Quest for the right Drug
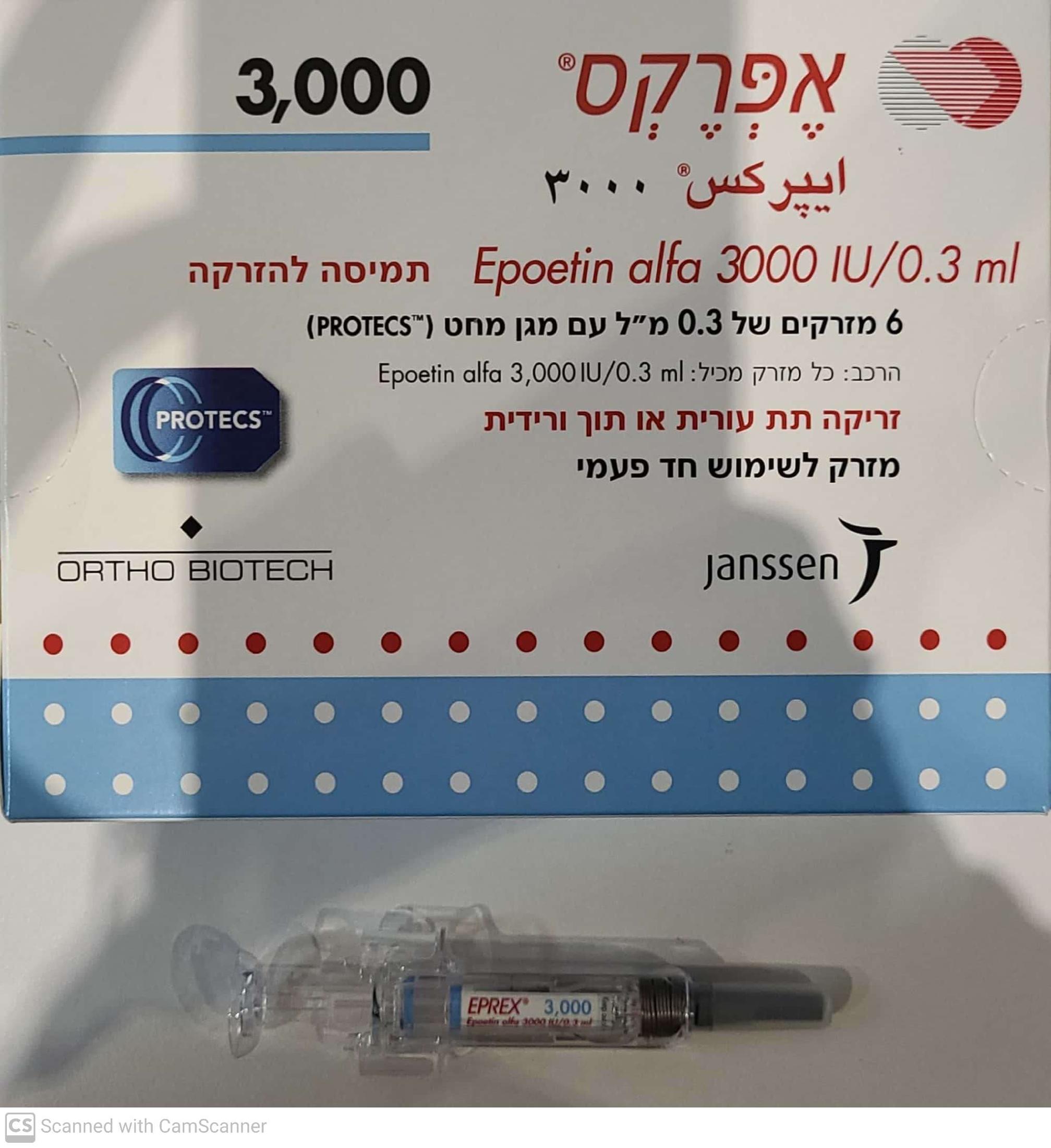
אפרקס מזרקים 3000 EPREX 3000 (RECOMBINANT HUMAN ERYTHROPOIETIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי, תת-עורי : I.V, S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Method of administration As with any other injectable product, check that there are no particles in the solution or change in colour. Before use, leave the EPREX syringe to stand until it reaches room temperature. This usually takes between 15 and 30 minutes. a) Intravenous injection: Administer over at least one to five minutes, depending on the total dose. In haemodialysed patients, a bolus injection may be given during the dialysis session through a suitable venous port in the dialysis line. Alternatively, the injection can be given at the end of the dialysis session via the fistula needle tubing, followed by 10 ml of isotonic saline to rinse the tubing and ensure satisfactory injection of the product into the circulation. A slower injection is preferable in patients who react to the treatment with “flu-like” symptoms (see section 4.8). Do not administer EPREX by intravenous infusion or in conjunction with other drug solutions. subcutaneous injection: A maximum volume of 1 ml at one injection site should generally not be exceeded. In case of larger volumes, more than one site should be chosen for the injection. The injections are given in the limbs or the anterior abdominal wall. In those situations, in which the physician determines that a patient or caregiver can safely and effectively administer EPREX, subcutaneously, instruction as to the proper dosage and administration should be provided. Eprex_Solution for injection_Sep2021_Ref EU SmPC Jun2021 Page 3 of 25 Refer to section 3, How should the medicine be used? (instructions on how to inject EPREX) of the package leaflet. Posology All other causes of anaemia (iron, folate or Vitamin B12 deficiency, aluminium intoxication, infection or inflammation, blood loss, haemolysis and bone marrow fibrosis of any origin) should be evaluated and treated prior to initiating therapy with epoetin alfa, and when deciding to increase the dose. In order to ensure optimum response to epoetin alfa, adequate iron stores should be assured and iron supplementation should be administered if necessary (see section 4.4). Treatment of symptomatic anaemia in adult and paediatric chronic renal failure patients: In patients with chronic renal failure where intravenous access is routinely available (haemodialysis patients) administration by the intravenous route is preferable. Where intravenous access is not readily available (patients not yet undergoing dialysis and peritoneal dialysis patients), EPREX may be administered subcutaneously. Treatment of symptomatic anaemia in adult chronic renal failure patients Anaemia symptoms and sequelae may vary with age, gender, and co-morbid medical conditions; a physician’s evaluation of the individual patient’s clinical course and condition is necessary. The recommended desired haemoglobin concentration range is between 10 g/dL to 12 g/dL (6.2 to 7.5 mmol/L). EPREX should be administered in order to increase haemoglobin to not greater than 12 g/dL (7.5 mmol/L). A rise in haemoglobin of greater than 2 g/dL (1.25 mmol/L) over a four week period should be avoided. If it occurs, appropriate dose adjustment should be made as provided. Due to intra-patient variability, occasional individual haemoglobin values for a patient above and below the desired haemoglobin level may be observed. Haemoglobin variability should be addressed through dose management, with consideration for the haemoglobin target range of 10 g/dL (6.2 mmol/L) to 12 g/dL (7.5 mmol/L). A sustained haemoglobin level of greater than 12 g/dL (7.5 mmol/L) should be avoided. If the haemoglobin is rising by more than 2 g/dL (1.25 mmol/L) per month, or if the sustained haemoglobin exceeds 12 g/dL (7.5 mmol/L) reduce the EPREX dose by 25%. If the haemoglobin exceeds 13 g/dL (8.1 mmol/L), discontinue therapy until it falls below 12 g/dL (7.5 mmol/L) and then reinstitute EPREX therapy at a dose 25% below the previous dose. Patients should be monitored closely to ensure that the lowest approved effective dose of EPREX is used to provide adequate control of anaemia and of the symptoms of anaemia whilst maintaining a haemoglobin concentration below or at 12 g/dL (7.5 mmol/L). Caution should be exercised with escalation of ESA doses in patients with chronic renal failure. In patients with a poor haemoglobin response to ESA, alternative explanations for the poor response should be considered (see section 4.4 and 5.1). Adult haemodialysis patients In patients on haemodialysis where intravenous access is readily available, administration by the intravenous route is preferable. The treatment is divided into two stages: Eprex_Solution for injection_Sep2021_Ref EU SmPC Jun2021 Page 4 of 25 Correction phase 50 IU/kg, 3 times per week. If necessary, increase or decrease the dose by 25 IU/kg (3 times per week) until the desired haemoglobin concentration range between 10 g/dL to 12 g/dL (6.2 to 7.5 mmol/L) is achieved (this should be done in steps of at least four weeks). Maintenance phase The recommended total weekly dose is between 75 IU/kg and 300 IU/kg. Appropriate adjustment of the dose should be made in order to maintain haemoglobin values within the desired concentration range between 10 g/dL to 12 g/dL (6.2 to 7.5 mmol/l). The clinical data available suggest that those patients whose initial haemoglobin is very low (<6 g/dL or < 3.75 mmol/L) may require higher maintenance doses than those whose initial anaemia is less severe (> 8 g/dL or > 5 mmol/L). Paediatric haemodialysis patients: Anaemia symptoms and sequelae may vary with age, gender, and co-morbid medical conditions; a physician’s evaluation of the individual patient’s clinical course and condition is necessary. In paediatric patients the recommended target haemoglobin range is between 9.5 and 11 g/dl (5.9- 6.8 mmol/l). EPREX should be administered in order to increase haemoglobin to not greater than 11 g/dl (6.8 mmol/l). Patients should be monitored closely to ensure that the lowest approved dose of EPREX is used to provide adequate control of anaemia and of the symptoms of anaemia. The treatment is divided into two stages: In paediatric patients on haemodialysis where intravenous access is readily available, administration by the intravenous route is preferable. Correction phase The starting dose is 50 IU/kg intravenously, 3 times per week. If necessary, increase or decrease the dose by 25 IU/kg (3 times per week) until the desired haemoglobin concentration range of between 9.5 g/dl to 11 g/dl (5.9 to 6.8 mmol/l) is achieved (this should be done in steps of at least four weeks). Maintenance phase: Appropriate adjustment of the dose should be made in order to maintain the haemoglobin levels within the desired range between 9.5 g/dl and 11 g/dl (5.9 to 6.8 mmol/l). Generally, children under 30 kg require higher maintenance doses than children over 30 kg and adults. For example, the following maintenance doses were observed in clinical trials after 6 months of treatment. Eprex_Solution for injection_Sep2021_Ref EU SmPC Jun2021 Page 5 of 25 Dose (IU/kg given 3x week) Weight (kg) Median Usual maintenance dose < 10 100 75-150 10-30 75 60-150 > 30 33 30-100 Available data suggest that those patients whose initial haemoglobin is very low (<6.8 g/dl [4.25 mmol/l] ) may require higher maintenance doses than those whose initial haemoglobin is higher (>6.8 g/dl [4.25 mmol/l ]). Adult patients with renal insufficiency not yet undergoing dialysis Where intravenous access is not readily available EPREX may be administered subcutaneously. The treatment is divided into two stages: Correction phase Starting dose of 50 IU/kg, 3 times per week, followed if necessary by a dosage increase with 25 IU/kg increments (3 times per week) until the desired goal is achieved (this should be done in steps of at least four weeks). Maintenance phase During the maintenance phase, EPREX can be administered either 3 times per week, and in the case of subcutaneous administration, once weekly or once every 2 weeks. Appropriate adjustment of dose and dose intervals should be made in order to maintain haemoglobin values at the desired level: Hb between 10 and 12 g/dL (6.2 7.5 mmol/L). Extending dose intervals may require an increase in dose. The maximum dosage should not exceed 150 IU/kg 3 times per week, 240 IU/kg (up to a maximum of 20,000 IU) once weekly, or 480 IU/kg (up to a maximum of 40,000 IU) once every 2 weeks. Eprex_Solution for injection_Sep2021_Ref EU SmPC Jun2021 Page 6 of 25 Adult peritoneal dialysis patients Where intravenous access is not readily available EPREX may be administered subcutaneously. The treatment is divided into two stages: Correction phase Starting dose of 50 IU/kg, 2 times per week. Maintenance phase The recommended maintenance dose is between 25 IU/kg and 50 IU/kg, 2 times per week in 2 equal injections. Appropriate adjustment of the dose should be made in order to maintain haemoglobin values at the desired level between 10 g/dL to 12 g/dL (6.2 to 7.5 mmol/L). Treatment of patients with chemotherapy-induced anaemia Anaemia symptoms and sequelae may vary with age, gender, and overall burden of disease; a physician’s evaluation of the individual patient’s clinical course and condition is necessary. EPREX should be administered by the subcutaneous route to patients with anaemia (e.g. haemoglobin concentration ≤ 10 g/dL (6.2 mmol/L)). Appropriate adjustment of the dose should be made in order to maintain haemoglobin concentrations within the desired concentration range between 10 g/dl and 12 g/dl (6.2 and 7.5 mmol/l). Due to intra-patient variability, occasional individual haemoglobin concentrations for a patient above and below the desired haemoglobin concentration may be observed. Haemoglobin variability should be addressed through dose management, with consideration for the haemoglobin concentration range between 10 g/dL (6.2 mmol/l) and 12 g/dL (7.5 mmol/L). A sustained haemoglobin concentration of greater than 12 g/dl (7.5 mmol/L) should be avoided; guidance for appropriate dose adjustment for when haemoglobin values exceed 12 g/dL (7.5 mmol/L) are described below. Epoetin alfa therapy should continue until one month after the end of chemotherapy. However, the need to continue Epoetin alfa therapy should be reevaluated periodically. The initial dose is 150 IU/kg given subcutaneously 3 times per week. Alternatively, EPREX can be administered at an initial dose of 40,000IU once weekly. If the haemoglobin has increased by at least 1 g/dL (0.62 mmol/L) or the reticulocyte count has increased ≥ 40,000 cells/mL above baseline after 4 weeks of treatment, the dose should remain at 150 IU/kg 3 times per week or 40,000IU once weekly. If the haemoglobin increase is < 1 g/dL (< 0.62 mmol/L) and the reticulocyte count has increased < 40,000 cells/mL above baseline, increase the dose to 300 IU/kg 3 times per week or 60,000 IU once weekly. . If after an additional 4 weeks of therapy at 300 IU/kg 3 times per week or 60,000 IU once weekly, the haemoglobin has increased ≥ 1 g/dL (≥ 0.62 mmol/L) or the reticulocyte count has increased ≥ 40,000 cells/mL, the dose should remain at 300 IU/kg 3 times per week or 60,000 IU once weekly. Page 7 of 25 However, if the haemoglobin has increased < 1 g/dL (< 0.62 mmol/L) and the reticulocyte count has increased < 40,000 cells/mL above baseline, response is unlikely and treatment should be discontinued. The recommended dosing regimen is described in the following diagram: or 40,000 IU once weekly or 40,000 IU once weekly or 60,000 IU once weekly Patients should be monitored closely to ensure that the lowest approved dose of erythropoiesis- stimulating agent (ESA) is used to provide adequate control of the symptoms of anaemia. Dose adjustment to maintain haemoglobin concentrations between 10g/dl 12 g/dl: If the haemoglobin is rising by more than 2 g/dl (1.25 mmol/l) per month, or if the haemoglobin exceeds 12 g/dl (7.5 mmol/l), reduce the epoetin alfa dose by about 25 50%. If the haemoglobin exceeds 12g/dL (7.5mmol/l), discontinue therapy until it falls below 12 g/dl (7.5 mmol/l) and then reinstitute epoetin alfa therapy at a dose 25% below the previous dose. Adult surgery patients in an autologous predonation programme The intravenous route of administration should be used. At the time of donating blood, epoetin alfa should be administered after the completion of the blood donation procedure. Mildly anaemic patients (haematocrit of 3339%) requiring predeposit of ≥ 4 units of blood should be treated with epoetin alfa at 600 IU/kg, 2 times weekly for 3 weeks prior to surgery. Adult patients scheduled for major elective orthopaedic surgery The subcutaneous route of administration should be used. Prior to initiating treatment with EPREX a hemoglobin level should be obtained to establish that it is 10g/dL ± 1. Page 8 of 25 The recommended dose regimen is 600 IU/kg of epoetin alfa, given weekly for three weeks (days -21, -14 and -7) prior to surgery and on the day of surgery. In cases where there is a medical need to shorten the lead time before surgery to less than three weeks, 300 IU/kg epoetin alfa should be given daily for 10 consecutive days prior to surgery, on the day of surgery and for four days immediately thereafter. When performing haematologic assessments during the preoperative period, if the haemoglobin level reaches 15 g/dl, or higher, administration of epoetin alfa should be stopped and further dosages should not be given. Care should be taken to ensure that at the outset of the treatment patients are not iron-deficient. Zidovudine-treated HIV-infected patients Prior to beginning EPREX, it is recommended that the endogenous serum erythropoietin level be determined (prior to transfusion). Available evidence suggests that patients receiving zidovudine with endogenous serum erythropoietin levels > 500 mUnits/mL are unlikely to respond to therapy with EPREX. Responsiveness to EPREX in HIV-infected patients is dependent upon the endogenous serum erythropoietin level prior to treatment. Patients with endogenous serum erythropoietin levels ≤ 500 mUnits/mL, and who are receiving a dose of zidovudine ≤ 4,200 mg/week, may respond to EPREX therapy. Patients with endogenous serum erythropoietin levels > 500 mUnits/mL do not appear to respond to EPREX therapy. In a series of four clinical trials involving 255 patients, 60% to 80% of HIV- infected patients treated with zidovudine had endogenous serum erythropoietin levels ≤ 500 mUnits/mL. Response to EPREX in zidovudine-treated HIV-infected patients is manifested by reduced transfusion requirements and increased hematocrit. In zidovudine-treated HIV-infected patients the dosage of Eprex should be titrated for each patient to achieve and maintain the lowest hemoglobin level sufficient to avoid the need for blood transfusion and not to exceed the upper safety limit of 12 g/dL. Starting Dose: For adult patients with serum erythropoietin levels ≤500 mUnits/mL who are receiving a dose of zidovudine ≤4200 mg/week, the recommended starting dose of EPREX is 100 IU/kg as an I.V. or S.C. injection TIW (three times a week) for 8 weeks. Increase Dose: During the dose adjustment phase of therapy, the hemoglobin should be monitored weekly. If the response is not satisfactory in terms of reducing transfusion requirements or increasing hemoglobin after 8 weeks of therapy, the dose of EPREX can be increased by 50 to 100 Units/kg TIW. Response should be evaluated every 4 to 8 weeks thereafter and the dose adjusted accordingly by 50 to 100 Units/kg increments TIW. If patients have not responded satisfactorily to an EPREX dose of 300 Units/kg TIW, it is unlikely that they will respond to higher doses of EPREX. Discontinue EPREX if an increase in hemoglobin is not achieved at a dose of 300 Units/kg for 8 weeks. Maintenance Dose: After attainment of the desired response (ie, reduced transfusion requirements or increased hemoglobin), the dose of EPREX should be titrated to maintain the response based on factors such as variations in zidovudine dose and the presence of intercurrent infectious or inflammatory episodes. If the haemoglobin exceeds the upper safety limit of 12 g/dL, the dose should be discontinued until the hemoglobin drops to 11 g/dL. The dose should be reduced by 25% when treatment is resumed and then titrated to maintain the desired hemoglobin. Page 9 of 25

פרטי מסגרת הכללה בסל
התרופה תינתן בכל אחד מאלה: 1. אנמיה חמורה (severe anemia) בחולי אי ספיקה כלייתית כרונית. 2. חולים אנמיים הסובלים ממחלה ממאירה והמקבלים טיפול פעיל ייעודי במחלתם וכן לחולים הסובלים ממיאלומה נפוצה (multiple myeloma) או מהתסמונת המיאלודיספלסטית (myelodisplastic syndrome) שנתקיימו בהם כל אלה: 1. אחד מהתנאים האלה: א. רמת המוגלובין נמוכה מ-8 גרם %. ב. החולה מרותק למיטתו בגלל אנמיה המלווה במחלת לב איסכמית או באי ספיקה לבבית. ג. החולה נזקק לקבלת שתי מנות דם לפחות פעם בשבועיים במשך חודשיים. 2. נשללה סיבה אחרת לאנמיה שאינה קשורה לטיפול הייעודי במחלתם האמורה לעיל ובכלל זה דימום, חוסר ברזל, חוסר חומצה פולית, חוסר ויטמין B12 והמוליזה. 3. רמת אריתרופואטין בנסיוב נמוכה מ-100 mu/ml.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| חולים אנמיים הסובלים ממחלה ממאירה והמקבלים טיפול פעיל ייעודי במחלתם וכן לחולים הסובלים ממיאלומה נפוצה (multiple myeloma) או מהתסמונת המיאלודיספלסטית (myelodisplastic syndrome | 01/02/2001 | המטולוגיה | ||
| אנמיה חמורה (severe anemia) בחולי אי ספיקה כלייתית כרונית. | 01/02/2001 | המטולוגיה | ||
| oncology | 01/02/2001 | DARBEPOETIN ALFA, EPOETIN ALFA, EPOETIN BETA, EPOETIN THETA (R-HUEPO) | ||
| CKD | 01/02/2001 | DARBEPOETIN ALFA, EPOETIN BETA, EPOETIN ALFA, METHOXY POLYETHYLENE GLYCOL-EPOETIN BETA, EPOETIN THETA (R-HUEPO) |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/02/2001
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
