Quest for the right Drug
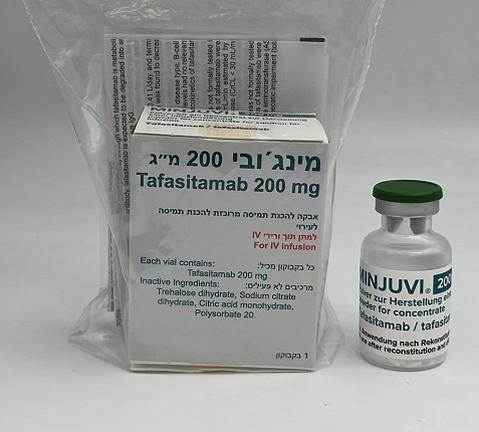
מינג'ובי 200 מ"ג Minjuvi 200mg (TAFASITAMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, monoclonal antibodies, ATC code: L01FX12. Mechanism of action Tafasitamab is an Fc-enhanced monoclonal antibody that targets the CD19 antigen expressed on the surface of pre-B and mature B lymphocytes. Upon binding to CD19, tafasitamab mediates B-cell lysis through: • engagement of immune effector cells like natural killer cells, γδ T cells and phagocytes • direct induction of cell death (apoptosis) The Fc modification results in enhanced antibody-dependent cellular cytotoxicity and antibody-dependent cellular phagocytosis. Pharmacodynamic effects In patients with relapsed or refractory DLBCL, tafasitamab led to a reduction in peripheral blood B-cell counts. The reduction relative to baseline B-cell count reached 97% after eight days of treatment in the L-MIND study. The maximum B-cell reduction at approximately 100% (median) was reached within 16 weeks of treatment. Although the depletion of B-cells in the peripheral blood is a measurable pharmacodynamic effect, it is not directly correlated with the depletion of B-cells in solid organs or in malignant deposits. Clinical efficacy Tafasitamab plus lenalidomide followed by tafasitamab monotherapy was studied in the L-MIND study, an open-label multicentre single-arm study. This study was conducted in adult patients with relapsed or refractory DLBCL after 1 to 3 prior systemic DLBCL therapies, who at the time of the trial were not candidates for high dose chemotherapy followed by ASCT or who had refused ASCT. One of the prior systemic therapies had to include a CD20 targeted therapy. The study excluded patients with severe hepatic impairment (total serum bilirubin > 3 mg/dL) and patients with renal impairment (CrCL< 60 mL/min.), as well as patients with history or evidence of clinically significant cardiovascular, CNS and/or other systemic disease. Patients with a known history of “double/triple-hit” genetics DLBCL were also excluded at study entry. For the first three cycles, patients received 12 mg/kg tafasitamab via infusion on day 1, 8, 15 and 22 of each 28-day cycle, plus a loading dose on day 4 of cycle 1. Thereafter, tafasitamab was administered on days 1 and 15 of each cycle until disease progression. Premedication including antipyretics, histamine H1 and H2 receptor blockers and glucocorticosteroids was given 30 to 120 minutes prior to the first three tafasitamab infusions. Patients self-administered 25 mg lenalidomide daily on days 1 to 21 of each 28-day cycle, up to 12 cycles. A total of 81 patients were enrolled in the L-MIND study. The median age was 72 years (range 41 to 86 years), 89% were white and 54% were males. Out of 81 patients, 74 (91.4%) had ECOG performance score of 0 or 1 and 7 (8.6%) had ECOG score of 2. The median number of prior therapies was two (range: 1 to 4), with 40 patients (49.4%) receiving one prior therapy and 35 patients (43.2%) receiving 2 prior lines of treatment. Five patients (6.2%) had 3 prior lines of therapies and 1 (1.2%) had 4 prior lines of treatment. All patients had received a prior anti-CD20-containing therapy. Eight patients had a diagnosis of DLBCL transformed from low-grade lymphoma. Fifteen patients (18.5%) had primary refractory disease, 36 (44.4%) were refractory to their last prior therapy, and 34 (42.0%) were refractory to rituximab. Nine patients (11.1%) had received prior ASCT. The primary reasons for patients not being candidates for ASCT included age (45.7%), refractory to salvage chemotherapy (23.5%), comorbidities (13.6%) and refusal of high dose chemotherapy/ASCT (16.0%). One patient received tafasitamab, but not lenalidomide. The remaining 80 patients received at least one dose of tafasitamab and lenalidomide. All patients enrolled in the L-MIND study had a diagnosis of DLBCL based on local pathology. However, as per central pathology review, 10 patients could not be classified as DLBCL. The median duration of exposure to treatment was 9.2 months (range: 0.23, 54.67 months). Thirty-two (39.5%) patients completed 12 cycles of tafasitamab. Thirty (37.0%) patients completed 12 cycles of lenalidomide. The primary efficacy endpoint was best objective response rate (ORR), defined as the proportion of complete and partial responders, as assessed by an independent review committee (IRC). Other efficacy endpoints included duration of response (DoR), progression-free survival (PFS) and overall survival (OS). The efficacy results are summarised in Table 3. Table 3: Efficacy results in patients with relapsed or refractory diffuse large B-cell lymphoma in the MOR208C203 (L-MIND) study Efficacy parameter Tafasitamab + lenalidomide (N = 81 [ITT]*) 30-NOV-2019 cut-off 30-OCT-2020 cut-off (24 months analysis) (35 months analysis) Primary endpoint Best objective response rate (per IRC) Overall response rate, n (%) 46 (56.8) 46 (56.8) (95% CI) [45.3, 67.8] [45.3, 67.8] Complete response rate, n 32 (39.5) 32 (39.5) (%) [28.8, 51.0] [28.8, 51.0] (95% CI) Partial response rate, n (%) 14 (17.3) 14 (17.3) (95% CI) [ 9.8, 27.3] [ 9.8, 27.3] Secondary endpoint Overall duration of response (complete + partial response) a Median, months 34.6 43.9 (95% CI) [26.1, NR] [26.1, NR] ITT = intention to treat; NR = not reached *One patient received only tafasitamab CI: Binomial exact confidence interval using Clopper Pearson method a Kaplan Meier estimates Overall survival (OS) was a secondary endpoint in the study. After a median follow up time of 42.7 months (95% CI: 38.0; 47.2), the median OS was 31.6 months (95% CI: 18.3; not reached). Amongst the eight patients who had a DLBCL transformed from a prior indolent lymphoma, seven patients had an objective response (three patients a CR, four patients a PR) and one patient had a stable disease as the best response to tafasitamab+ lenalidomide treatment. Elderly In the ITT set, 36 of 81 patients were ≤ 70 years and 45 of 81 patients were > 70 years. No overall differences in efficacy were observed for patients ≤ 70 years versus patients > 70 years of age. Paediatric population The European Medicines Agency has waived the obligation to submit the results of studies with MINJUVI 200 mg in all subsets of the paediatric population in diffuse large B-cell lymphoma (see section 4.2 for information on paediatric use). This medicinal product has been authorised under a so-called ‘conditional approval’ scheme. This means that further evidence on this medicinal product is awaited. The European Medicines Agency will review new information on this medicinal product at least every year and this SmPC will be updated as necessary.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The absorption, distribution, biotransformation and elimination were documented based on a population pharmacokinetic analysis. Absorption Based on an analysis of tafasitamab in combination with lenalidomide, tafasitamab average serum trough concentrations (± standard deviation) were 179 (± 53) μg/mL during weekly (plus an additional dose on day 4 of cycle 1) intravenous administrations of 12 mg/kg. During administration every 14 days from cycle 4 onwards, average trough serum concentrations were 153 (± 68) μg/mL. Overall maximum tafasitamab serum concentrations were 483 (± 109) μg/mL. Distribution The total volume of distribution for tafasitamab was 9.3 L. Biotransformation The exact pathway through which tafasitamab is metabolised has not been characterised. As a human IgG monoclonal antibody, tafasitamab is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG. Elimination The clearance of tafasitamab was 0.41 L/day and terminal elimination half-life was 16.9 days. Following long-term observations, tafasitamab clearance was found to decrease over time to 0.19 L/day after two years. Special populations Age, body weight, sex, tumour size, disease type, B-cell or absolute lymphocyte counts, anti-drug antibodies, lactate dehydrogenase and serum albumin levels had no relevant effect on the pharmacokinetics of tafasitamab. The influence of race and ethnicity on the pharmacokinetics of tafasitamab is unknown. Renal impairment The effect of renal impairment was not formally tested in dedicated clinical trials; however, no clinically meaningful differences in the pharmacokinetics of tafasitamab were observed for mild to moderate renal impairment (creatinine clearance (CrCL) ≥ 30 and < 90 mL/min estimated by the Cockcroft-Gault equation). The effect of severe renal impairment to end-stage renal disease (CrCL < 30 mL/min) is unknown. Hepatic impairment The effect of hepatic impairment was not formally tested in dedicated clinical trials; however no clinically meaningful differences in the pharmacokinetics of tafasitamab were observed for mild hepatic impairment (total bilirubin ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN, or total bilirubin 1 to 1.5 times ULN and any AST). The effect of moderate to severe hepatic impairment (total bilirubin > 1.5 times ULN and any AST) is unknown.

פרטי מסגרת הכללה בסל
א. התכשיר יינתן לטיפול בחולי לימפומה מסוג DLBCL, בשילוב לנלידומיד, לאחר קו טיפול אחד לפחות, בחולים שלא מתאימים להשתלה. ב. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מהבאים – Polatuzumab vedotin, Selinexor, Tafasitamabג. מתן התרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התכשיר יינתן לטיפול בחולי לימפומה מסוג DLBCL, בשילוב לנלידומיד, לאחר קו טיפול אחד לפחות, בחולים שלא מתאימים להשתלה. ב. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מהבאים – Polatuzumab vedotin, Selinexor, Tafasitamab ג. מתן התרופה ייעשה לפי מרשם של רופא מומחה בהמטולוגיה. | 01/02/2023 | המטולוגיה | DLBCL, Diffuse large B cell lymphoma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/02/2023
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
