Quest for the right Drug
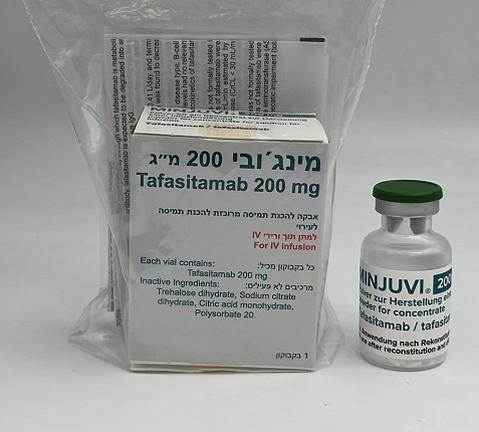
מינג'ובי 200 מ"ג Minjuvi 200mg (TAFASITAMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most common adverse reactions are: infections (73%), neutropenia (51%), asthenia (40%), anaemia (36%), diarrhoea (36%), thrombocytopenia (31%), cough (26%), oedema peripheral (24%), pyrexia (24%), decreased appetite (22%). The most common serious adverse reactions were infection (26%) including pneumonia (7%), and febrile neutropenia (6%). Permanent discontinuation of tafasitamab due to an adverse reaction occurred in 15% of patients. The most common adverse reactions leading to permanent discontinuation of tafasitamab were infections and infestations (5%), nervous system disorders (2.5%), and respiratory, thoracic and mediastinal disorders (2.5%). The frequency of dose modification or interruption due to adverse reactions was 65%. The most common adverse reactions leading to tafasitamab treatment interruption were blood and lymphatic system disorders (41%). Tabulated list of adverse reactions Adverse reactions reported in clinical trials are listed by MedDRA System Organ Class and by frequency. The frequencies of adverse reactions is based on the pivotal phase 2 trial MOR208C203 (L-MIND) with 81 patients. Patients were exposed to tafasitamab for a median of 7.7 months. The adverse reaction frequencies from clinical trials are based on all-cause adverse event frequencies, where a proportion of the events for an adverse reaction may have other causes than the medicinal product, such as the disease, other medicines or unrelated causes. Frequencies are defined as follows: very common (≥ 1/10); common (≥ 1/100 to < 1/10); uncommon (≥ 1/1,000 to < 1/100); rare (≥ 1/10,000 to < 1/1,000); very rare (< 1/10,000); and not known (cannot be estimated from the available data). Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness. Table 2: Adverse reactions in patients with relapsed or refractory DLBCL who received tafasitamab in the clinical trial MOR208C203 (L-MIND) System organ class Frequency Adverse reactions Infections and infestations Very common Bacterial, viral and fungal infections+, including opportunistic infections with fatal outcomes (e.g. bronchopulmonary aspergillosis, bronchitis, pneumonia and urinary tract infection) Common Sepsis (including neutropenic sepsis) Neoplasms benign, Common Basal cell carcinoma malignant and unspecified (incl. cysts and polyps) Blood and lymphatic system Very common Febrile neutropenia+, neutropenia+, disorders thrombocytopenia+, anaemia, leukopenia+ Common Lymphopenia Immune system disorders Common Hypogammaglobulinaemia Metabolism and nutrition Very common Hypokalaemia, decreased appetite disorders Common Hypocalcaemia, hypomagnesaemia Nervous system disorders Common Headache, paraesthesia, dysgeusia Respiratory, thoracic and Very common Dyspnoea, cough mediastinal disorders Common Exacerbation of chronic obstructive pulmonary disease, nasal congestion Gastrointestinal disorders Very common Diarrhoea, constipation, vomiting, nausea, abdominal pain Hepatobiliary disorders Common Hyperbilirubinaemia, transaminases increased (includes ALT and/or AST increased), Gamma-glutamyltransferase increased Skin and subcutaneous Very common Rash (includes different types of rash, e.g. rash, tissue disorders rash maculopapular, rash pruritic, rash erythematous) Common Pruritus, alopecia, erythema, hyperhidrosis Musculoskeletal and Very common Back pain, muscle spasms connective tissue disorders Common Arthralgia, pain in extremity, musculoskeletal pain Renal and urinary disorders Common Blood creatinine increased General disorders and Very common Asthenia++, oedema peripheral, pyrexia administration site Common Mucosal inflammation conditions Investigations Common Weight decreased, C-reactive protein increased Injury, poisoning and Common Infusion related reaction procedural complications +Further information on this adverse reaction is provided in the text below. ++ Asthenia includes asthenia, fatigue and malaise. Compared with the incidences on combination therapy with lenalidomide, the incidences of non-haematological adverse reactions on tafasitamab monotherapy decreased by at least 10% for decreased appetite, asthenia, hypokalaemia, constipation, nausea, muscle spasms, dyspnoea and C-reactive protein increased. Description of selected adverse reactions Myelosuppression Treatment with tafasitamab can cause serious or severe myelosuppression including neutropenia, thrombocytopenia and anaemia (see sections 4.2 and 4.4). In the L-MIND study, myelosuppression (i.e. neutropenia, febrile neutropenia, thrombocytopenia, leukopenia, lymphopenia or anaemia) occurred in 65.4% of patients treated with tafasitamab. Myelosuppression was managed by reduction or interruption of lenalidomide, interruption of tafasitamab and/or administration of G-CSF (see sections 4.2 and 4.4). Myelosuppression led to interruption of tafasitamab in 41% and to tafasitamab discontinuation in 1.2%. Neutropenia/febrile neutropenia Incidence of neutropenia was 51%. Incidence of Grade 3 or 4 neutropenia was 49% and of Grade 3 or 4 febrile neutropenia was 12%. Median duration of any adverse reaction of neutropenia was 8 days (range 1 – 222 days); median time to onset to first occurrence of neutropenia was 49 days (range 1 – 994 days). Thrombocytopenia Incidence of thrombocytopenia was 31%. Incidence of Grade 3 or 4 thrombocytopenia was 17%. Median duration of any adverse reaction thrombocytopenia was 11 days (range 1 – 470 days); median time to onset to first occurrence of thrombocytopenia was 71 days (range 1 – 358 days). Anaemia Incidence of anaemia was 36%. Incidence of Grade 3 or 4 anaemia was 7%. Median duration of any adverse reaction of anaemia was 15 days (range 1 – 535 days); median time to onset to first occurrence of anaemia was 49 days (range 1 – 1129 days). When patients in the L-MIND study were switched from tafasitamab and lenalidomide in the combination therapy phase to tafasitamab alone in the extended monotherapy phase, the incidences of haematological events decreased by at least 20% for neutropenia, thrombocytopenia and anaemia; no incidences of febrile neutropenia were reported with tafasitamab monotherapy (see sections 4.2 and 4.4). Infections In the L-MIND study, infections occurred in 73% of patients. Incidence of Grade 3 or 4 infections was 28%. The most frequently reported Grade 3 or higher infections were pneumonia (7%), respiratory tract infections (4.9%), urinary tract infections (4.9%) and sepsis (4.9%). Infection was fatal in < 1% of patients (pneumonia) within 30 days of last treatment. Median time to first onset of Grade 3 or 4 infection was 62.5 days (4 – 1014 days). Median duration of any infection was 11 days (1 – 392 days). Recommendations for management of infections are provided in section 4.4. Infection led to dose interruption of tafasitamab in 27% and tafasitamab discontinuation in 4.9%. Infusion-related reactions In the L-MIND study, infusion-related reactions occurred in 6% of patients. All infusion related reactions were Grade 1 and resolved on the day of occurrence. Eighty percent of these reactions occurred during cycle 1 or 2. Symptoms included chills, flushing, dyspnoea and hypertension (see sections 4.2 and 4.4). Immunogenicity In 245 patients treated with tafasitamab, no treatment-emergent or treatment-boosted anti-tafasitamab antibodies were observed. Pre-existing anti-tafasitamab antibodies were detected in 17/245 patients (6.9%) with no impact on pharmacokinetics, efficacy or safety of tafasitamab. Special populations Elderly Among 81 patients treated in the L-MIND study, 56 (69%) patients were > 65 years of age. Patients > 65 years of age had a numerically higher incidence of serious treatment emergent adverse events (TEAEs) (55%) than patients ≤ 65 years (44%). Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/

פרטי מסגרת הכללה בסל
א. התכשיר יינתן לטיפול בחולי לימפומה מסוג DLBCL, בשילוב לנלידומיד, לאחר קו טיפול אחד לפחות, בחולים שלא מתאימים להשתלה. ב. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מהבאים – Polatuzumab vedotin, Selinexor, Tafasitamabג. מתן התרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התכשיר יינתן לטיפול בחולי לימפומה מסוג DLBCL, בשילוב לנלידומיד, לאחר קו טיפול אחד לפחות, בחולים שלא מתאימים להשתלה. ב. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מהבאים – Polatuzumab vedotin, Selinexor, Tafasitamab ג. מתן התרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה. | 01/02/2023 | המטולוגיה | DLBCL, Diffuse large B cell lymphoma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/02/2023
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
