Quest for the right Drug
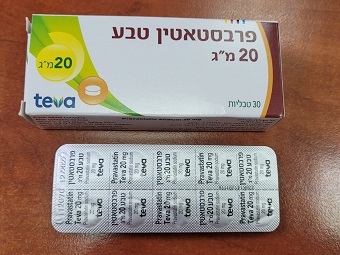
פרבסטאטין טבע 20 מ"ג PRAVASTATIN TEVA 20 MG (PRAVASTATIN SODIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1. Pharmacodynamic properties Pharmacotherapeutic group Serum lipid reducing agents/cholesterol and triglyceride reducers/HMG-CoA reductase inhibitors ATC-Code: C10AA03 Mechanism of action Pravastatin is a competitive inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, the enzyme catalysing the early rate-limiting step in cholesterol biosynthesis, and produces its lipid-lowering effect in two ways. Firstly, with the reversible and specific competitive inhibition of HMG-CoA reductase, it effects modest reduction in the synthesis of intracellular cholesterol. This results in an increase in the number of LDL-receptors on cell surfaces and enhanced receptor-mediated catabolism and clearance of circulating LDL-cholesterol. Secondly, pravastatin inhibits LDL production by inhibiting the hepatic synthesis of VLDL cholesterol, the LDL- cholesterol precursor. In both healthy subjects and patients with hypercholesterolaemia, Pravastatin Teva lowers the following lipid values: total cholesterol, LDL cholesterol, apolipoprotein B, VLDL-cholesterol and triglycerides, while HDL cholesterol and apolipoprotein A are elevated. Clinical efficacy Primary prevention The "West of Scotland Coronary Prevention Study (WOSCOPS)" was a randomised, double-blind, placebo-controlled trial among 6,595 male patients aged from 45 to 64 years with moderate to severe hypercholesterolaemia (LDL-C: 155-232 mg/dl [4.0- 6.0 mmol/l]) and with no history of myocardial infarction, treated for an average duration of 4.8 years with either a 40 mg daily dose of pravastatin or placebo as an adjunct to diet. In pravastatin-treated patients, results showed: - a decrease in the risk of mortality from coronary disease and of non-lethal myocardial infarction (relative risk reduction RRR was 31%; p = 0.0001 with an absolute risk of 7.9% in the placebo group, and 5.5% in pravastatin-treated patients); the effects on these cumulative cardiovascular events rates being evident as early as 6 months of treatment; - a decrease in the total number of deaths from a cardiovascular event (RRR 32%; p = 0.03); - when risk factors were taken into account, a RRR of 24% (p = 0.039) in total mortality was also observed among patients treated with pravastatin; - a decrease in the relative risk for undergoing myocardial revascularisation procedures (coronary artery bypass graft surgery or coronary angioplasty) by 37% (p = 0.009) and coronary angiography by 31% (p = 0.007). The benefit of the treatment on the criteria indicated above is not known in patients over the age of 65 years, who could not be included in the study. In the absence of data in patients with hypercholesterolaemia associated with a triglyceride level of more than 6 mmol/l (5.3 g/l) after a diet for 8 weeks, in this study, the benefit of pravastatin treatment has not been established in this type of patients. Secondary prevention The "Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID)" was a multicenter, randomised, double-blind, placebo-controlled study comparing the effects of pravastatin (40 mg OD) with placebo in 9014 patients aged 31 to 75 years for an average duration of 5.6 years with normal to elevated serum cholesterol levels (baseline total cholesterol = 155 to 271 mg/dl [4.0-7.0 mmol/l], mean total cholesterol = 219 mg/dl [5.66 mmol/l]) and with variable triglyceride levels of up to 443 mg/dl [5.0 mmol/l] and with a history of myocardial infarction or unstable angina pectoris in the preceding 3 to 36 months. Treatment with pravastatin significantly reduced the relative risk of Coronary Heart Disease (CHD) death by 24% (p = 0.0004, with an absolute risk of 6.4% in the placebo group, and 5.3% in pravastatin-treated patients), the relative risk of coronary events (either CHD death or nonfatal myocardial infarction (MI)) by 24% (p < 0.0001) and the relative risk of fatal or nonfatal myocardial infarction (MI) by 29% (p < 0.0001). In pravastatin-treated patients, results showed: - a reduction in the relative risk of total mortality by 23% (p < 0.0001) and cardiovascular mortality by 25% (p < 0.0001); - a reduction in the relative risk of undergoing myocardial revascularisation procedures (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) by 20% (p < 0.0001); - a reduction in the relative risk of stroke by 19% (p = 0.048). The "Cholesterol and Recurrent Events (CARE)" study was a randomised, double-blind, placebo- controlled study comparing, the effects of pravastatin (40 mg OD) on coronary heart disease death and non-fatal myocardial infarction (MI) for an average of 4.9 years in 4,159 patients aged 21 to 75 years, with normal total cholesterol levels (baseline mean total cholesterol < 240 mg/dl), who had experienced a myocardial infarction (MI) in the preceding 3 to 20 months. Treatment with pravastatin significantly reduced: - the rate of a recurrent coronary event (either coronary heart disease death or non-fatal MI) by 24% (p = 0.003, placebo 13.3%, Pravastatin 10.4%); - the relative risk of undergoing revascularisation procedures (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) by 27% (p < 0.001). The relative risk of stroke was also reduced by 32% (p = 0.032), and stroke or transient ischemic attack (TIA) combined by 27% (p = 0.02). The benefit of the treatment on the above criteria is not known in patients over the age of 75 years, who could not be included in the CARE and LIPID studies. In the absence of data in patients with hypercholesterolaemia associated with a triglyceride level of more than 4 mmol/l (3.5 g/l) or more than 5 mmol/l (4.45 g/l) after following a diet for 4 or 8 weeks, in the CARE and LIPID studies, respectively, the benefit of treatment with Pravastatin has not been established in this type of patients. In the CARE and LIPID studies, about 80% of patients had received acetyl-salicylic acid (ASA) as part of their regimen.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption: Pravastatin is administered orally in the active form. It is rapidly absorbed; peak serum levels are achieved 1 to 1.5 hours after ingestion. On average, 34% of the orally administered dose is absorbed, with an absolute bioavailability of 17%. The presence of food in the gastrointestinal tract leads to a reduction in the bioavailability, but the cholesterol-lowering effect of pravastatin is identical whether taken with or without food. After absorption, 66% of pravastatin undergoes a first-pass extraction through the liver, which is the primary site of its action and the primary site of cholesterol synthesis and clearance of LDL-cholesterol. In vitro studies demonstrated that pravastatin is transported into hepatocytes and with substantially less intake in other cells. In view of this substantial first pass through the liver, plasma concentrations of pravastatin have only a limited value in predicting the lipid-lowering effect. The plasma concentrations are proportional to the doses administered. Distribution: About 50% of circulating pravastatin is bound to plasma proteins. The volume of distribution is about 0.5 l/kg. A small quantity of pravastatin passes into the human breast milk. Biotransformation and elimination: Pravastatin is not significantly metabolised by cytochrome P450 nor does it appear to be a substrate or an inhibitor of P-glycoprotein but rather a substrate of other transport proteins. Following oral administration, 20% of the initial dose is eliminated in the urine and 70% in the faeces. Plasma elimination half-life of oral pravastatin is 1.5 to 2 hours. After intravenous administration, 47% of the dose is eliminated by the renal excretion and 53% by biliary excretion and biotransformation. The major degradation product of pravastatin is the 3-α- hydroxy isomeric metabolite. This metabolite has one-tenth to one-fortieth the HMG-CoA reductase inhibitor activity of the parent compound. The systemic clearance of pravastatin is 0.81 l/h/kg and the renal clearance is 0.38 l/h/kg indicating tubular secretion. Special populations Hepatic failure: Systemic exposure to pravastatin and metabolites in patients with alcoholic cirrhosis is enhanced by about 50% comparatively to patients with normal liver function. Renal impairment: No significant modifications were observed in patients with mild renal impairment. However severe and moderate renal insufficiency may lead to a two-fold increase of the systemic exposure to pravastatin and metabolites.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| 09/03/1999 | ליפידים | ATORVASTATIN, CERIVASTATIN, FLUVASTATIN, LOVASTATIN, PRAVASTATIN, SIMVASTATIN, ROSUVASTATIN | היפרליפידמיה |
שימוש לפי פנקס קופ''ח כללית 1994
Adjunct to dietary therapy to decrease elevated serum total and LDL cholesterol concentrations in primary hypercholesterolemia (types IIa and IIb) when the response to diet and other nonpharmacological methods has been inadequate. יירשם לפי פרוטוקול טיפולי מחייב
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
25.04.22 - עלון לצרכן אנגלית 25.04.22 - עלון לצרכן עברית 25.04.22 - עלון לצרכן ערבית 08.12.23 - עלון לצרכן אנגלית 08.12.23 - עלון לצרכן ערבית 10.12.23 - עלון לצרכן עברית 19.04.24 - עלון לצרכן עברית 12.07.24 - עלון לצרכן אנגלית 12.07.24 - עלון לצרכן עברית 12.07.24 - עלון לצרכן ערבית 26.11.20 - החמרה לעלון 20.02.22 - החמרה לעלון 09.03.16 - החמרה לעלון 08.12.23 - החמרה לעלון 19.04.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פרבסטאטין טבע 20 מ"ג