Quest for the right Drug
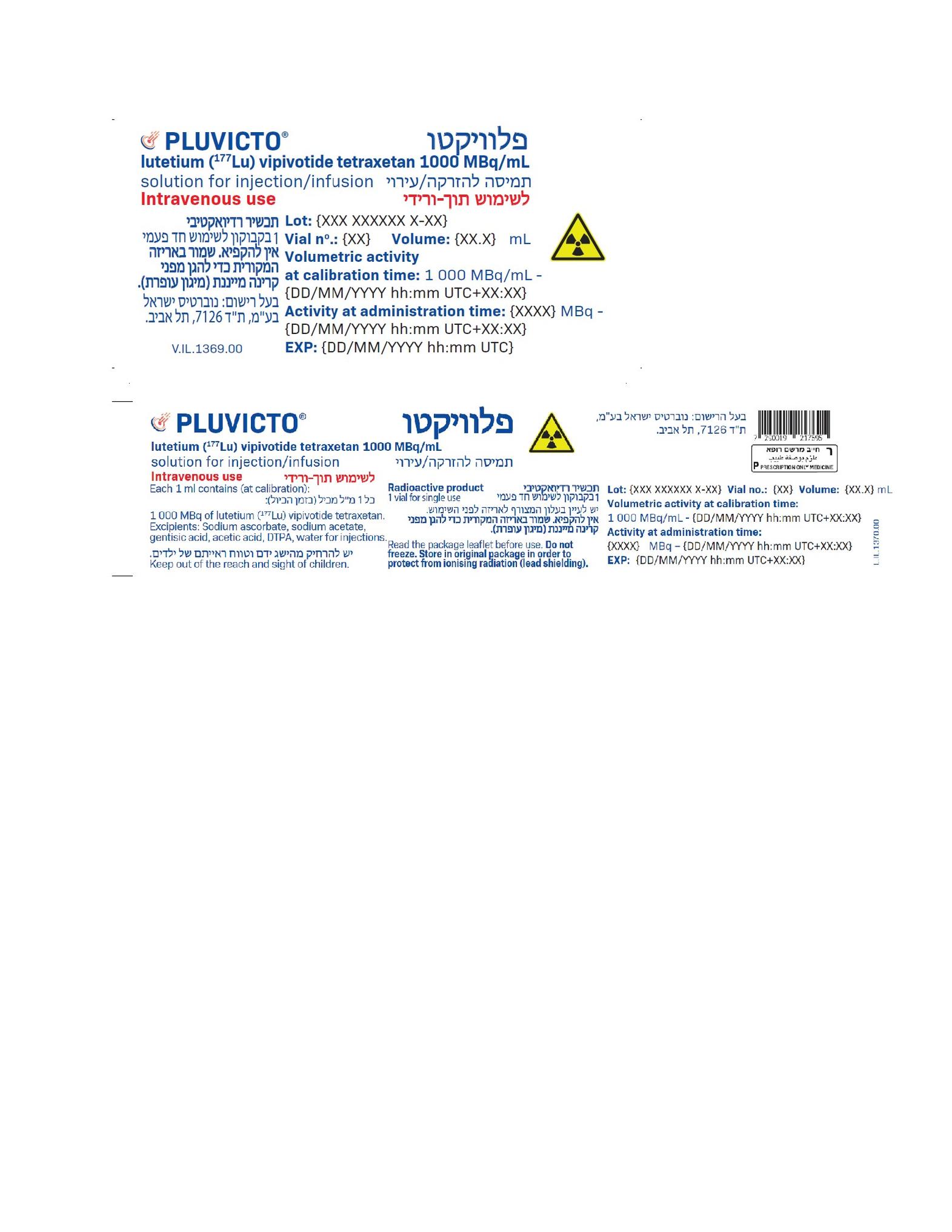
פלוויקטו PLUVICTO (LUTETIUM (177LU) VIPIVOTIDE TETRAXETAN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה להזרקהאינפוזיה : SOLUTION FOR INJECTION / INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
8 ADVERSE REACTIONS The following clinically significant adverse reactions are described elsewhere in the labeling: • Myelosuppression [see Warnings and Precautions (7.2)] • Renal Toxicity [see Warnings and Precautions (7.3)] 8.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The safety of PLUVICTO was evaluated in the VISION study in patients with progressive, PSMA-positive mCRPC [see Clinical Studies (14)]. Of the 831 patients randomized, 734 patients received at least one dose of randomized treatment. Patients received at least one dose of either PLUVICTO 7.4 GBq (200 mCi) administered every 6 to 10 weeks plus BSoC (N = 529) or BSoC alone (N = 205). The median duration of exposure to randomized treatment was 7.8 months (range, 0.3 to 24.9) for patients who received PLUVICTO plus BSoC. Among patients who received PLUVICTO plus BSoC, the PLU API APR23 V1.0 USPI October 2022 median number of doses of PLUVICTO received was 5 (range, 1 to 6). The median cumulative dose of PLUVICTO was 37.5 GBq (range, 7.0 to 48.3). The median duration of follow-up was 14.8 months for patients receiving PLUVICTO plus BSoC. Serious adverse reactions occurred in 36% of patients who received PLUVICTO plus BSoC. Serious adverse reactions in > 1% of patients who received PLUVICTO plus BSoC included hemorrhage (4%), musculoskeletal pain (3.8%), sepsis (3.2%), anemia (2.8%), urinary tract infection (2.6%), acute kidney injury (1.7%), pneumonia (1.7%), pancytopenia (1.3%), pyrexia (1.3%), spinal cord compression (1.1%), and pulmonary embolism (1.1%). Fatal adverse reactions occurred in 2.8% of patients who received PLUVICTO plus BSoC, including sepsis (0.9%), pancytopenia (0.6%), hepatic failure (0.4%), intracranial hemorrhage (0.2%), subdural hematoma (0.2%), ischemic stroke (0.2%), COVID-19 (0.2%), and aspiration pneumonia (0.2%). PLUVICTO was permanently discontinued due to adverse reactions in 12% of patients. Adverse reactions leading to permanent discontinuation of PLUVICTO in ≥ 1% of patients who received PLUVICTO plus BSoC were anemia (2.8%), thrombocytopenia (2.8%), and leukopenia (including neutropenia) (1.7%). Adverse reactions leading to a dose interruption of PLUVICTO occurred in 16% of patients. The most frequent (≥ 3%) adverse reactions leading to a dose interruption of PLUVICTO in patients who received PLUVICTO plus BSoC were anemia (5%) and thrombocytopenia (3.6%). Adverse reactions leading to a dose reduction of PLUVICTO occurred in 6% of patients. The most frequent (≥ 1%) adverse reactions leading to a dose reduction of PLUVICTO in patients who received PLUVICTO plus BSoC were thrombocytopenia (1.9%) and anemia (1.3%). The most common adverse reactions (≥ 20%) occurring at a higher incidence in patients who received PLUVICTO plus BSoC were fatigue, dry mouth, nausea, anemia, decreased appetite, and constipation. The most common laboratory abnormalities that worsened from baseline in ≥ 30% of patients who received PLUVICTO plus BSoC were decreased lymphocytes, decreased hemoglobin, decreased leukocytes, decreased platelets, decreased calcium, and decreased sodium. Table 3 and Table 4 summarize the incidence of adverse reactions and laboratory abnormalities, respectively. Table 3: Adverse Reactions (≥ 5%) in Patients With PSMA-positive mCRPC Who Received PLUVICTO Plus BSoC in VISION Adverse reactions PLUVICTO plus BSoC BSoC (N = 529) (N = 205) All Grades Grades 3 to 4 All Grades Grades 3 to 4 (%) (%) (%) (%) General disorders Fatigue 43 6 23 1.5 Decreased appetite 21 1.9 15 0.5 Weight decreased 11 0.4 9 0 Peripheral edemaa 10 0.4 7 0.5 Pyrexia 7 0.4 3.4 0 Gastrointestinal disorders Dry mouthb 39 0 0.5 0 Nausea 35 1.3 17 0.5 Constipation 20 1.1 11 0.5 Vomitingc 19 0.9 6 0.5 Diarrhea 19 0.8 2.9 0.5 Abdominal paind 11 1.1 6 0.5 Blood and lymphatic system disorders PLU API APR23 V1.0 USPI October 2022 Adverse reactions PLUVICTO plus BSoC BSoC (N = 529) (N = 205) All Grades Grades 3 to 4 All Grades Grades 3 to 4 (%) (%) (%) (%) Anemia 32 13 13 4.9 Thrombocytopenia 17 8 4.4 1 Renal and urinary disorders Urinary tract infectione 12 3.8 1 0.5 Acute kidney injuryf 9 3.2 6 2.9 Nervous system disorders Dizziness 8 0.9 4.4 0 Headache 7 0.8 2 0 Dysgeusiag 7 0 1.5 0 Abbreviation: BSoC, best standard of care. a Peripheral edema includes peripheral edema, fluid retention, and fluid overload. b Dry mouth includes dry mouth, aptyalism, and dry throat. cVomiting includes vomiting and retching. dAbdominal pain includes abdominal pain, abdominal pain upper, abdominal discomfort, abdominal pain lower, abdominal tenderness, and gastrointestinal pain. e Urinary tract infection includes urinary tract infection, cystitis, and cystitis bacterial. fAcute kidney injury includes blood creatinine increased, acute kidney injury, renal failure, and blood urea increased. gDysgeusia includes dysgeusia and taste disorder. Clinically relevant adverse reactions in < 5% of patients who received PLUVICTO plus BSoC included dry eye, vertigo, and pancytopenia (including bicytopenia). Table 4: Select Laboratory Abnormalities (≥ 10%) That Worsened from Baseline in Patients With PSMA-positive mCRPC Who Received PLUVICTO Plus BSoC (Between Arm Difference of ≥ 5% All Grades) in VISION Laboratory abnormalities PLUVICTO plus BSoCa BSoCb All Grades Grades 3 to 4 All Grades Grades 3 to 4 (%) (%) (%) (%) Chemistry Decreased calcium 39 2.5 28 3 c Decreased sodium 33 0.6 23 1 Increased aspartate aminotransferase 28 1.1 18 1c Increased creatinine 24 0.9c 14 0.5c Increased potassium 24 0.6 18 0.5c Increased sodium 11 0c 5 0c Hematology Decreased lymphocytes 85 47 51 18 c Decreased hemoglobin 63 15 34 7c Decreased leukocytes 56 7 22 2 Decreased platelets 45 9 20 2.5 Decreased neutrophils 28 4.5 9 0.5 Abbreviation: BSoC, best standard of care. a The denominator used to calculate the rate for each laboratory parameter varied from 506 to 529 based on the number of patients with a baseline value and at least one post-treatment value. PLU API APR23 V1.0 USPI October 2022 b The denominator used to calculate the rate for each laboratory parameter varied from 194 to 198 based on the number of patients with a baseline value and at least one post-treatment value. cNo Grade 4 laboratory abnormalities worsening from baseline were reported. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/ 9 USE IN SPECIFIC POPULATIONS 9.1 Pregnancy Risk Summary The safety and efficacy of PLUVICTO have not been established in females. Based on its mechanism of action, PLUVICTO can cause fetal harm [see Clinical Pharmacology (12.1)]. There are no available data on PLUVICTO use in pregnant females. No animal studies using lutetium Lu 177 vipivotide tetraxetan have been conducted to evaluate its effect on female reproduction and embryo-fetal development; however, all radiopharmaceuticals, including PLUVICTO, have the potential to cause fetal harm. 9.2 Lactation Risk Summary The safety and efficacy of PLUVICTO have not been established in females. There are no data on the presence of lutetium Lu 177 vipivotide tetraxetan in human milk or its effects on the breastfed child or on milk production. 9.3 Females and Males of Reproductive Potential Contraception Males Based on its mechanism of action, advise male patients with female partners of reproductive potential to use effective contraception during treatment with PLUVICTO and for 14 weeks after the last dose [see Clinical Pharmacology (12.1), Nonclinical Toxicology (13.1)]. Infertility The recommended cumulative dose of 44.4 GBq of PLUVICTO results in a radiation absorbed dose to the testes within the range where PLUVICTO may cause temporary or permanent infertility. 9.4 Children and adolescents The safety and effectiveness of PLUVICTO in children and adolescents under the age of 18 years have not been established. 9.5 Geriatric Use Of the 529 patients who received at least one dose of PLUVICTO plus BSoC in the VISION study, 387 patients (73%) were 65 years or older and 143 patients (27%) were 75 years or older. No overall differences in effectiveness were observed between patients ≥ 75 years of age and younger patients. Serious adverse reactions occurred in 11% of patients ≥ 75 years of age and in 11% of younger patients. Grade ≥ 3 adverse reactions occurred in 40% of patients ≥ 75 years of age and in 31% of younger patients. 9.6 Renal Impairment Exposure of lutetium Lu 177 vipivotide tetraxetan is expected to increase with the degree of renal impairment [see Clinical Pharmacology (12.3)]. No dose adjustment is recommended for patients with mild (baseline CLcr 60 to 89 mL/min by Cockcroft-Gault) to moderate (CLcr 30 to 59 mL/min) renal impairment; however, patients with mild or PLU API APR23 V1.0 USPI October 2022 moderate renal impairment may be at greater risk of toxicity. Frequently monitor renal function and adverse reactions in patients with mild to moderate renal impairment [see Dosage and Administration (4.4)]. The pharmacokinetics and safety of PLUVICTO have not been studied in patients with severe (CLcr 15 to 29 mL/min) renal impairment or end-stage renal disease.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
