Quest for the right Drug
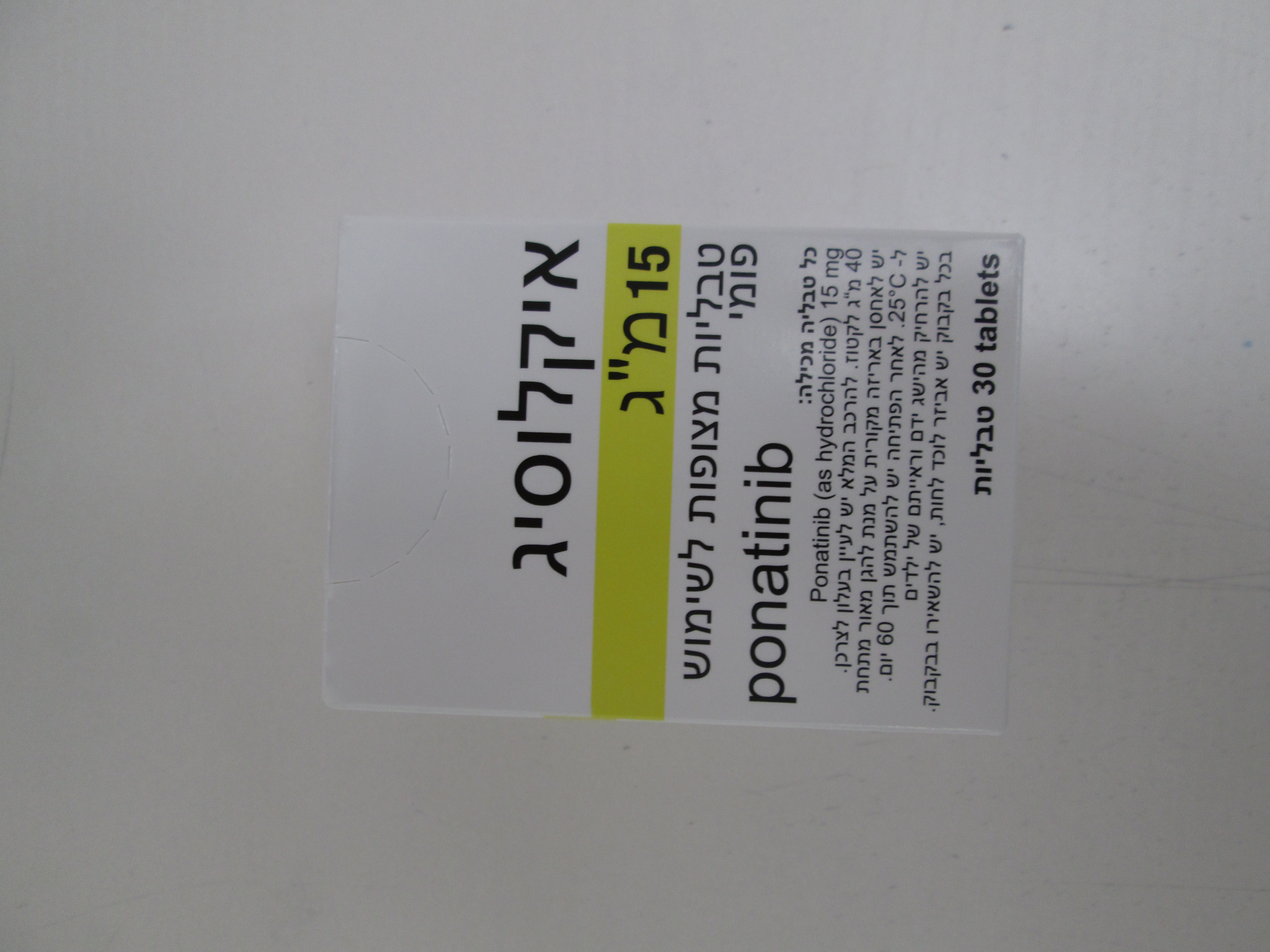
איקלוסיג 15 מ"ג ICLUSIG 15 MG (PONATINIB AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות : COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The adverse reactions described in this section were identified in a single-arm, open-label, international, multicenter trial in 449 CML and Ph+ ALL patients who were resistant or intolerant to prior TKI therapy including those with a BCR-ABL T315I mutation. All patients received 45 mg Iclusig once daily. Dose adjustments to 30 mg once daily or 15 mg once daily were allowed for the management of treatment toxicity. Additionally, after approximately 2 years of follow-up, all patients who were still taking a 45 mg daily dose were recommended to undergo a dose reduction, even in the absence of adverse events, in response to the continued occurrence of vascular occlusive events in the clinical trial. At the time of reporting, all ongoing patients had a minimum follow-up of 64 months. The median duration of treatment with Iclusig was 32.2 months in CP-CML patients, 19.4 months in AP-CML patients, and 2.9 months in BP-CML/Ph+ ALL patients. The median dose intensity was 28 mg/day in CP-CML patients or, 63% of the expected 45 mg dose; median dose intensity was greater in advanced disease states (32 mg/day in the AP-CML patients and 44 mg/day in the BP CML/Ph+ ALL patients). The most common serious adverse reactions > 2% (treatment-emergent frequencies) were pneumonia (7.3%), pancreatitis (5.8%), abdominal pain (4.7 atrial fibrillation (4.5%), pyrexia (4.5%), myocardial infarction (4.0%), peripheral arterial occlusive disease (3.8%), anaemia (3.8%), angina pectoris (3.3%), platelet count decreased (3.1%), febrile neutropenia (2.9%), hypertension (2.9%), coronary artery disease (2.7%), cardiac failure congestive (2.4%), cerebrovascular accident (2.4%), sepsis (2.4%), cellulitis (2.2%), acute kidney injury (2.0%), urinary tract infection (2.0%) and lipase increased (2.0%). Serious arterial cardiovascular, cerebrovascular, and peripheral vascular occlusive adverse reactions (treatment-emergent frequencies) occurred in 10%, 7%, and 9% of Iclusig treated patients, respectively. Serious venous occlusive reactions (treatment-emergent frequencies) occurred in 5% of patients. Arterial cardiovascular, cerebrovascular, and peripheral vascular occlusive adverse reactions (treatment-emergent frequencies) occurred in 13%, 9%, and 11% of Iclusig-treated patients, respectivelyOverall arterial occlusive adverse reactions have occurred in 25% of Iclusig-treated patients from the phase 2 trial, with serious adverse reactions occurring in 20% of patients. Some patients experienced more than one type of event. Venous thromboembolic reactions (treatment-emergent frequencies) occurred in 6% of patients. The incidence of thromboembolic events is higher in patients with Ph+ ALL or BP-CML than those with AP-CML or CP-CML. No venous occlusive events were fatal. After a minimum follow-up of 64 months, the rates of adverse reactions resulting in discontinuation were 20% in CP-CML, 11% in AP-CML, 15% in BP-CML and 9% in Ph+ ALL. Tabulated list of adverse reactions Adverse reactions reported in all CML and Ph+ ALL patients are presented in Table 4. Frequency categories are very common (≥ 1/10), common (≥ 1/100 to < 1/10) and uncommon (≥ 1/1000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), and not known (cannot be estimated from the available data). Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness. Table 4 Adverse reactions observed in CML and Ph+ ALL patients – frequency reported by incidence of treatment emergent events System organ class Frequency Adverse reactions Very common upper respiratory tract infection Infections and infestations Common pneumonia, sepsis, folliculitis, cellulitis anaemia, platelet count decreased, neutrophil Very common count decreased Blood and lymphatic system pancytopenia, febrile neutropenia, white disorders Common blood cell count decreased, lymphocyte count decreased Endocrine disorders Common hypothyroidism Very common decreased appetite dehydration, fluid retention, hypocalcaemia, hyperglycaemia, hyperuricaemia, Metabolism and nutrition Common hypophosphataemia, hypertriglyceridaemia, disorders hypokalaemia, weight decreased, hyponatraemia Uncommon tumour lysis syndrome Psychiatric disorders Very common insomnia Very common headache, dizziness cerebrovascular accident, cerebral infarction, neuropathy peripheral, lethargy, migraine, Common hyperaesthesia, hypoaesthesia, paraesthesia, Nervous system disorders transient ischaemic attack cerebral artery stenosis, cerebral haemorrhage, haemorrhage intracranial, Uncommon posterior reversible encephalopathy syndrome * vision blurred, dry eye, periorbital oedema, Common eyelid oedema, conjunctivitis, visual Eye disorders impairment retinal vein thrombosis, retinal vein Uncommon occlusion, retinal artery occlusion cardiac failure, myocardial infarction, cardiac failure congestive, coronary artery Common disease, angina pectoris, pericardial effusion, atrial fibrillation, ejection fraction decreased, Cardiac disorders acute coronary syndrome, atrial flutter myocardial ischemia, cardiac discomfort, Uncommon ischemic cardiomyopathy, arteriospasm coronary, left ventricular dysfunction, Vascular disorders Very common hypertension System organ class Frequency Adverse reactions peripheral arterial occlusive disease, peripheral ischaemia, peripheral artery Common stenosis, intermittent claudication, deep vein thrombosis, hot flush, flushing poor peripheral circulation, splenic infarction, embolism venous, venous Uncommon thrombosis, hypertensive crisis, renal artery stenosis Not Known Aneurysms and artery dissections Very common dyspnoea, cough Respiratory, thoracic and pulmonary embolism, pleural effusion, mediastinal disorders Common epistaxis, dysphonia, pulmonary hypertension abdominal pain, diarrhoea, vomiting, Very common constipation, nausea, lipase increased pancreatitis, blood amylase increased, Gastrointestinal disorders gastrooesophageal reflux disease, stomatitis, Common dyspepsia, abdominal distension, abdominal discomfort, dry mouth, gastric haemorrhage alanine aminotransferase increased, aspartate Very common aminotransferase increased blood bilirubin increased, blood alkaline Hepatobiliary disorders Common phosphatase increased, gamma- glutamyltransferase increased Uncommon hepatotoxicity, hepatic failure, jaundice Very common rash, dry skin, pruritus rash pruritic, exfoliative rash, erythema, alopecia, skin exfoliation, night sweats, Common hyperhidrosis, petechia, ecchymosis, pain of Skin and subcutaneous tissue skin, dermatitis exfoliative, hyperkeratosis, disorders skin hyperpigmentation Rare panniculitis(including erythema nodosum) bone pain, arthralgia, myalgia, pain in Very common Musculoskeletal and extremity, back pain, muscle spasms connective tissue disorders musculoskeletal pain, neck pain, Common musculoskeletal chest pain Reproductive system and Common erectile dysfunction breast disorders fatigue, asthenia, oedema peripheral, Very common General disorders and pyrexia, pain administrative site conditions chills, influenza like illness, non-cardiac Common chest pain, mass, face oedema * Spontaneous reports from post-marketing experience Description of selected adverse reactions Vascular occlusion (see section 4.2 and 4.4). Serious vascular occlusion has occurred in patients treated with Iclusig, including cardiovascular, cerebrovascular and peripheral vascular events, and venous thrombotic events. Patients with and without cardiovascular risk factors, including patients age 50 years or younger, experienced these events. Arterial occlusive adverse events were more frequent with increasing age and in patients with history of ischaemia, hypertension, diabetes, or hyperlipidaemia. Myelosuppression Myelosuppression was commonly reported in all patient populations. The frequency of Grade 3 or 4 thrombocytopenia, neutropenia, and anaemia was higher in patients with AP-CML and BP-CML/Ph+ ALL than in patients with CP-CML (see Table 5). Myelosuppression was reported in patients with normal baseline laboratory values as well as in patients with pre-existing laboratory abnormalities. Discontinuation due to myelosuppression was infrequent (thrombocytopenia 4%, neutropenia and anaemia < 1% each). Hepatitis B reactivation Hepatitis B reactivation has been reported in association with BCR-ABL TKIs. Some cases resulted in acute hepatic failure or fulminant hepatitis leading to liver transplantation or a fatal outcome (see section 4.4). Severe Cutaneous Adverse Reactions (SCARs) Severe skin reactions (such as Stevens-Johnson Syndrome) have been reported with some BCR-ABL Tyrosine Kinase Inhibitors. Patients should be warned to immediately report suspected skin reactions, especially if associated with blistering, peeling, mucosal involvement or systemic symptoms. Table 5 Incidence of clinically relevant grade 3/4* laboratory abnormalities in ≥ 2% of patients in any disease group from the Phase 2 Trial (N=449): minimum follow-up of 64 month for all ongoing patients Laboratory test All patients CP-CML AP-CML BP-CML/Ph+ (N=449) (N=270) (N=85) ALL (N=94) (%) (%) (%) (%) Haematology Thrombocytopenia (platelet count 40 35 49 46 decreased) Neutropenia (ANC decreased) 34 23 52 52 Leukopenia (WBC decreased) 25 12 37 53 Anaemia (Hgb decreased) 20 8 31 46 Lymphopenia 17 10 25 28 Biochemistry Lipase increased 14 14 13 14 Phosphorus decreased 10 10 13 9 Glucose increased 7 8 13 1 ALT increased 6 4 8 7 Sodium decreased 5 6 6 2 AST increased 4 3 5 3 Amylase increased 4 4 4 3 Potassium decreased 2 <1 6 2 Potassium increased 2 2 1 3 Alkaline phosphatase increased 2 2 4 2 Bilirubin 1 <1 2 1 Calcium decreased 1 <1 2 1 ALT=alanine aminotransferase, ANC=absolute neutrophil count, AST=aspartate aminotransferase, Hgb=haemoglobin, WBC=white blood cell count. *Reported using National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. לוקמיה מסוג CML בחולים עם מוטציה מסוג T315I או בחולה עם עמידות או חוסר סבילות למעכבי טירוזין קינאז.2. לוקמיה מסוג Ph+ ALL בחולים עם מוטציה מסוג T315I או בחולה עם עמידות או חוסר סבילות למעכבי טירוזין קינאז.ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לוקמיה מסוג Ph+ ALL בחולים עם מוטציה מסוג T315I או בחולה עם עמידות או חוסר סבילות למעכבי טירוזין קינאז. | ||||
| לוקמיה מסוג CML בחולים עם מוטציה מסוג T315I או בחולה עם עמידות או חוסר סבילות למעכבי טירוזין קינאז. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
