Quest for the right Drug
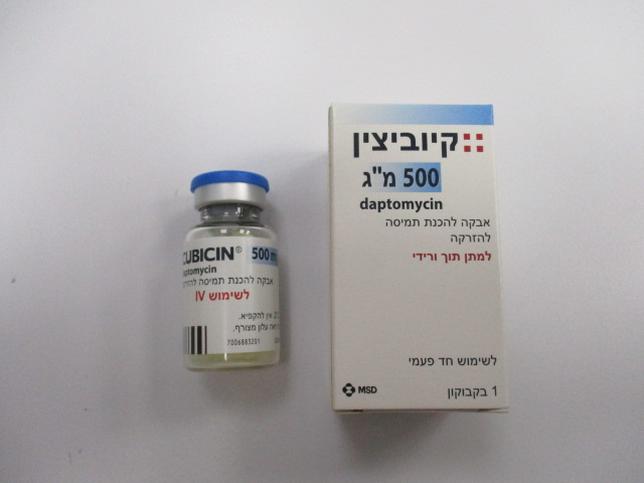
קיוביצין 500 מ"ג CUBICIN 500 MG (DAPTOMYCIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה מיובשת בהקפאה להכנת תמיסה להזרקה : LYOPHILIZED POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Anaphylaxis/Hypersensitivity Reactions Anaphylaxis/hypersensitivity reactions have been reported with the use of antibacterial agents, including CUBICIN, and may be life-threatening. If an allergic reaction to CUBICIN occurs, discontinue the drug and institute appropriate therapy [see Adverse Reactions (6.2)]. 5.2 Myopathy and Rhabdomyolysis Myopathy, defined as muscle aching or muscle weakness in conjunction with increases in creatine phosphokinase (CPK) values to greater than 10 times the upper limit of normal (ULN), has been reported with the use of CUBICIN. Rhabdomyolysis, with or without acute renal failure, has been reported [see Adverse Reactions (6.2)]. Patients receiving CUBICIN should be monitored for the development of muscle pain or weakness, particularly of the distal extremities. In patients who receive CUBICIN, CPK levels should be monitored weekly, and more frequently in patients who received recent prior or concomitant therapy with an HMG-CoA reductase inhibitor or in whom elevations in CPK occur during treatment with CUBICIN. In adult patients with renal impairment, both renal function and CPK should be monitored more frequently than once weekly [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. In Phase 1 studies and Phase 2 clinical trials in adults, CPK elevations appeared to be more frequent when CUBICIN was dosed more than once daily. Therefore, CUBICIN should not be dosed more frequently than once a day. CUBICIN should be discontinued in patients with unexplained signs and symptoms of myopathy in conjunction with CPK elevations to levels >1,000 U/L (~5× ULN), and in patients without reported symptoms who have marked elevations in CPK, with levels >2,000 U/L (≥10× ULN). In addition, consideration should be given to suspending agents associated with rhabdomyolysis, such as HMG-CoA reductase inhibitors, temporarily in patients receiving CUBICIN [see Drug Interactions (7.1)]. 5.3 Eosinophilic Pneumonia Eosinophilic pneumonia has been reported in patients receiving CUBICIN [see Adverse Reactions (6.2)]. In reported cases associated with CUBICIN, patients developed fever, dyspnea with hypoxic respiratory insufficiency, and diffuse pulmonary infiltrates or organizing pneumonia. In general, patients developed eosinophilic pneumonia 2 to 4 weeks after starting CUBICIN and improved when CUBICIN was discontinued and steroid therapy was initiated. Recurrence of eosinophilic pneumonia upon re- exposure has been reported. Patients who develop these signs and symptoms while receiving CUBICIN should undergo prompt medical evaluation, and CUBICIN should be discontinued immediately. Treatment with systemic steroids is recommended. 5.4 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) DRESS has been reported in post-marketing experience with CUBICIN [see Adverse Reactions (6.2)]. Patients who develop skin rash, fever, peripheral eosinophilia, and systemic organ (for example, hepatic, renal, pulmonary) impairment while receiving CUBICIN should undergo medical evaluation. If DRESS is suspected, discontinue CUBICIN promptly and institute appropriate treatment. 5.5 Tubulointerstitial Nephritis (TIN) TIN has been reported in post-marketing experience with CUBICIN [see Adverse Reactions (6.2)]. Patients who develop new or worsening renal impairment while receiving CUBICIN should undergo medical evaluation. If TIN is suspected, discontinue CUBICIN promptly and institute appropriate treatment. 5.6 Peripheral Neuropathy Cases of peripheral neuropathy have been reported during the CUBICIN postmarketing experience [see Adverse Reactions (6.2)]. Therefore, physicians should be alert to signs and symptoms of peripheral neuropathy in patients receiving CUBICIN. Monitor for neuropathy and consider discontinuation. 5.7 Potential Nervous System and/or Muscular System Effects in Pediatric Patients Younger than 12 Months Avoid use of CUBICIN in pediatric patients younger than 12 months due to the risk of potential effects on muscular, neuromuscular, and/or nervous systems (either peripheral and/or central) observed in neonatal dogs with intravenous daptomycin [see Nonclinical Toxicology (13.2)]. 5.8 Clostridioides difficile–Associated Diarrhea Clostridioides difficile–associated diarrhea (CDAD) has been reported with the use of nearly all systemic antibacterial agents, including CUBICIN, and may range in severity from mild diarrhea to fatal colitis [see Adverse Reactions (6.2)]. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile. C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin- producing strains of C. difficile cause increased morbidity and mortality, since these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary because CDAD has been reported to occur more than 2 months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated. 5.9 Persisting or Relapsing S. aureus Bacteremia/Endocarditis Patients with persisting or relapsing S. aureus bacteremia/endocarditis or poor clinical response should have repeat blood cultures. If a blood culture is positive for S. aureus, minimum inhibitory concentration (MIC) susceptibility testing of the isolate should be performed using a standardized procedure, and diagnostic evaluation of the patient should be performed to rule out sequestered foci of infection. Appropriate surgical intervention (e.g., debridement, removal of prosthetic devices, valve replacement surgery) and/or consideration of a change in antibacterial regimen may be required. Failure of treatment due to persisting or relapsing S. aureus bacteremia/endocarditis may be due to reduced daptomycin susceptibility (as evidenced by increasing MIC of the S. aureus isolate) [see Clinical Studies (14.2)]. 5.10 Decreased Efficacy in Patients with Moderate Baseline Renal Impairment Limited data are available from the two Phase 3 complicated skin and skin structure infection (cSSSI) trials regarding clinical efficacy of CUBICIN treatment in adult patients with creatinine clearance (CLCR) <50 mL/min; only 31/534 (6%) patients treated with CUBICIN in the intent-to-treat (ITT) population had a baseline CLCR <50 mL/min. Table 2 shows the number of adult patients by renal function and treatment group who were clinical successes in the Phase 3 cSSSI trials. Table 2: Clinical Success Rates by Renal Function and Treatment Group in Phase 3 cSSSI Trials in Adult Patients (Population: ITT) Success Rate n/N (%) CLCR CUBICIN Comparator 4 mg/kg every 24h 50–70 mL/min 25/38 (66%) 30/48 (63%) 30–<50 mL/min 7/15 (47%) 20/35 (57%) In a subgroup analysis of the ITT population in the Phase 3 S. aureus bacteremia/endocarditis trial, clinical success rates, as determined by a treatment-blinded Adjudication Committee [see Clinical Studies (14.2)], in the CUBICIN-treated adult patients were lower in patients with baseline CLCR <50 mL/min (see Table 3). A decrease of the magnitude shown in Table 3 was not observed in comparator-treated patients. Table 3: Adjudication Committee Clinical Success Rates at Test of Cure by Baseline Creatinine Clearance and Treatment Subgroup in the S. aureus Bacteremia/Endocarditis Trial in Adult Patients (Population: ITT) Success Rate n/N (%) CUBICIN Baseline Comparator 6 mg/kg every 24h CLCR Right-Sided Right-Sided Bacteremia Infective Bacteremia Infective Endocarditis Endocarditis >80 mL/min 30/50 (60%) 7/14 (50%) 19/42 (45%) 5/11 (46%) 50–80 12/26 (46%) 1/4 (25%) 13/31 (42%) 1/2 (50%) mL/min 30–<50 2/14 (14%) 0/1 (0%) 7/17 (41%) 1/1 (100%) mL/min Consider these data when selecting antibacterial therapy for use in adult patients with baseline moderate to severe renal impairment. 5.11 Increased International Normalized Ratio (INR)/Prolonged Prothrombin Time Clinically relevant plasma concentrations of daptomycin have been observed to cause a significant concentration-dependent false prolongation of prothrombin time (PT) and elevation of International Normalized Ratio (INR) when certain recombinant thromboplastin reagents are utilized for the assay [see Drug Interactions (7.2)]. 5.12 Development of Drug-Resistant Bacteria Prescribing CUBICIN in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. 6 ADVERSE REACTIONS The following adverse reactions are described, or described in greater detail, in other sections: • Anaphylaxis/Hypersensitivity Reactions [see Warnings and Precautions (5.1)] • Myopathy and Rhabdomyolysis [see Warnings and Precautions (5.2)] • Eosinophilic Pneumonia [see Warnings and Precautions (5.3)] • Drug Reaction with Eosinophilia and Systemic Symptoms [see Warnings and Precautions (5.4)] • Tubulointerstitial Nephritis [see Warnings and Precautions (5.5)] • Peripheral Neuropathy [see Warnings and Precautions (5.6)] • Increased International Normalized Ratio (INR)/Prolonged Prothrombin Time [see Warnings and Precautions (5.11) and Drug Interactions (7.2)] 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice. Clinical trials enrolled 1,864 adult patients treated with CUBICIN and 1,416 treated with comparator. Complicated Skin and Skin Structure Infection Trials in Adults In Phase 3 complicated skin and skin structure infection (cSSSI) trials in adult patients, CUBICIN was discontinued in 15/534 (2.8%) patients due to an adverse reaction, while comparator was discontinued in 17/558 (3.0%) patients. The rates of the most common adverse reactions, organized by body system, observed in adult patients with cSSSI (receiving 4 mg/kg CUBICIN) are displayed in Table 4. Table 4: Incidence of Adverse Reactions that Occurred in ≥2% of Adult Patients in the CUBICIN Treatment Group and ≥ the Comparator Treatment Group in Phase 3 cSSSI Trials Adult Patients (%) Adverse Reaction CUBICIN 4 mg/kg Comparator* (N=534) (N=558) Gastrointestinal disorders Diarrhea 5.2 4.3 Nervous system disorders Headache 5.4 5.4 Dizziness 2.2 2.0 Skin/subcutaneous disorders Rash 4.3 3.8 Diagnostic investigations Abnormal liver function tests 3.0 1.6 Elevated CPK 2.8 1.8 Infections Urinary tract infections 2.4 0.5 Vascular disorders Hypotension 2.4 1.4 Respiratory disorders Dyspnea 2.1 1.6 *Comparator: vancomycin (1 g IV q12h) or an anti-staphylococcal semi-synthetic penicillin (i.e., nafcillin, oxacillin, cloxacillin, or flucloxacillin; 4 to 12 g/day IV in divided doses). Drug-related adverse reactions (possibly or probably drug-related) that occurred in <1% of adult patients receiving CUBICIN in the cSSSI trials are as follows: Body as a Whole: fatigue, weakness, rigors, flushing, hypersensitivity Blood/Lymphatic System: leukocytosis, thrombocytopenia, thrombocytosis, eosinophilia, increased International Normalized Ratio (INR) Cardiovascular System: supraventricular arrhythmia Dermatologic System: eczema Digestive System: abdominal distension, stomatitis, jaundice, increased serum lactate dehydrogenase Metabolic/Nutritional System: hypomagnesemia, increased serum bicarbonate, electrolyte disturbance Musculoskeletal System: myalgia, muscle cramps, muscle weakness, arthralgia Nervous System: vertigo, mental status change, paresthesia Special Senses: taste disturbance, eye irritation S. aureus Bacteremia/Endocarditis Trial in Adults In the S. aureus bacteremia/endocarditis trial involving adult patients, CUBICIN was discontinued in 20/120 (16.7%) patients due to an adverse reaction, while comparator was discontinued in 21/116 (18.1%) patients. Serious Gram-negative infections (including bloodstream infections) were reported in 10/120 (8.3%) CUBICIN-treated patients and 0/115 comparator-treated patients. Comparator-treated patients received dual therapy that included initial gentamicin for 4 days. Infections were reported during treatment and during early and late follow-up. Gram-negative infections included cholangitis, alcoholic pancreatitis, sternal osteomyelitis/mediastinitis, bowel infarction, recurrent Crohn’s disease, recurrent line sepsis, and recurrent urosepsis caused by a number of different Gram -negative bacteria. The rates of the most common adverse reactions, organized by System Organ Class (SOC), observed in adult patients with S. aureus bacteremia/endocarditis (receiving 6 mg/kg CUBICIN) are displayed in Table 5. Table 5: Incidence of Adverse Reactions that Occurred in ≥5% of Adult Patients in the CUBICIN Treatment Group and ≥ the Comparator Treatment Group in the S. aureus Bacteremia/Endocarditis Trial Adult Patients n (%) Adverse Reaction* CUBICIN 6 mg/kg Comparator† (N=120) (N=116) Infections and infestations Sepsis NOS 6 (5%) 3 (3%) Adult Patients n (%) Adverse Reaction* CUBICIN 6 mg/kg Comparator† (N=120) (N=116) Bacteremia 6 (5%) 0 (0%) Gastrointestinal disorders Abdominal pain NOS 7 (6%) 4 (3%) General disorders and administration site conditions Chest pain 8 (7%) 7 (6%) Edema NOS 8 (7%) 5 (4%) Respiratory, thoracic and mediastinal disorders Pharyngolaryngeal pain 10 (8%) 2 (2%) Skin and subcutaneous tissue disorders Pruritus 7 (6%) 6 (5%) Sweating increased 6 (5%) 0 (0%) Psychiatric disorders Insomnia 11 (9%) 8 (7%) Investigations Blood creatine phosphokinase increased 8 (7%) 1 (1%) Vascular disorders Hypertension NOS 7 (6%) 3 (3%) *NOS, not otherwise specified. †Comparator: vancomycin (1 g IV q12h) or an anti-staphylococcal semi-synthetic penicillin (i.e., nafcillin, oxacillin, cloxacillin, or flucloxacillin; 2 g IV q4h), each with initial low-dose gentamicin. The following reactions, not included above, were reported as possibly or probably drug-related in the CUBICIN-treated group: Blood and Lymphatic System Disorders: eosinophilia, lymphadenopathy, thrombocythemia, thrombocytopenia Cardiac Disorders: atrial fibrillation, atrial flutter, cardiac arrest Ear and Labyrinth Disorders: tinnitus Eye Disorders: vision blurred Gastrointestinal Disorders: dry mouth, epigastric discomfort, gingival pain, hypoesthesia oral Infections and Infestations: candidal infection NOS, vaginal candidiasis, fungemia, oral candidiasis, urinary tract infection fungal Investigations: blood phosphorous increased, blood alkaline phosphatase increased, INR increased, liver function test abnormal, alanine aminotransferase increased, aspartate aminotransferase increased, prothrombin time prolonged Metabolism and Nutrition Disorders: appetite decreased NOS Musculoskeletal and Connective Tissue Disorders: myalgia Nervous System Disorders: dyskinesia, paresthesia Psychiatric Disorders: hallucination NOS Renal and Urinary Disorders: proteinuria, renal impairment NOS Skin and Subcutaneous Tissue Disorders: pruritus generalized, rash vesicular Other Trials in Adults In Phase 3 trials of community-acquired pneumonia (CAP) in adult patients, the death rate and rates of serious cardiorespiratory adverse events were higher in CUBICIN-treated patients than in comparator- treated patients. These differences were due to lack of therapeutic effectiveness of CUBICIN in the treatment of CAP in patients experiencing these adverse events [see Indications and Usage (1.3)]. Laboratory Changes in Adults Complicated Skin and Skin Structure Infection Trials in Adults In Phase 3 cSSSI trials of adult patients receiving CUBICIN at a dose of 4 mg/kg, elevations in CPK were reported as clinical adverse events in 15/534 (2.8%) CUBICIN-treated patients, compared with 10/558 (1.8%) comparator-treated patients. Of the 534 patients treated with CUBICIN, 1 (0.2%) had symptoms of muscle pain or weakness associated with CPK elevations to greater than 4 times the upper limit of normal (ULN). The symptoms resolved within 3 days and CPK returned to normal within 7 to 10 days after treatment was discontinued [see Warnings and Precautions (5.2)]. Table 6 summarizes the CPK shifts from Baseline through End of Therapy in the cSSSI adult trials. Table 6: Incidence of CPK Elevations from Baseline during Therapy in Either the CUBICIN Treatment Group or the Comparator Treatment Group in Phase 3 cSSSI Adult Trials Adult Patients with All Adult Patients Normal CPK at Baseline CUBICIN CUBICIN Change in CPK 4 mg/kg Comparator* 4 mg/kg Comparator* (N=430) (N=459) (N=374) (N=392) % n % n % n % n No Increase 90.7 390 91.1 418 91.2 341 91.1 357 † Maximum Value >1× ULN 9.3 40 8.9 41 8.8 33 8.9 35 >2× ULN 4.9 21 4.8 22 3.7 14 3.1 12 >4× ULN 1.4 6 1.5 7 1.1 4 1.0 4 >5× ULN 1.4 6 0.4 2 1.1 4 0.0 0 >10× ULN 0.5 2 0.2 1 0.2 1 0.0 0 Note: Elevations in CPK observed in adult patients treated with CUBICIN or comparator were not clinically or statistically significantly different. *Comparator: vancomycin (1 g IV q12h) or an anti-staphylococcal semi-synthetic penicillin (i.e., nafcillin, oxacillin, cloxacillin, or flucloxacillin; 4 to 12 g/day IV in divided doses). †ULN (Upper Limit of Normal) is defined as 200 U/L. S. aureus Bacteremia/Endocarditis Trial in Adults In the S. aureus bacteremia/endocarditis trial in adult patients, at a dose of 6 mg/kg, 11/120 (9.2%) CUBICIN-treated patients, including two patients with baseline CPK levels >500 U/L, had CPK elevations to levels >500 U/L, compared with 1/116 (0.9%) comparator-treated patients. Of the 11 CUBICIN-treated patients, 4 had prior or concomitant treatment with an HMG-CoA reductase inhibitor. Three of these 11 CUBICIN-treated patients discontinued therapy due to CPK elevation, while the one comparator-treated patient did not discontinue therapy [see Warnings and Precautions (5.2)]. 6.2 Post-Marketing Experience The following adverse reactions have been identified during post-approval use of CUBICIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Blood and lymphatic system disorders: anemia, thrombocytopenia General and administration site conditions: pyrexia Immune System Disorders: anaphylaxis; hypersensitivity reactions, including angioedema, pruritus, hives, shortness of breath, difficulty swallowing, truncal erythema, and pulmonary eosinophilia [see Contraindications (4) and Warnings and Precautions (5.1)] Infections and Infestations: Clostridioides difficile–associated diarrhea [see Warnings and Precautions (5.8)] Laboratory Investigations: platelet count decreased Musculoskeletal Disorders: myoglobin increased; rhabdomyolysis (some reports involved patients treated concurrently with CUBICIN and HMG-CoA reductase inhibitors) [see Warnings and Precautions (5.2), Drug Interactions (7.1), and Clinical Pharmacology (12.3)] Respiratory, Thoracic, and Mediastinal Disorders: cough, eosinophilic pneumonia, organizing pneumonia [see Warnings and Precautions (5.3)] Nervous System Disorders: peripheral neuropathy [see Warnings and Precautions (5.6)] Skin and Subcutaneous Tissue Disorders: serious skin reactions, including drug reaction with eosinophilia and systemic symptoms (DRESS), vesiculobullous rash (with or without mucous membrane involvement, including Stevens-Johnson syndrome [SJS] and toxic epidermal necrolysis [TEN]), and acute generalized exanthematous pustulosis [see Warnings and Precautions (5.4)] Gastrointestinal Disorders: nausea, vomiting Renal and urinary disorders: acute kidney injury, renal insufficiency, renal failure, and tubulointerstitial nephritis (TIN) [see Warnings and Precautions (5.5)] Special Senses: visual disturbances Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
רישום
131 21 30994 01
מחיר
0 ₪
מידע נוסף
