-infected patients with HIV RNA > 5,000 copies/mL. Randomisation was stratified by screening HIV RNA level (≤ 50,000 copies/mL; and > 50,000 copies/mL) and by hepatitis B or C status (positive or negative). Patient demographics (gender, age and race) and baseline characteristics were comparable between the group receiving raltegravir 400 mg twice daily and the group receiving efavirenz 600 mg at bedtime. Results 48-week and 240-week analyses With respect to the primary efficacy endpoint, the proportion of patients achieving HIV RNA < 50 copies/mL at Week 48 was 241/280 (86.1 %) in the group receiving raltegravir and 230/281 (81.9 %) in the group receiving efavirenz. The treatment difference (raltegravir – efavirenz) was 4.2 % with an associated 95 % CI of (-1.9, 10.3) establishing that raltegravir is non-inferior to efavirenz (p-value for non-inferiority < 0.001). At Week 240, the treatment difference (raltegravir – efavirenz) was 9.5 % with an associated 95 % CI of (1.7, 17.3). Week 48 and Week 240 outcomes for patients on the recommended dose of raltegravir 400 mg twice daily from STARTMRK are shown in Table 3. Table 3 Efficacy Outcome at Weeks 48 and 240 STARTMRK Study 48 Weeks 240 Weeks Raltegravir Efavirenz Raltegravir Efavirenz Parameter 400 mg twice 600 mg 400 mg twice 600 mg daily at bedtime daily at bedtime (N = 281) (N = 282) (N = 281) (N = 282) Percent HIV-RNA < 50 copies/mL (95 % CI) All patients† 86 (81, 90) 82 (77, 86) 71 (65, 76) 61 (55, 67) Baseline Characteristic‡ HIV-RNA > 100,000 copies/mL 91 (85, 95) 89 (83, 94) 70 (62, 77) 65 (56, 72) ≤ 100,000 copies/mL 93 (86, 97) 89 (82, 94) 72 (64, 80) 58 (49, 66) CD4-count ≤ 50 cells/mm3 84 (64, 95) 86 (67, 96) 58 (37, 77) 77 (58, 90) > 50 and ≤ 200 cells/mm3 89 (81, 95) 86 (77, 92) 67 (57, 76) 60 (50, 69) > 200 cells/mm3 94 (89, 98) 92 (87, 96) 76 (68, 82) 60 (51, 68) Viral Subtype Clade B 90 (85, 94) 89 (83, 93) 71 (65, 77) 59 (52, 65) Non-Clade B 96 (87, 100) 91 (78, 97) 68 (54, 79) 70 (54, 82) Mean CD4 Cell Change (95 % CI), cells/mm3 All patients‡ 189 (174, 204) 163 (148, 178) 374 (345, 403) 312 (284, 339) Baseline Characteristic‡ HIV-RNA > 100,000 copies/mL 196 (174, 219) 192 (169, 214) 392 (350, 435) 329 (293, 364) ≤ 100,000 copies/mL 180 (160, 200) 134 (115, 153) 350 (312, 388) 294 (251, 337) CD4-count ≤ 50 cells/mm3 170 (122, 218) 152 (123, 180) 304 (209, 399) 314 (242, 386) > 50 and ≤ 200 cells/mm3 193 (169, 217) 175 (151, 198) 413 (360, 465) 306 (264, 348) > 200 cells/mm3 190 (168, 212) 157 (134, 181) 358 (321, 395) 316 (272, 359) Viral Subtype Clade B 187 (170, 204) 164 (147, 181) 380 (346, 414) 303 (272, 333) Non-Clade B 189 (153, 225) 156 (121, 190) 332 (275, 388) 329 (260, 398) STARTMRK Study 48 Weeks 240 Weeks Raltegravir Efavirenz Raltegravir Efavirenz Parameter 400 mg twice 600 mg 400 mg twice 600 mg daily at bedtime daily at bedtime (N = 281) (N = 282) (N = 281) (N = 282) † Non-completer is failure imputation: patients who discontinued prematurely are imputed as failure thereafter. Percent of patients with response and associated 95 % confidence interval (CI) are reported. ‡ For analysis by prognostic factors, virologic failures were carried forward for percent < 50 and 400 copies/mL. For mean CD4 changes, baseline- carry-forward was used for virologic failures. Notes: The analysis is based on all available data. Raltegravir and efavirenz were administered with emtricitabine (+) tenofovir disoproxil fumarate.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption As demonstrated in healthy volunteers administered single oral doses of raltegravir in the fasted state, raltegravir is rapidly absorbed with a tmax of approximately 3 hours postdose. Raltegravir AUC and Cmax increase dose proportionally over the dose range 100 mg to 1,600 mg. Raltegravir C12 hr increases dose proportionally over the dose range of 100 to 800 mg and increases slightly less than dose proportionally over the dose range 100 mg to 1,600 mg. Dose proportionality has not been established in patients. With twice-daily dosing, pharmacokinetic steady state is achieved rapidly, within approximately the first 2 days of dosing. There is little to no accumulation in AUC and Cmax and evidence of slight accumulation in C12 hr. The absolute bioavailability of raltegravir has not been established. Raltegravir may be administered with or without food. Raltegravir was administered without regard to food in the pivotal safety and efficacy studies in HIV-infected patients. Administration of multiple doses of raltegravir following a moderate-fat meal did not affect raltegravir AUC to a clinically meaningful degree with an increase of 13 % relative to fasting. Raltegravir C12 hr was 66 % higher and Cmax was 5 % higher following a moderate-fat meal compared to fasting. Administration of raltegravir following a high-fat meal increased AUC and C max by approximately 2-fold and increased C 12 hr by 4.1-fold. Administration of raltegravir following a low-fat meal decreased AUC and Cmax by 46 % and 52 %, respectively; C12 hr was essentially unchanged. Food appears to increase pharmacokinetic variability relative to fasting. Overall, considerable variability was observed in the pharmacokinetics of raltegravir. For observed C12 hr in BENCHMRK 1 and 2 the coefficient of variation (CV) for inter-subject variability = 212 % and the CV for intra-subject variability = 122 %. Sources of variability may include differences in co-administration with food and concomitant medicines. Distribution Raltegravir is approximately 83 % bound to human plasma protein over the concentration range of 2 to 10 µM. Raltegravir readily crossed the placenta in rats, but did not penetrate the brain to any appreciable extent. In two studies of HIV-1 infected patients who received raltegravir 400 mg twice daily, raltegravir was readily detected in the cerebrospinal fluid. In the first study (n=18), the median cerebrospinal fluid concentration was 5.8 % (range 1 to 53.5 %) of the corresponding plasma concentration. In the second study (n=16), the median cerebrospinal fluid concentration was 3 % (range 1 to 61 %) of the corresponding plasma concentration. These median proportions are approximately 3- to 6-fold lower than the free fraction of raltegravir in plasma. Biotransformation and excretion The apparent terminal half-life of raltegravir is approximately 9 hours, with a shorter α-phase half-life (~1 hour) accounting for much of the AUC. Following administration of an oral dose of radiolabeled raltegravir, approximately 51 and 32 % of the dose was excreted in faeces and urine, respectively. In faeces, only raltegravir was present, most of which is likely to be derived from hydrolysis of raltegravir-glucuronide secreted in bile as observed in preclinical species. Two components, namely raltegravir and raltegravir-glucuronide, were detected in urine and accounted for approximately 9 and 23 % of the dose, respectively. The major circulating entity was raltegravir and represented approximately 70 % of the total radioactivity; the remaining radioactivity in plasma was accounted for by raltegravir-glucuronide. Studies using isoform-selective chemical inhibitors and cDNA-expressed UDP-glucuronosyltransferases (UGT) show that UGT1A1 is the main enzyme responsible for the formation of raltegravir-glucuronide. Thus, the data indicate that the major mechanism of clearance of raltegravir in humans is UGT1A1-mediated glucuronidation. UGT1A1 Polymorphism In a comparison of 30 subjects with *28/*28 genotype to 27 subjects with wild-type genotype, the geometric mean ratio (90 % CI) of AUC was 1.41 (0.96, 2.09) and the geometric mean ratio of C 12 hr was 1.91 (1.43, 2.55). Dose adjustment is not considered necessary in subjects with reduced UGT1A1 activity due to genetic polymorphism. Special populations Elderly There was no clinically meaningful effect of age on raltegravir pharmacokinetics in healthy subjects and patients with HIV-1 infection over the age range studied (19 to 84 years, with few individuals over the age of 65). Gender, race and BMI There were no clinically important pharmacokinetic differences due to gender, race or body mass index (BMI) in adults. Renal impairment Renal clearance of unchanged medicinal product is a minor pathway of elimination. In adults, there were no clinically important pharmacokinetic differences between patients with severe renal insufficiency and healthy subjects (see section 4.2). Because the extent to which raltegravir may be dialysable is unknown, dosing before a dialysis session should be avoided. Hepatic impairment Raltegravir is eliminated primarily by glucuronidation in the liver. In adults, there were no clinically important pharmacokinetic differences between patients with moderate hepatic insufficiency and healthy subjects. The effect of severe hepatic insufficiency on the pharmacokinetics of raltegravir has not been studied (see sections 4.2 and 4.4).

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בנשאי HIV. ב. מתן התרופה ייעשה לפי מרשם של מנהל מרפאה לטיפול באיידס במוסד רפואי שהמנהל הכיר בו כמרכז AIDS;ג. משטר הטיפול בתרופה יהיה כפוף להנחיות המנהל כפי שיעודכנו מזמן לזמן על פי המידע העדכני בתחום הטיפול במחלה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בנשא HIV |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
140 33 31793 02
מחיר
0 ₪
מידע נוסף
