Quest for the right Drug
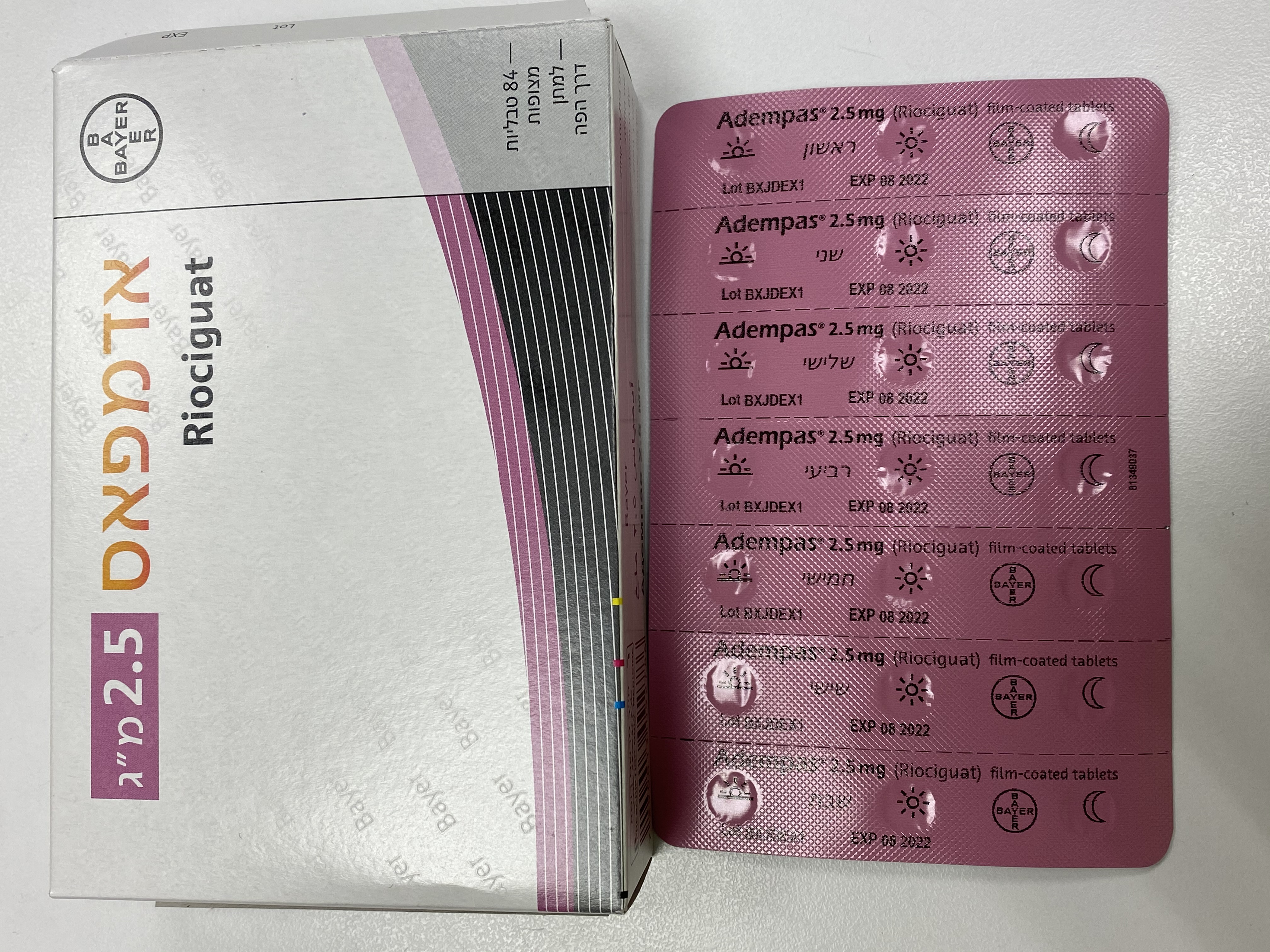
אדמפאס 2.5 מ"ג ADEMPAS 2.5 MG (RIOCIGUAT)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antihypertensives (antihypertensives for pulmonary arterial hypertension) ATC code: C02KX05 Mechanism of action Riociguat is a stimulator of soluble guanylate cyclase (sGC), an enzyme in the cardiopulmonary system and the receptor for nitric oxide (NO). When NO binds to sGC, the enzyme catalyses synthesis of the signalling molecule cyclic guanosine monophosphate (cGMP). Intra-cellular cGMP plays an important role in regulating processes that influence vascular tone, proliferation, fibrosis, and inflammation. Pulmonary hypertension is associated with endothelial dysfunction, impaired synthesis of NO and insufficient stimulation of the NO-sGC-cGMP pathway. Riociguat has a dual mode of action. It sensitises sGC to endogenous NO by stabilising the NO-sGC binding. Riociguat also directly stimulates sGC independently of NO. Riociguat restores the NO-sGC-cGMP pathway and leads to increased generation of cGMP. Pharmacodynamic effects Riociguat restores the NO-sGC-cGMP pathway resulting in a significant improvement of pulmonary vascular haemodynamics and an increase in exercise ability. There is a direct relationship between riociguat plasma concentration and haemodynamic parameters such as systemic and pulmonary vascular resistance, systolic blood pressure and cardiac output. Clinical efficacy and safety Efficacy in patients with CTEPH A randomised, double-blind, multi-national, placebo controlled, phase III study (CHEST-1) was conducted in 261 adult patients with inoperable chronic thromboembolic pulmonary hypertension (CTEPH) (72%) or persistent or recurrent CTEPH after pulmonary endarterectomy (PEA; 28%). During the first 8 weeks riociguat was titrated every 2-weeks based on the patient’s systolic blood pressure and signs or symptoms of hypotension to the optimal individual dose (range 0.5 mg to 2.5 mg three times daily) which was then maintained for a further 8 weeks. The primary endpoint of the study was the placebo adjusted change from baseline in 6-minute walk distance (6MWD) at the last visit (week 16). At the last visit, the increase in 6MWD in patients treated with riociguat was 46 m (95% confidence interval (CI): 25 m to 67 m; p<0.0001), compared to placebo. Results were consistent in the main sub-groups evaluated (ITT analysis, see table 2). Table 2: Effects of riociguat on 6MWD in CHEST-1 at last visit Entire patient population Riociguat Placebo (n=173) (n=88) Baseline (m) 342 356 [SD] [82] [75] Mean change from baseline (m) 39 -6 [SD] [79] [84] Placebo-adjusted difference (m) 46 95% CI, [p-value] 25 to 67 [<0.0001] FC III patient population Riociguat Placebo (n=107) (n=60) Baseline (m) 326 345 [SD] [81] [73] Mean change from baseline (m) 38 -17 [SD] [75] [95] Placebo-adjusted difference (m) 56 95% CI 29 to 83 FC II patient population Riociguat Placebo (n=55) (n=25) Baseline (m) 387 386 [SD] [59] [64] Mean change from baseline (m) 45 20 [SD] [82] [51] Placebo-adjusted difference (m) 25 95% CI -10 to 61 Inoperable patient population Riociguat Placebo (n=121) (n=68) Baseline (m) 335 351 [SD] [83] [75] Mean change from baseline (m) 44 -8 [SD] [84] [88] Placebo-adjusted difference (m) 54 95% CI 29 to 79 Patient population with CTEPH Riociguat Placebo post-PEA (n=52) (n=20) Baseline (m) 360 374 [SD] [78] [72] Mean change from baseline (m) 27 1.8 [SD] [68] [73] Placebo- adjusted difference (m) 27 95% CI -10 to 63 Improvement in exercise capacity was accompanied by improvement in multiple clinically relevant secondary endpoints. These findings were in accordance with improvements in additional haemodynamic parameters. Table 3: Effects of riociguat in CHEST-1 on PVR, NT-proBNP and WHO functional class at last visit Riociguat Placebo PVR (n=151) (n=82) Baseline 790.7 779.3 (dyn·s·cm-5) [SD] [431.6] [400.9] Mean change from baseline -225.7 23.1 (dyn·s·cm-5) [SD] [247.5] [273.5] Placebo-adjusted difference -246.4 (dyn·s·cm-5) 95% CI, [p-value] –303.3 to –189.5 [<0.0001] NT-proBNP Riociguat Placebo (n=150) (n=73) Baseline (ng/L) 1508.3 1705.8 [SD] [2337.8] [2567.2] Mean change from baseline (ng/L) -290.7 76.4 [SD] [1716.9] [1446.6] Placebo-adjusted difference (ng/L) -444.0 95% CI, [p-value] -843.0 to -45.0 [<0.0001] Change in WHO Functional Class Riociguat Placebo (n=173) (n=87) Improved 57 (32.9%) 13 (14.9%) Stable 107 (61.8%) 68 (78.2%) Deteriorated 9 (5.2%) 6 (6.9%) p-value 0.0026 PVR= pulmonary vascular resistance Adverse Events leading to discontinuation occurred at a similar frequency in both treatment groups (riociguat individual dose titration (IDT) 1.0-2.5 mg, 2.9%; placebo, 2.3%). Long-term treatment of CTEPH An open-label extension study (CHEST-2) included 237 patients who had completed CHEST-1. At the end of the study, mean (SD) treatment duration in the total group was 1285 (709) days and median duration was 1174 days (ranging from15 to 3512 days). In total, 221 patients (93.2%) had a treatment duration of approximately 1 year (at least 48 weeks), 205 patients (86.5%) of approximately 2 years (at least 96 weeks) and 142 patients (59.9%) of approximately 3 years (at least 144 weeks). Treatment exposure was 834 person years in total. The safety profile in CHEST-2 was similar to that observed in pivotal trials. After treatment with riociguat, the mean 6MWD improved in the overall population by 53 m at 12 months (n=208), 48 m at 24 months (n=182), and 49 m at 36 months (n=117) compared to baseline. Improvements in 6MWD persisted until the end of the study. Table 4 shows the proportion of patients* with changes in WHO functional class during riociguat treatment compared to baseline. Table 4: CHEST-2: Changes in WHO Functional Class Changes in WHO Functional Class (n (%) of patients) Treatment duration in Improved Stable Worsened CHEST-2 1 years (n=217) 100 (46%) 109 (50%) 6 (3%) 2 years (n=193) 76 (39%) 111 (58%) 5 (3%) 3 years (n=128) 48 (38%) 65 (51%) 14 (11%) *Patients participated in the study until the drug was approved and commercially available in their countries. The probability of survival was 97% after 1 year, 93% after 2 years and 89% after 3 years of riociguat treatment. Efficacy in patients with PAH A randomised, double-blind, multi-national, placebo controlled, phase III study (PATENT-1) was conducted in 443 adult patients with PAH (riociguat individual dose titration up to 2.5 mg three times daily: n=254, placebo: n=126, riociguat “capped” dose titration (CT) up to 1.5 mg (exploratory dose arm, no statistical testing performed; n=63)). Patients were either treatment-naïve (50%) or pre-treated with ERA (43%) or a prostacyclin analogue (inhaled (iloprost), oral (beraprost) or subcutaneous (treprostinil); 7%) and had been diagnosed with idiopathic or heritable PAH (63.4%), PAH associated with connective tissue disease (25.1%) and congenital heart disease (7.9%). During the first 8 weeks riociguat was titrated every 2-weeks based on the patient’s systolic blood pressure and signs or symptoms of hypotension to the optimal individual dose (range 0.5 mg to 2.5 mg three times daily), which was then maintained for a further 4 weeks. The primary endpoint of the study was placebo- adjusted change from baseline in 6MWD at the last visit (week 12). At the last visit the increase in 6MWD with riociguat individual dose titration (IDT) was 36 m (95% CI: 20 m to 52 m; p0.0001) compared to placebo. Treatment-naïve patients (n=189) improved by 38 m, and pre-treated patients (n=191) by 36 m (ITT analysis, see table 5). Further exploratory subgroup analysis revealed a treatment effect of 26 m, (95% CI: 5 m to 46 m) in patients pre-treated with ERAs (n=167) and a treatment effect of 101 m (95% CI: 27 m to 176 m) in patients pre-treated with prostacyclin analogues (n=27). Table 5 : Effects of riociguat on 6MWD in PATENT-1 at last visit Entire patient population Riociguat IDT Placebo Riociguat CT (n=254) (n=126) (n=63) Baseline (m) 361 368 363 [SD] [68] [75] [67] Mean change from baseline 30 -6 31 (m) [SD] [66] [86] [79] Placebo-adjusted difference 36 (m) 95% CI, [p-value] 20 to 52 [<0.0001] FC III patients Riociguat IDT Placebo Riociguat CT (n=140) (n=58) (n=39) Baseline (m) 338 347 351 [SD] [70] [78] [68] Mean change from baseline 31 -27 29 (m) [SD] [64] [98] [94] Placebo-adjusted difference 58 (m) 95% CI 35 to 81 FC II patients Riociguat IDT Placebo Riociguat CT (n=108) (n=60) (n=19) Baseline (m) 392 393 378 [SD] [51] [61] [64] Mean change from baseline 29 19 43 (m) [SD] [69] [63] [50] Placebo-adjusted difference 10 (m) 95% CI -11 to 31 Treatment-naïve patient Riociguat IDT Placebo Riociguat CT population (n=123) (n=66) (n=32) Baseline (m) 370 360 347 [SD] [66] [80] [72] Mean change from baseline 32 -6 49 (m) [SD] [74] [88] [47] Placebo-adjusted difference 38 (m) 14 to 62 95% CI Pre-treated patient Riociguat IDT Placebo Riociguat CT population (n=131) (n=60) (n=31) Baseline (m) 353 376 380 [SD] [69] [68] [57] Mean change from baseline 27 -5 12 (m) [SD] [58] [83] [100] Placebo- adjusted difference 36 (m) 15 to 56 95% CI Improvement in exercise capacity was accompanied by consistent improvement in multiple clinically-relevant secondary endpoints. These findings were in accordance with improvements in additional haemodynamic parameters (see table 6). Table 6: Effects of riociguat in PATENT-1 on PVR and NT-proBNP at last visit Riociguat IDT Placebo Riociguat CT PVR (n=232) (n=107) (n=58) Baseline 791 834.1 847.8 (dyn·s·cm-5) [SD] [452.6] [476.7] [548.2] Mean change from PVR baseline -223 -8.9 -167.8 (dyn·s·cm-5) [SD] [260.1] [316.6] [320.2] Placebo-adjusted difference -225.7 (dyn·s·cm-5) 95% CI, [p-value] -281.4 to -170.1[<0.0001] NT-proBNP Riociguat IDT Placebo Riociguat CT (n = 228) (n = 106) (n=54) Baseline (ng/L) 1,026.7 1,228.1 1,189.7 [SD] [1,799.2] [1,774.9] [1,404.7] Mean change from baseline (ng/L) -197.9 232.4 -471.5 [SD] [1721.3] [1011.1] [913.0] Placebo-adjusted difference (ng/L) -431.8 95% CI, [p-value] -781.5 to -82.1 [<0.0001] Change in WHO Functional Riociguat IDT Placebo Riociguat CT Class (n = 254) (n = 125) (n=63) Improved 53 (20.9%) 18 (14.4%) 15 (23.8%) Stable 192 (75.6%) 89 (71.2%) 43 (68.3%) Deteriorated 9 (3.6%) 18 (14.4%) 5 (7.9%) p-value 0.0033 Riociguat-treated patients experienced a significant delay in time to clinical worsening versus placebo-treated patients (p = 0.0046; Stratified log-rank test) (see table 7). Table 7: Effects of riociguat in PATENT-1 on events of clinical worsening Clinical Worsening Events Riociguat IDT Placebo Riociguat CT (n=254) (n=126) (n=63) Patients with any clinical worsening 3 (1.2%) 8 (6.3%) 2 (3.2%) Death 2 (0.8%) 3 (2.4%) 1 (1.6%) Hospitalisations due to PH 1 (0.4%) 4 (3.2%) 0 Decrease in 6MWD due to PH 1 (0.4%) 2 (1.6%) 1 (1.6%) Persistent worsening of Functional 0 1 (0.8%) 0 Class due to PH Start of new PH treatment 1 (0.4%) 5 (4.0%) 1 (1.6%) Patients treated with riociguat showed significant improvement in Borg CR 10 dyspnoea score (mean change from baseline (SD): riociguat -0.4 (2), placebo 0.1 (2); p = 0.0022). Adverse Events leading to discontinuation occurred less frequently in both riociguat treatment groups than in the placebo group (riociguat IDT 1.0-2.5 mg, 3.1%; riociguat CT 1.6%; placebo, 7.1%). Long-term treatment of PAH An open label extension study (PATENT-2) included 396 patients who had completed PATENT-1. In PATENT-2, mean (SD) treatment duration in the total group (not including exposure in PATENT-1) was 1375 (772) days and median duration was 1331 days (ranging from 1 to 3565 days). In total, treatment exposure was approximately 1 year (at least 48 weeks) for 90%, 2 years (at least 96 weeks) for 85%, and 3 years (at least 144 weeks) for 70% of patients. Treatment exposure was 1491 person years in total. The safety profile in PATENT-2 was similar to that observed in pivotal trials. After treatment with riociguat, the mean 6MWD improved in the overall population by 50 m at 12 months (n=347), 46 m at 24 months (n=311) and 46 m at 36 months (n=238) compared to baseline. Improvements in 6MWD persisted until the end of the study. Table 8 shows the proportion of patients* with changes in WHO functional class during riociguat treatment compared to baseline. Table 8: PATENT-2: Changes in WHO Functional Class Changes in WHO Functional Class (n(%) of patients) Treatment duration in PATENT- Improved Stable Worsened 2 1 years (n=358) 116 (32%) 222 (62%) 20 (6%) 2 years (n=321) 106 (33%) 189 (59%) 26 (8%) 3 years (n=257) 88 (34%) 147 (57%) 22 (9%) *Patients participated in the study until the study drug was approved and commercially available in their countries. The probability of survival was 97% after 1 year, 93% after 2 years and 88% after 3 years of riociguat treatment. Patients with pulmonary hypertension associated with idiopathic interstitial pneumonias (PH-IIP): A randomised, double blind, placebo-controlled phase II study (RISE-IIP) to evaluate the efficacy and safety of riociguat in patients with symptomatic pulmonary hypertension associated with idiopathic interstitial pneumonias (PH-IIP) was terminated early due to an increased risk of mortality and serious adverse events in in patients treated with riociguat and a lack of efficacy More patients taking riociguat died (11% vs. 4%) and had serious adverse events (37% vs. 23%) during the main phase. In the long-term extension, more patients who switched from the placebo group to riociguat (21%) died than those who continued in the riociguat group (3%). Riociguat is therefore contraindicated in patients with pulmonary hypertension associated with idiopathic interstitial pneumonias (see section 4.3). Paediatric population The European Medicines Agency has deferred the obligation to submit the results of studies with riociguat in one or more subsets of the paediatric population in the treatment of pulmonary hypertension. See section 4.2 for information on paediatric use.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption The absolute bioavailability of riociguat is high (94%). Riociguat is rapidly absorbed with maximum concentrations (Cmax) appearing 1-1.5 hours after tablet intake. Intake with food reduced riociguat AUC slightly, Cmax was reduced by 35%. Bioavailability (AUC and Cmax) is comparable for riociguatadministered orally as a crushed tablet suspended in apple sauce or in water compared to a whole tablet (see section 4.2). Distribution Plasma protein binding in humans is high at approximately 95%, with serum albumin and alpha 1-acidic glycoprotein being the main binding components. The volume of distribution is moderate with volume of distribution at steady state being approximately 30 L. Biotransformation N-demethylation, catalysed by CYP1A1, CYP3A4, CYP3A5 and CYP2J2 is the major biotransformation pathway of riociguat leading to its major circulating active metabolite M-1 (pharmacological activity: 1/10th to 1/3rd of riociguat) which is further metabolised to the pharmacologically inactive N-glucuronide. CYP1A1 catalyses the formation of riociguat’s main metabolite in liver and lungs and is known to be inducible by polycyclic aromatic hydrocarbons, which, for example, are present in cigarette smoke. Elimination Total riociguat (parent compound and metabolites) is excreted via both renal (33-45%) and biliary/faecal routes (48-59%). Approximately 4-19% of the administered dose was excreted as unchanged riociguat via the kidneys. Approximately 9-44% of the administered dose was found as unchanged riociguat in faeces. Based on in vitro data riociguat and its main metabolite are substrates of the transporter proteins P-gp (P- glycoprotein) and BCRP (breast cancer resistance protein). With a systemic clearance of about 3-6 L/h, riociguat can be classified as a low-clearance drug. Elimination half-life is about 7 hours in healthy subjects and about 12 hours in patients. Linearity Riociguat pharmacokinetics are linear from 0.5 to 2.5 mg. Inter-individual variability (CV) of riociguat exposure (AUC) across all doses is approximately 60%. Special populations Gender Pharmacokinetic data reveal no relevant differences due to gender in the exposure to riociguat. Paediatric population No studies have been conducted to investigate the pharmacokinetics of riociguat in paediatric patients. Elderly population Elderly patients (65 years or older) exhibited higher plasma concentrations than younger patients, with mean AUC values being approximately 40% higher in elderly, mainly due to reduced (apparent) total and renal clearance. Inter-ethnic differences Pharmacokinetic data reveal no relevant inter-ethnic differences. Different weight categories Pharmacokinetic data reveal no relevant differences due to weight in the exposure to riociguat. Hepatic impairment In cirrhotic patients (non-smokers) with mild hepatic impairment (classified as Child Pugh A) riociguat mean AUC was increased by 35% compared to healthy controls, which is within normal intra-individual variability. In cirrhotic patients (non-smokers) with moderate hepatic impairment (classified as Child Pugh B), riociguat mean AUC was increased by 51% compared to healthy controls. There are no data in patients with severe hepatic impairment (classified as Child Pugh C). Patients with ALT > 3 x ULN and bilirubin > 2 x ULN were not studied (see section 4.4). Renal impairment Overall, mean dose- and weight- normalised exposure values for riociguat were higher in subjects with renal impairment compared to subjects with normal renal function. Corresponding values for the main metabolite were higher in subjects with renal impairment compared to healthy subjects. In non-smoking individuals with mild (creatinine clearance 80-50 mL/min), moderate (creatinine clearance <50-30 mL/min) or severe (creatinine clearance <30 mL/min) renal impairment, riociguat plasma concentrations (AUC) were increased by 53%, 139% or 54%, respectively. Data in patients with creatinine clearance <30 mL/min are limited and there are no data for patients on dialysis. Due to the high plasma protein binding riociguat is not expected to be dialysable.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול ביתר לחץ דם ריאתי כרוני תרומבואמבולי - CTEPH (Chronic Thromboembolic Pulmonary Hypertension) בחולים בדרגת תפקוד II או III לפי ה-WHO, שמחלתם אינה מתאימה לטיפול באמצעות התערבות כירורגית או שמחלתם לא הגיבה או חזרה לאחר ההתערבות הכירורגית.ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה או קרדיולוגיה ילדים או רפואת ריאות או רפואת ריאות ילדים.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
11/01/2018
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
