Quest for the right Drug
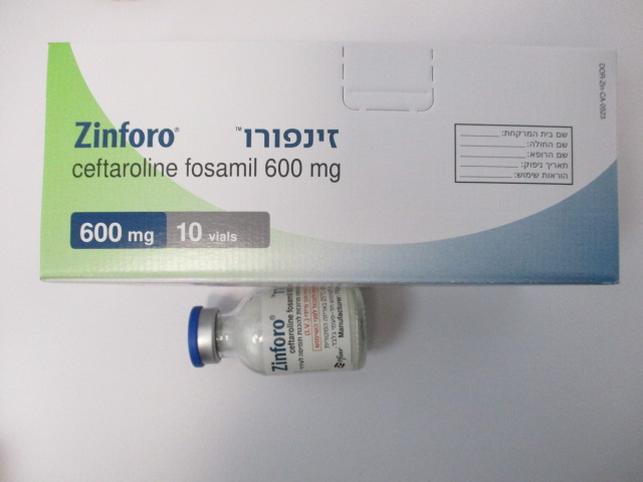
זינפורו ZINFORO (CEFTAROLINE FOSAMIL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antibacterials for systemic use, other cephalosporins and penems, ATC code: J01DI02 The active moiety after Zinforo administration is ceftaroline. Mechanism of action Ceftaroline is a cephalosporin antibacterial with in vitro activity against Gram-positive and -negative bacteria. The bactericidal action of ceftaroline is mediated through binding to essential penicillin- binding proteins (PBPs). Biochemical studies have shown that ceftaroline has high affinity for PBP2a of methicillin-resistant Staphylococcus aureus (MRSA) and PBP2x of penicillin non-susceptible Streptococcus pneumoniae (PNSP). As a result, minimum inhibitory concentrations (MICs) of ceftaroline against a proportion of these organisms tested fall into the susceptible range (see Resistance section below). Resistance Ceftaroline is not active against strains of Enterobacterales producing extended-spectrum beta- lactamases (ESBLs) from the TEM, SHV or CTX-M families, serine carbapenemases (such as KPC), class B metallo-beta-lactamases or class C (AmpC) cephalosporinases. Organisms that express these enzymes and which are therefore resistant to ceftaroline occur at very variable rates between countries and between healthcare facilities within countries. If ceftaroline is commenced before susceptibility test results are available then local information on the risk of encountering organisms that express these enzymes should be taken into consideration. Resistance may also be mediated by bacterial impermeability or drug efflux pump mechanisms. One or more of these mechanisms may co-exist in a single bacterial isolate. Interaction with other antibacterial agents In vitro studies have not demonstrated any antagonism between ceftaroline in combination with other commonly used antibacterial agents (e.g. amikacin, azithromycin, aztreonam, daptomycin, levofloxacin, linezolid, meropenem, tigecycline, and vancomycin). Susceptibility testing breakpoints MIC (minimum inhibitory concentration) interpretive criteria for susceptibility testing have been established by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) breakpoints for ceftaroline fosamil and are listed here: https://www.ema.europa.eu/documents/other/minimum-inhibitory-concentration-mic- breakpoints_en.xlsx Pharmacokinetic/pharmacodynamic relationship As with other beta-lactam antimicrobial agents, the percent time above the minimum inhibitory concentration (MIC) of the infecting organism over the dosing interval (%T > MIC) has been shown to be the parameter that best correlates with the efficacy of ceftaroline. Clinical efficacy against specific pathogens Efficacy has been demonstrated in clinical studies against the pathogens listed under each indication that were susceptible to ceftaroline in vitro. Complicated skin and soft tissue infections Gram-positive micro-organisms • Staphylococcus aureus (including methicillin-resistant strains) • Streptococcus pyogenes • Streptococcus agalactiae • Streptococcus anginosus group (includes S. anginosus, S. intermedius, and S. constellatus) • Streptococcus dysgalactiae Gram-negative micro-organisms • Escherichia coli • Klebsiella pneumoniae • Klebsiella oxytoca • Morganella morganii Community-acquired pneumonia No cases of CAP due to MRSA were enrolled into the studies. The available clinical data cannot substantiate efficacy against penicillin non-susceptible strains of S. pneumoniae. Gram-positive micro-organisms • Streptococcus pneumoniae • Staphylococcus aureus (methicillin-susceptible strains only) Gram-negative micro-organisms • Escherichia coli • Haemophilus influenzae • Haemophilus parainfluenzae • Klebsiella pneumoniae Antibacterial activity against other relevant pathogens Clinical efficacy has not been established against the following pathogens although in vitro studies suggest that they would be susceptible to ceftaroline in the absence of acquired mechanisms of resistance: Anaerobic micro-organisms Gram-positive micro-organisms • Peptostreptococcus spp. Gram-negative micro-organisms • Fusobacterium spp. In vitro data indicate that the following species are not susceptible to ceftaroline: • Chlamydophila spp. • Legionella spp. • Mycoplasma spp. • Proteus spp. • Pseudomonas aeruginosa
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The Cmax and AUC of ceftaroline increase approximately in proportion to dose within the single dose range of 50 to 1000 mg. No appreciable accumulation of ceftaroline is observed following multiple intravenous infusions of 600 mg administered over 60 minutes every 8 or 12 hours for up to 14 days in healthy adults with CrCL > 50 mL/min. Distribution The plasma protein binding of ceftaroline is low (approximately 20%) and ceftaroline is not distributed into erythrocytes. The median steady-state volume of distribution of ceftaroline in healthy adult males following a single 600 mg intravenous dose of radiolabelled ceftaroline fosamil was 20.3 l, similar to the volume of extracellular fluid. Biotransformation Ceftaroline fosamil (prodrug) is converted into the active ceftaroline in plasma by phosphatase enzymes and concentrations of the prodrug are measurable in plasma primarily during intravenous infusion. Hydrolysis of the beta-lactam ring of ceftaroline occurs to form the microbiologically inactive, open-ring metabolite, ceftaroline M-1. The mean plasma ceftaroline M-1 to ceftaroline AUC ratio following a single 600 mg intravenous infusion of ceftaroline fosamil in healthy subjects is approximately 20-30%. In pooled human liver microsomes, metabolic turnover was low for ceftaroline, indicating that ceftaroline is not metabolised by hepatic CYP450 enzymes. Elimination Ceftaroline is primarily eliminated by the kidneys. Renal clearance of ceftaroline is approximately equal, or slightly lower than the glomerular filtration rate in the kidney, and in vitro transporter studies indicate that active secretion does not contribute to the renal elimination of ceftaroline. The mean terminal elimination half-life of ceftaroline in healthy adults is approximately 2.5 hours. Following the administration of a single 600 mg intravenous dose of radiolabelled ceftaroline fosamil to healthy male adults, approximately 88% of radioactivity was recovered in urine and 6% in faeces. Special populations Renal impairment Dosage adjustments are required in adults, adolescents and children with CrCL ≤ 50 mL/min (see section 4.2). There is insufficient information to recommend dosage adjustments in adolescents with ESRD aged from 12 to < 18 years and with bodyweight < 33 kg and in children with ESRD aged from 2 to < 12 years. There is insufficient information to recommend dosage adjustments in paediatric patients aged < 2 years with moderate or severe renal impairment or ESRD. Hepatic impairment The pharmacokinetics of ceftaroline in patients with hepatic impairment has not been established. As ceftaroline does not appear to undergo significant hepatic metabolism, the systemic clearance of ceftaroline is not expected to be significantly affected by hepatic impairment. Therefore, no dosage adjustment is recommended for patients with hepatic impairment. Elderly Following administration of a single 600 mg intravenous dose of ceftaroline fosamil, the pharmacokinetics of ceftaroline were similar between healthy elderly subjects (≥ 65 years of age), and healthy young adult subjects (18-45 years of age). There was a 33% increase in AUC0-∞ in the elderly that was mainly attributable to age-related changes in renal function. Zinforo dose adjustment is not required in elderly patients with creatinine clearance above 50 mL/min. Paediatric population Dose adjustments are required for children aged from 2 months to < 12 years and for adolescents aged 12 to < 18 years with bodyweight < 33 kg (see section 4.2). The safety and efficacy of Zinforo in children aged birth to < 2 months have not been established. Patients with cystic fibrosis Cystic fibrosis patients were excluded from CAP clinical trials. Some case reports and published studies suggest the need for a higher dose of ceftaroline fosamil in cystic fibrosis patients due to possibility of altered ceftaroline pharmacokinetics leading to sub-therapeutic levels. Results from a population pharmacokinetic study, based on data pooled from various studies, overall showed no significant, clinically relevant differences in ceftaroline pharmacokinetic parameters in cystic fibrosis patients (age 6 years and above). Ceftaroline clearance was similar between cystic fibrosis patients and patients with CAP or cSSTI while ceftaroline central volume was similar to healthy subjects.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
